Anterior Abdominal Wall Flashcards
What is the location of the abodminal wall?
The abdominal wall is located between the xiphoid process / costal margin and the pelvis

The pelvic bones are formed by the fusion of what three bones?
The pelvic bones are formed by the fusion of:
- Ilium
- Pubis
- Ischium

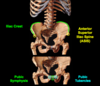
What are the landmarks on ilium and pubis?
Landmarks on the ilium:
- Iliac crest (at L4 vertebral level)
- Anterior superior iliac spine (ASIS)
Landmarks on the pubis:
- Pubic symphysis (at the midline where the two pubic bones meet)
- Pubric tubercles (prominances lateral to public symysis)
Umbilicus
- What is it?
- Where is it located (on a person with low body fat)?
Umbilicus
- Former site of attachment of umbilical cord
- Location varies with age and body contours
- In a person with low body fat, the umbilicus lies at L4 vertebral level and is midway between the xiphoid process and public symphysis
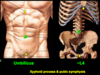
What are the abdominal planes and where do they pass through? What do two these planes form?
Transumbilical plane - passes horizontally through the umbilicus at L4 vertebral level (corresponding to level of the iliac crests)
Median plane - pass vertically through the body midline, from the xiphoid process to the pubic sympysis
The transumbilical plane and median plane form the four abdominal quadrants:
- Right upper
- Left upper
- Right lower
- Left lower
Transpyloric plane - passes through the L1 vertebral level

Abdominal fascia
What are the three layers of the abdominal fascia and where are they located?
Abdominal fasica
Superficial fascia
- Inferior to umbilicus, there are two layers
- Superficial fatty layer / Camper fascia
- Deep membranous layer / Scarpa fascia - this layer limits the spread of abdominal wall infections inferiorly into the thigh because it firmly attaches to the iliac crest, inguinal ligament, and public sympysis
- Superior to the umbilicus, there is only one layer
Deep investing fascia - surrounds the muscles of the abdominal wall
Transversalis fascia - located between the deep surface of the transverse abdominal muscle and parietal peritoneum

Scrotum fascia layers
- What is the superficial layer?
- What is the deep layer?
- What is the deep layer continuous with?
Scrotum fascia layers
Superficial layer - skin
Deep layer - specialized fascia (dartos fascia and dartos muscle)
Dartos fascia
- Contains no fat
- Continuous with the scarpa layer of the abdominal wall
- Due to this connection, infections / fluids from the abdominal wall can collect in the scrotum
Dartos muscle
- Smooth muscle fibers
- Contracts in response to cold, giving the skin a wrinkled appearance and helping reduce heat loss by reducing surface area

Labia majora fascia
- What is this fascia continuous with?
- What is the significance of this continuous in regards with infection?
Labia majora fascia
Fascia is continuous with the Scarpa layer (same as scrotum)
Infection / fluid can collect in labia majora due to this connection

What are the functions of the abdominal muscles?
Functions of the abdominal muscles
- Maintain posture and control movements of the torso
- Protect abdominal organs
- Active during forced expiration
- Decrease volume of abdominal cavity, thus increasing abdominal pressure, which is necessary for micturition (urination) and parturition (childbirth)
What are the three layers of the abdominal muscles?
Three main layers of abdominal muscle from superficial to deep:
- External oblique and aponeurosis
- Internal oblique and aponeurosis
- Transverse abdominis and aponeurosis

Rectus abdominis
- Where is it located?
- What causes the 6 pack look?
- What is it enclosed by?
Rectus abdominis
- Located on either side of the midline
- Belly is interupted by tendinous intersections, which causes 6 pack appearance
- Enclosed by the rectus sheath

