Anesthesia Consultation Flashcards
What is the purpose of the preoperative consultation?
To reduce the patient’s surgical and anesthetic perioperative morbidity or mortality, and to return the patient to desirable level functioning as quickly as possible.
“Perioperative risk” is multifactorial and a function of: (3)
- the preoperative medical condition of the patient
- the invasiveness of the surgical procedure
- the type of anesthetic administered
Surgical procedures and administration of anesthesia are associated with a complex stress response that is proportional to: (4)
- the magnitude of injury
- total operating time
- amount of intraoperative blood loss
- degree of postoperative pain
What is the key factor in improving outcome and lowering the length of hospital stay as well as the total costs of patients care?
Decreasing the stress response to surgery and trauma
What are the goals of preoperative evaluation?
- Documentation of the condition(s) for which surgery is needed.
- Assessment of the patient’s overall health status.
- Uncovering of hidden conditions that could cause problems both during and after surgery.
- Perioperative risk determination.
- Optimization of the patient’s medical condition in order to reduce the patient’s surgical and anesthetic perioperative morbidity or mortality.
- Development of an appropriate perioperative care plan.
- Education of the patient about surgery, anesthesia, intraoperative care and postoperative pain treatments in the hope of reducing anxiety and facilitating recovery.
- Reduction of costs, shortening of hospital stay, reduction of cancellations and increase of patient satisfaction.
What is the most important component of the preoperative evaluation?
patient history
What should the patient history include? (8)
- a past and current medical history
- a surgical history
- a family history
- a social history (use of tobacco, alcohol and illegal drugs)
- a history of allergies
- current and recent drug therapy
- unusual reactions or responses to drugs and any problems or complications associated with previous anesthetics.
- family history of adverse reactions associated with anesthesia should also be obtained.
A focused pre-anesthesia physical examination includes: (2)
- an assessment of the airway
- lungs and heart, with documentation of vital signs
When is a complete blood count needed? (4)
- major surgery
- chronic cardiovascular, pulmonary, renal, or hepatic disease, or malignancy
- known or suspected anemia, hemorrhage, or myelosuppression
- less than 1 y/o
When is an PTT/INR indicated? (3)
anticoagulant therapy
bleeding diathesis (hemorrhage)
liver disease
When are electrolytes and creatinine labs indicated? (5)
HTN
renal disease
diabetes
pituitary or adrenal disease
digoxin or diuretic therapy
An EKG is indicated prior to surgery for these patients:
- heart disease, HTN, diabetes
- other risk factors for cardiac disease (including age, which alone is reason to get an ECG)
- subarachnoid or intracranial hemorrhage, CVA, head trauma
When is a CXR indicated preoperatively?
cardiac or pulmonary disease
malignancy
When should MAO be withdrawn prior to surgery?
Why?
2-3 weeks
risk of interactions with anesthetics
When should oral contraceptives be discontinues before elective surgery?
Why?
6 weeks
increased risk of venous thrombosis
When should patients discontinue their herbal supplements?
2 weeks prior
When should aspirin be discontinued prior to surgery?
7-10 days
When should thienopyridines (such as clopidogrel) be discontinued prior to surgery?
Why?
2 weeks before
Affects platelets
When should oral anticoagulants be discontinued prior to surgery?
What should INR level be?
4-5 days
1.5
What are major clinical predictors of increased risk for perioperative cardiac complications? (5)
recent MI
unstable or severe angina
decompensated CHF
significant arrhythmias
severe valvular disease
What are intermediate clinical predictors of increased risk for perioperative cardiac complications? (5)
mild angina
prior MI history
compensated CHF
diabetes
renal insufficiency
What are minor clinical predictors of increased risk for perioperative cardiac complications? (6)
advanced age
abnormal ECG
rhythm other than sinus
poor functional capacity
history of stroke
uncontrolled HTN
What are high risk predictors for perioperative cardiac complications? (cardiac complication rate of >5%) (4)
emergency surgery
aortic and major vascular surgery
prolonged surgical procedures with large fluid shifts or blood loss
unstable hemodynamic situations
What are intermediate risk procedures for perioperative cardiac complications? (cardiac complication rate of 1-5%) (6)
abdominal or thoracic surgery
neurosurgery
ENT procedures
minor vascular surgery
orthopedic surgery
prostatectomy
What are low risk procedures for perioperative cardiac complications? (cardiac complication rate of
breast surgery
superficial surgery
eye surgery
endoscopic procedures
plastic and reconstructive surgery
ambulatory surgery
What functional capacity, METS:
standard light home activities
walk around the house
walk 1-2 blocks on level ground at 3-5 km/hr
1-4 mets
What functional capacity, METS:
climb a flight of stairs
walk up a hill
run a short distance
moderate activities like golf, dancing, mounting walking
5-9 METS
What functional capacity, METS:
strenuous sports (swimming, tennis, bicycle) heavy professional work
>= 10 METs
What does METs stand for?
metabolic equivalents of oxygen consumption
What are postoperative pulmonary complications? (7)
Pneumonia
Atelectasis
Bronchitis
Bronchospasm
Hypoxemia
Respiratory failure with prolonged mechanical ventilation
Exacerbation of underlying chronic lung disease
What ASA status is a patient with mild systemic disease?
ASA 2
What ASA status is a patient with severe systemic disease?
3
What ASA status is a patient with severe systemic disease that is a constant threat to life?
ASA 4
What ASA status is a moribund patient who is not expected to survive without the operation?
ASA 5
What ASA status is an organ donor?
ASA 6
What are procedure-related risk factors?
Primarily based on how close the surgery is to the diaphragm (ie upper abdominal and thoracic surgery are the highest risk procedures)
What are risk factors for postoperative pulmonary complications?
procedure-related risk factors
length of surgery (>3 hrs)
emergency surgery
underlying chronic pulmonary disease
smoking
age >60
obesity
presence of sleep apnea
poor exercise tolerance
What patient should be carefully assessed preoperatively for symptoms and signs of peripheral vascular, cerebrovascular and coronary disease?
diabetics
Diabetics have a higher incidence of death after a ____ than non-diabetic.
MI
What should be administered prior to surgery for a diabetic prior to surgery to limit perioperative ischemia?
beta-blockers
When should you treat blood glucose perioperatively?
> 180 is a good rule of thumb
What are perioperative hyperglycemia complications?
dehydration
impaired wound healing
inhibition of WBC
For dental extractions, arthrocentesis, biopsies, ophthalmic operations and diagnostic endoscopy patients need to alter their regimen. True or false?
false
do not need to
What drugs should be considered for the anticoagulated patient?
IV heparin
LMWH (low molecular weight heparin)
Invasive surgery is generally safe (from major hemorrhagic complication) when the INR ~___.
1.5
It takes approximately __ days for the INR to reach 1.5 once oral anticoagulant is stopped preoperatively.
4
It takes approximately __ days for the INR to reach 2.0 once oral anticoagulant is restarted postoperatively.
3
Regional anesthesia can safely performed in in patients receiving anticoagulant or antiplatelet therapy provided that patient management is based on appropriate timing of needle placement and catheter removal relative to the timing of anticoagulant drug administration. True or false?
true
Indwelling catheters should not be removed in the presence of therapeutic anticoagulation, as this appears to significantly increase the risk of _____ _______.
spinal hematoma
What does this waveform indicate?

