Anesthesia Gas Monitoring Flashcards
Why do we care?
- inadvertent agent OD
- timing to reach MAC/MAC awake
- error detection in vaporizer filling
- monitor uptake/distribution
- monitor low-flow anesthesia
How is gas monitoring measured?
Infrared analysis- gasses with 2+ dissimilar molecular atoms in molecule have specific/unique infrared absorption spectra
Can O2 be measured with infrared analysis?
NO! 2 similar atoms in molecule.
How is O2 monitoring measured?
-requires paramagnetic/fuel-cell analysis
Infrared photospectrometry
- amt of IR rays absorbed is proportional to the concentration of the absorbing molecules
- compared to known standard
- calculated
Diverting =
Sidestream sampling
How does diverting: sidestream sampling function?
- continuously aspirates a sample of gas from patient circuit near the breathing circuit and airway device connection (as close to the patient as possible)
- detects inspired/expired gases simultaneously
How many mls aspirated from diverting: sidestream sampling?
50-250 mls
Diverting: Sidestream sampling
- sample directed between infrared emitter, optical filter, & infrared detector -> outputs a signal proportional to remaining infrared E not absorbed by gases -> detected signal amplified/interpreted via microprocessors
- multiple optical filters required if identifying multiple gases simultaneously
Advantages of diverting: side stream sampling
- automatic calibration/zeroing
- minimal dead-space
- minimal cross contamination between patients
Disadvantages of diverting: side stream sampling
- multiple places leaks could occur
- more variability in CO2 reading
- slower response to changes
Non-diverting =
in-line gas sampling
How does non-diverting: in-line sampling function?
-measures gas concentration by using sensor that is located DIRECTLY in the gas stream
What gases are measured with non-diverting: in-line sampling?
O2 & CO2
How does non-diverting: in-line sampling measure CO2?
infrared analysis with sensor between breathing system and patient
How dose non-diverting: in-line sampling measure O2?
electrochemical analysis with sensor in the inspiratory limb of breathing circuit
Issues with diverting: side stream sampling monitoring
- high sample flow (200 ml/min)
- high flow rate impedes use with infants d/t inspiratory/expiratory flows similar to analyzer
- water vapor, liquid, secretions remain isolated from system (Dfend water trap)

Increase EtCO2:
- increased muscular activity (shivering)
- MH
- increased CO (resuscitation)
- Bicarb infusion
- Tourniquet release
- effective bronchospasm therapy (bronchodilation)
- decreased minute ventilation (hypoventilation)

Decrease EtCO2:
- decreased muscular activity (NMBA)
- hypothermia
- decreased CO (cardiac arrest)
- pulmonary embolism
- bronchospasm
- increased minute ventilation (hyperventilation)

Esophageal intubation- little or no CO2 present

Inadequate seal around ETT
possible causes:
- leaky/deflated cuff
- airway too small for patient

Hypoventilation
possible causes:
- decreased RR
- decreased TV
- increase metabolic rate
- hyperthermia

Hyperventilation
possible causes:
- increased RR
- increased TV
- decreased metabolic rate
- hypothermia

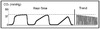
Rebreathing
possible causes:
- faulty expiratory valve
- inadequate inspiratory flow
- insufficient expiratory flow
- malfunction of CO2 absorbant