Rectus sheath
- What forms the rectus sheath?
- Where is the linea alba and what is it formed by?
- Where is the arcuate line? Describe the transition is marks
Rectus sheath
- Formed by aponeuroses of external and internal obliques and transversus abdominus
- Linea alba - runs vertically in midline and is formed by the fibers of the rectus sheath fusing in the midline
-
Arcuate line - 1/3 the distance between the umbilicus and pubis and marks the transition in composition of rectus sheath
- Superior to arcuate line - aponeurosis of internal oblique splits to enclose the rectus abdominis
- Inferior to arcuate line - all three aponeurotic layers (external, internal, and transversus) pass anterior to the rectus abfominis, leaving only the transversalis fascia deep to the rectus abdominis

Nerves of the abdominal wall
- Skin and muscle are innervated by the ventral rami of which nerves?
- What is the significance of nerves innervating muscle layers of the abdominal wall segmentally?
Skin and muscles are innervated by the ventral rami of:
- T7 - T11 (intercostal nerves)
- T12 (subcostal nerve)
- L1 (iliohypogastric and ilioinguinal nerves)
Innervate muscle layers of the abdominal wall segmentally as they pass through them to reach the skin. Thus, injury to a single nerve would not paralyze an entire muscle, only a segement of it. The paralyzed portion however could create a weakend area in the abdominal contents to protrude or herniate.

Describe where the dermatomes of the abdominal wall are
Dermatomes of the abdominal wall:
- T7 - T9 are superior to the umbilicus (T7 is at xiphoid)
- T10 is at the umbilicus
- T11 - L1 are inferior to the umbilicus

Arteries of the abdominal wall
- What are the arteries?
- Where are they located?
- What do they branch off from?
- Which ones anastomose?
Arteries of the abdominal wall
- Posterior intercostal arteries
- Subcostal arteries
-
Superior epigastric arteries
- Located in rectus sheath, deep to rectus abdominis
- Branches of internal thoracic arteries
- Anastomose with inferior epigastic arteries within rectus sheath
-
Inferior epigastric arteries
- Located within the rectus sheath, deep to rectus abdominis
- Branches of external iliac arteries
- Anastomose with superior epigastic arteries within rectus sheath
-
Superficial epigastric arteries
- Located in superficial fascia and course vertically towards the umbilicus

Veins of the abdominal wall
- Do veins accompany arteries?
- Name two of the abdominal wall venous anastomoses
- Significance of anastomoses?
Veins of the abdominal wall
- Veins accompany arteries and share the same names
- They form extensive venous plexuses with many anastomoses
- These venous anastomoses are clinically significant as they provide alternative routes for venous return to the heart when normal venous channels are blocked
- Examples of abdominal wall venous anastomoses:
- Superior and inferior epigastric veins
- Paraumbilical and superficial epigastric veins

Describe the superior and inferior epigastric venous anastomoses
Superior and inferior epigastric venous anastomoses
Caval-caval anastomoses
If blood flow through the inferior vena cava is blocked, venous blood withing the inferior epigastric veins can be shunted to the superior epigastric veins, and from there to the superior vene cava via numeros tributaries

Describe the paraumbilical and superficial epigastric venous anastamoses
Paraumbilical and superficial epigastric venous anastamoses
Portal-caval anastomosis
If blood flow through the liver is blocked (portal system blockage), venous blood within the paraumbilical veins (part of the portal system), can be shunted to the superficial epigastric veins. As a result, the veins radiating from the umbilicus dilate, creating a caput medusae (Medusa’s head)

Where does lymph drain superior and inferior to the umbilicus?
Superior to the umbilicus, lymph drains to the axillary lymph nodes
Inferior to the umbilicus, lymph drains to the superficial inguinal lymph nodes

Inguinal ligament
- What is it?
- What does it span between?
Inguinal ligament
Inferior part of the external oblique aponeurosis
Spans between the ASIS and the pubic tubercle

