Asthma Flashcards
Asthma epidemiology
5-10% of population Increasing Can be fatal
Asthma definitions
Defined as reversible increases in airway resistance, involving bronchi construction and inflammation.
Asthma spirometry characterisations
Reversible decreases in the FEV1:FVC (less than 70-80% suggests increased airway resistance ). Variations in PEF, which improve with a beta-2 agonist (+morning dipping).
Control of bronchial calibre - PARASYMPATHETIC (3)
ACh acts on M3 (muscarinic) receptors Bronchoconstriction Increase mucus
Control of bronchial calibre - SYMPATHETIC (3)
Circulating adrenaline acting on beta-2 adrenoceptors on bronchial smooth muscle to cause relaxation. Plus sympathetic fibres releasing NA acting on beta-2 adrenoceptors on parasympathetic ganglia to inhibit transmission. Beta-2 adrenoceptors also on mucus glands to inhibit secretion.
Asthmatic attack, provoking factors (5)
Allergens Cold air Viral infections Smoking Exercise
Asthmatic attacks, phases
May be characterised by early (immediate) phase followed by late phase. Sometimes just one or the other.
Asthma - Clinical features
Wheezing Breathlessness Tight chest Cough (worse at night/ exercise) Decreases in FEV1 (reversed by beta-2 agonist)
Asthmatic attack, method of action
Pic
Asthmatic attack, graph
Pic
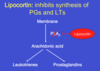
Asthma, Spasmogens
Histamine Prostaglandin, D2 Leukotrienes (C4 & D4) Platelet activating factor (PAF) See pic
Asthma, Chemotaxins & role
Leukotriene B4, PAF Lead to late phase Attract leukocytes, esp eosinophils and mononuclear cells Leading to inflammation and airway hyper-reactivity
Pharmacological management of Asthma - Principles (2)
BRONCHODILATORS Reverse bronchospasm (early phase) Rapid relief (“relievers”) PREVENTION Used to prevent an attack May be anti-inflammatory “Preventers”
Beta-2 adrenoceptor agonists - examples & action
E.g. Salbutamol (ventolin) First choice agents Increased FEV1 Act on beta-2 adrenoceptors on smooth muscle to increase cAMP
Salbutamol Action
Pic