hyperkalemia
progressive evolution of changes in the EKG that can culminate in ventricular fibrillation and death.
The presence of EKG changes is a better measure of clinically significant potassium toxicity than serum level.
What does this waveform indicate?

hypokalemia
ST segment depression
Flattening of the T wave
Appearance of a U wave
What EKG changes occur with hyper and hypocalcemia?
Hypercalcemia = shortens QT interval
Hypocalcemia = prolongs the QT interval

What arrhythmia is associated with a prolonged QT interval?
torsades
What waveform is this?
What does this waveform indicate?

Osborne Waves
severe hypothermia
Note: The rhythm is atrial fibrillation. Bradycardia is present. The QT/QTc is prolonged.
What does this EKG depict?

Digitaisl effect.
Note the downsloping ST segment.
Digitalis toxicity is commonly associated with dysrhythmias and AV nodal blocks.
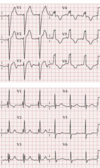
What are the following waveforms?

AV Node Blocks
- First degree AV block is normal except for a prolonged pr interval > 0.2 sec
- Second degree AV block (Mobitz 1 or Wenckebach) is a progressive lengthening of the pr interval until the QRS drops
- Second degree AV block (Mobitz 2) there is the presence of a dropped beat without progressive lengthening of the pr interval
- Third degree (complete heart block) no atrial impulses make it through to activate the ventricles. Ventricles respond by generating an escape rhythm.
What can the following drugs cause to change in an EKG:
Sotalol
Quinidine
Procainamide
Disopyramide
Amiodarone
Dofetilide
prolonged QT interval
What can the following drugs cause to change in an EKG:
Tricyclic Antidepressants
Phenothiazines
Erythromycin
Quinolone antibiotics
Antifungal medications
* Droperidol & Zofran
Can prolong QT interval
What are the stages of pericarditis found within the EKG?
ST segment elevation
T wave inversion which occurs after ST segment moves back to baseline
Q waves do not occur in pericarditis and the PR interval is sometimes depressed.

True / false
Q waves do not occur in pericarditis and the PR interval is sometimes elevated.
false
depressed
What condition is indicated by:
left ventricular hypertrophy and left axis deviation
Q waves in lateral leads I, aVL, V5, and V6

Hypertrophic Obstructive Cardiomyopathy (HOCM)
What does this strip indicate?

Hypertrophic Obstructive Cardiomyopathy (HOCM)
What does this strip indicate?

myocarditis
Note: Any diffuse inflammatory process involving the myocardium can produce a number of changes on the EKG. Most common are conduction blocks especially bundle branch blocks & hemiblocks.
What does this strip indicate?

COPD
Peaked p waves in leads II, III, aVF, and V1
right axis deviation
What changes will you see in a pulmonary embolus?
s waves in lead I
q waves in lead III
inverted t waves in lead III
S1 Q3 T3
True / False
Unlike an inferior infarction, in which Q waves are seen in at least two of the inferior leads, the Q waves in an acute pulmonary embolus are limited to lead III.
true
What do deeply inverted, wide T waves indicate?
CNS bleed