Inguinal canal
- Where is the inguinal canal located?
- Where are the deep and superficial inguinal rings location?
- Describe how it is a potential site for herniation
Inguinal canal
- Oblique canal within the anterior abdominal wall
- Superior to the inguinal ligament
Deep inguinal ring
- Internal entrance where structures enter the canal
- Located just superior to the midpoint of the inguinal ligament and lateral to inferior epigastric vessels
Superficial inguinal ring
- External exit where structures leave the canal
- Slit like opening within the external oblique aponeurosis
- Located superlateral to the pubic tubercle
The inguinal canal is a potential site of weakness for herniation, however as the rings do NOT overlap (due to the oblique course of the inguinal canal), increases in the intra-abdominal pressure force the walls of the canal to tightly oppose, closing this potential pathway

Ontogeny of the inguinal canal in a stereotypical male
- Where do the testes initally develop?
- What is the gubernaculum?
- Describe how the testes descend, include how the spermatic cord is formed
- What is each layer of the scrotum / spermatic cord derived from?
Ontogeny of the inguinal canal in a stereotypical male
- Testes initially develop in the posterior abdominal wall
- Gubernaculum - ligament cord that connects testes to scrotum
- Testes descend down the inguinal canal, through the deep and superficial rings, and enter the scrotum
- As they descend, the testes drag the vasculature, nerves, lymphatics, and ductus deferens through the canal. These structures form the spermatic cord
Fascia coverings from superficial to deep:
- External spermatic fascia - derived from external oblique aponeurosis
- Cremaster muscle and fascia - derived from internal oblique muscle and aponeurosis
- Internal spermatic fascia - derived from transversalis fascia

Ontogeny of the inguinal canal in a stereotypical female
- Where do the ovaries develop?
- What is the gubernaculum?
- What are the adult derivatives of the gubernaculum?
- Is the inguinal canal larger or smaller in females and why?
Ontogeny of the inguinal canal in a stereotypical female
- Overies also develop in the posterior abdominal wall and descend
- Gubernaculum - connects the ovaries and uterus to the labium majora
- Adult derivatives of the gubernaculum in the female:
- Ovarian ligament - between ovary and uterus
- Round ligament of the uterus - between uterus and labium majora
- Since the ovary never goes through the inguinal canal, the canal is narrower in females

What are the contents of the inguinal canal?
Contents of the inguinal canal
- Spermatic cord (males)
- Round ligament of the uterus (females)
- Ilioinguinal nerve (L1)
- Genital branch of the genitofemoral nerve (L1 and L2)

Ilioinguinal nerve and genital branch of the genitofemoral nerve
- Which vertebrae?
- What kind of innervation do these nerves provide and to where?
Ilioinguinal nerve
- L1
- Sensory innervation from:
- Inguinal region
- Scrotum / labia majora
- Inguinal region
Genital branch of the genitofemoral nerve
- L1 and L2
- Sensory innervation from:
- Inguinal region
- Scrotum / labia majora
- Motor innervation to cremaster muscle in the male

Inguinal hernias
- What is it?
- Occur more in males or females?
- What are the two types?
Inguinal hernias
- Protrusion of abdominal viscera through the abdominal wall
- Inguinal hernias occur more in males
- Indirect (congenital) and direct (acquired)

Indirect (congenital) inguinal hernia
- Is indirect or direct more common?
- Describe how mass herniates - where does it enter, what does it exit
Indirect (congenital) inguinal hernia
- Most common type of inguinal hernia
- Herniating mass enter the deep inguinal ring (lateral to the inferior epigastric vessels)
- It transverses the inguinal canal and becomes enclosed in the fascial coverings of the spermatic cord (3 layers)
- Exits the superficial inguinal ring and enters the scrotum or the labia majora

Direct (acquired) inguinal hernia
- Is indirect or direct more common?
- What are the borders of the inguinal triangle?
- Describe how the mass herniates
Direct (acquired) inguinal hernia
- Indirect is more common
- Involves an area of weakness called the inguinal triangle, which is bound by the rectus abdominis, inferior epigastric vessels, and inguinal ligament
- Mass pushes into peritoneum and transversalis fascia, medial to inferior epigastric vessels
- Enters the inguinal canal through its posterior wall
- Mass rarely enters scrotum
- If it does, the mass is lateral and outside of the spermatic cord



