An introduction to Blood Group Serology Flashcards
Blood Group Antigens are?
- Glycoproteins and glycolipids present on the surface of red cells
- Some (eg ABO) may be present more widely on endothelial surfaces
- Genetically determined
- Generally autosomal and co-dominant
- Xg system sex linked
- Limited understanding of biological function of the antigens
Describe the Genetic control of Blood groups
- Protein Determinants
- Gene codes for the antigenic determinant itself
- Rh, Kell, Duffy and Kidd systems
- Glycolipid Determinants
- Gene codes for production of enzymes that add or remove carbohydrate or lipids, through this you get definition of an antigen!
- ABO, Lewis group systems
Duffy Blood Group System and Malaria?
- The Duffy antigen on the RBCacts as the entry point to the red cell for the malarial parasite
- in caucasian populations the Fya-Fyb negativephenotype is rare
- In individuals with a black african ethnic backgroup up to 40% are Fya-Fyb- negative this represents the impact of natural selection for malarial resistance
The McLeod Phenotype
- Kx null phenotype associated with Chronic Granulomatous Disease and acanthocytosis!
Blood Groups Variation with Populations
- Varies significantly in different population types
- Most likely due to Genetic drift
- Usually no biological advantage apparent
- May have a clinical impact on the provision of compatible blood!!

Blood group antigens/systems are clinically important because they have the ability to
generate Blood Group Antibodies
Antibodies rcognise ‘foreign’ antigens
- May be IgM, IgG or occasionally IgA
- May be naturally occurring or immune stimulated
Difference between Naturally occuring and Immune stimulated Antibodies
Naturally Occurring:
- No exposure to foreign red cells but exposure to bacteria containing, for example, ‘A-like Antigens’.
- At birth baby has no ABs againsts ABO antigens, but by 6 months almost all babies will have formed some form of anti-A or Anti-B. This is because A or B antigens are very close to the antigens formed on the surface of bacteria
- Can Activate the Complement Cascade > intravascular destruction
- Anti-A produced
Immune Stimulated:
- exposure to foreign red cells (for example Rh+) by transfusion or pregnancy (Rh+ fetus)
- Cannot fully activate Complement Cascade > extravascular destruction
- can activate early phases, and coat early proteins
- Anti-Rh produced

Naturally Occurring Red Cell Antibodies
- Antigens that develop in the absence of exposure to the red cell antigen
- Most likely stimulated by cross reacing antigens derived from bacteria (as they’re very similar)
- Not present at birth but develop during 1st year of life
- Usually related to lipid antigens
- Significant IgM component to antibody, but IgG may also be present
- ABO and Lewis antigens fall in this category
Immune Stimulated Red Cell Antibodies
- Develop only following exposure to specific antigen
- May be produced following
- transfusion
- pregnancy
- injection (eg IVDU)
- Normally IgG in nature
A brief overview of the history of Transfusion.
Just for extra info
- Earliest record of transfusion in the early 19th century, for women bleeding heavily following childbirth. Would use husbands blood via cannuler. “Blundell Transfusion”
- Some died immediately, and some survived.
- Later on Dr Karl Landsteiner discovered the ABO blood group system
- the ABO blood group system is the most likely to kill you, and the best to know about
Where are ABO antigens found?
Present on the surface of
- Blood cells
- Epithelial cells
- Body fluids
What determines the ABO phenotype?
The phenotype is determined by a series of glycosyltransferase enzymes. These are resposible for addition of CHO molecules to the basic membrane structure.
The H antigen is neccessary for the ABO phenotype to be expressed
this is present in (almost) everyone

The ABO groups all have an H group attached, but whats the molecular difference in this!

H:** base structure with a D-galactose and fucose sugar. **This alone is known as the O blood group!!
A: N-acetylgalactosamine added to the surface of the red cell
B: Galactose added to the surface of the red
Therefore your blood group is determined by the presence of a sugar molecule

What does it mean by the ABO blood group being ‘co-dominant’
You inherited one gene from your mum and one from dad, and this COLLECTIVELY determines phenotype.
By 6 months of life you’ve developed antibodies against the A or/and B antigens which you lack
O is the most common phenotype!

Clinical Relevance of ABO systems
- ABO antibodies: naturally occuring and appear ~3-6months old
- Most important blood group as → to fatal transfusion errors
- ABO incompatible transfusion results in complement activation leading to…
- intravascular haemorrage
- renal failure
- DIC
Therefore for a tranfusion we select antigens that don’t have ___________
Therefore for a tranfusion we select antigens that don’t have corresponding antibodies present in the recepiants plasma
eg; blood group O (has therefore anti-A and Anti-B present) cannot be transfused with A or B groups. Can only be transfused with O
O is therefore the universal Donor but as a small population they can’t sustain everyone!

The Rh Blood Group System
- Second most important blood group system
- Protein antigen
- Expressed only on RBC
- antibodies only produced post exposure to the D+ red cells ‘immune stimulation’
- Rh(D) is highly immunogenic,
- if you expose a group to D+ red cells 80-90% will have a reaction
What is Rh(D)?
- Most important antigen of the Rh system
- Everyone is either Rh(D) positive or Rh(D) negaticed antigen is amorph
Rh(D) negative: dd
Rh(D) positive: DD or Dd

population frequency of Rh(D) in NZ?

Rh(D) and transfusion
- 90% of Rh(D) negative individuals transfused with a unit of Rh(D) positive red cells will produce anti-D strong immune reaction
- Anti-D is an IgG antibody that is unable to bind complement, Red cell destruction is extravascular
- Anti-D is the most common cause of Haemolytic Disease of the newborn: fetus RBC cross into mum, if fetus is D positive from Dad and mum is negative > anti-D formation > problems for mum in subsequent pregnancies
- Normally transfuse red cells of the same Rh(D) type as the recipient
- Never transfuse Rh(D) positive red cells to an Rh(D) negative female of child bearing age; male would only require D negative cells, not a biggie
Describe what the Rh antigen is??
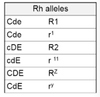
Describe the Expanded Rh system

- THe Rh system is the most complex of known blood group systems
- Rh antigen: product of 3 genetically closely linked alleles; which make allelic pairs
- C and c
- D and d (d is an amorph)
- E and e
- 3 allelic antigens behave as a single entitiy
- a number of common alleles can therefore be defined
Minor Blood Group Systems

- Over 400 blood group systems have been defined
- Majority not of clinical interest, but some relevance to
- frequency of antigen in pop
- frequency of antibody production following transfusion
- ability of antibody to destroy transfused red cells
- Relevance is higher if a small amount of the population will react
What are the 3 blood group systems of common clinical interest?
- Kell: K (Kell) and k (cellano)
- Kidd: Jka and Jkb
- Duffy: Fya and Fyb
Don’t need to know gene frequencies

Laboratory Techniques for detecting antigens and antibodies
- Often involves an agglutination technique; when the antibody + antigen put together they CLUMP
- Antigen testing usually uses commercially sourced monoclonal reagents
- these have high specificity and sensitivity
- are IgM in nature
- produce direct agglutination
- Molecular typing methods increasingly available











