AKI, CKD Flashcards
KDIGO AKI GUIDELINE
stage 1
stage 2
stage 3
•Preferred definition for AKI based on 3 stages consisting of ONLY Cr and Urine Output
•Stage 1
- Increase Cr 1.5-1.9 baseline or
- decreased UO
•Stage 2
- Increase Cr 2-2.9X baseline or
- UO 12 hrs
•Stage 3
- Increase Cr 3X baseline or
- Cr >4 or UO reduction 24hrs or anuria >12hrs
FeNa VS FeUrea or FeUA
FeNa: not accurate if pt is on diuretics w/in 24hrs
•FeNa < 1% = pre-renal azotemia
•FeNa >1% = intrinsic renal failure
•FeNa >4% = post-renal failure
FeUA: NOT influenced by diuretics
•FEUrea < 35% or FEUA < 9-10 % = prerenal
•FEUrea > 50% or FEUA > 10-12 % = ATN
- FeNa < 1% =
- FeNa >1% =
- FeNa >4% =
- FeNa < 1% = pre-renal azotemia
- FeNa >1% = intrinsic renal failure
- FeNa >4% = post-renal failure
Prerenal inury causes?
Hypovolemia
↓ cardiac output
↓ effective circulating volume
Prerenal Injury labs
Volume depletion
Decreased CO/Effective arterial volume
Urine output
Volume depletion
•Hemoconcentration: ↑ H/H, albumin, calcium
•↑ Na, BUN, Cr
Decreased CO/Effective arterial volume
•Edema
•↓ Na, Albumin
Urine output
•Oliguria (<500ml/d) or anuria (<100ml/day)**
- High specific gravity (>1.015)
- Normal sediment or hyaline casts
- Low Urine Na (<20mEq/L)
tx prerenal dz due to DEC CO effectivenes
↓ CO/Effective circulating volume
Optimize cardiac performance carefully
- •Diuretics (volume overloaded) -high dose IV
- •Nitrates
- •Dobutamine
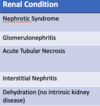
3 categores of intersitial AKI
Glomerular
- PSG
- IgA Nephropathy
- Nephrotic syndrome /Minimal change
- Polycystic kidney Dz
Tubules & Interstitium
- Acute Tubular Necrosis
- Acute Interstitial Nephropathy
Vascular
- Renal Artery Obstruction – vasculitis
- Renal Vein obstruction
- Microangiopathy – TTP, HUS, DIC
si/sx of Vascular intersitial AKI
FeNa >1% intrinsic renal failure
LE rash: livedo reticularis
urine eosinophils
postrenal AKI can be defined as
↑BUN and Cr from obstruction to urine flow in ureters, bladder or urethra (anuric & <5% of ARF
- BOO (ex. BPH, prostate cancer)
- Neurogenic bladder
- Malignancy (ex. ovarian, cervical, retroperitoneal)
- Pregnancy
Meds (Acyclovir, methotrexate, sulfa drugs
Polycystic Kidney Dz etiology
Autosomal dominant genetic disorder
- cyst formation
- enlargement of the kidney (and other organs ie. Pancreas, liver, spleen)
si/sx Polycystic Kidney Dz
Diffuse pain -abdomen, flank, back
- •Enlargement of cysts
- •Hemorrhage into cyst or perinephric hematoma
- •Infectious – UTI, pyelonephritis, abscess, infected cyst
- •Nephrolithiasis (20-30%)
HTN
+/- palpable flank mass
+/- hepatomegaly
Tx Polycystic Kidney Dz
BP management (ex. ACEI/ARB) =slow progression of dz
Pain management: AVOID NSAIDs
Nephrectomy / Surgical cyst decompression
Monitor & manage recurrent infections: UTI/Cysts
Hematuria: may need transfusion!!!
definition and causes of Acute Interstitial Nephritis
allergic reaction to medication
- •Antibiotics: B-lactams, sulfonamides, vancomycin, erythromycin, rifampin
- •Acyclovir
- •NSAIDS (either direct toxicity or allergy)
- •Anticonvulsants: Phenytoin, valproate, carbamazepine
Post-infectious
Autoimmune
si/sx of Acute Interstitial Nephritis
After recent new drug exposure
Fever
Skin rash
Peripheral eosinophilia
Oliguria
more commonly, patients are found incidentally to have rising serum creatinine after initiation of new med
WBC casts & Hematuria
Dz?
Tx
Acute Interstitial Nephritis
D/c of offending agent: reversal of renal injury
Glucocorticoid therapy: accelerate renal recovery
- •6 week taper prednisone or
- •IV methylprednisolone pulse 3 days)
Potential Nephrotoxins that cause ATN
- NSAIDs
- Chemotherapeutic agents
- Aminoglycosides
- Amphotericin
- Vancomycin
- Radiocontrast dye (GFR 30 rad cutoff)
- Poison (ethylene glycol, heavy metals)
UA - Pigmented granular casts (muddy-brown casts)
electrolyte changes?
Acute Tubular Necrosis (ATN
Serum hyperkalemia
Serum hyperphosphatemia
Serum hyperuricemia
Tx Acute Tubular Necrosis (ATN
Aggressive volume replacement– hydrate (If nephrotoxic agent, volume depletion)
Oliguria present and extracellular-volume normalized:
- • consider loop-diuretic high dose (100-200mg Lasix) to improve urine output
Protein restriction
Cola colored urine (blood degraded/hematuria/RBC casts)
Edema
Hypertension (salt & fluid retention)
Dx
Post-strep glomerulonephritis
dx Post-strep glomerulonephritis
+ throat, skin culture for strep A
•Elevated titers of abs to strep products
•(+) Anti-streptolysin (ASO)*
UA: Hematuria – RBC casts
•Proteinuria
(-) strep A antibody test
Urine red or coca cola 1-2 days s/p onset
Dx & Tx
IgA Nephropathy
ACE-/ARB, Steroids
Dialysis
Renal transplant
Heavy proteinuria (>3.5g/24hr)
Hypoalbuminemia (<3 g/dL)
Peripheral edema
Nephrotic Syndrome: adult
minimal change: children
dx minimal chanhe histology?
Light microscopy is normal on renal bx
Histology - diffuse effacement of the epithelial cell foot processes on electron microscopy
Hypoalbuminemia
tx minimal change
Prednisone
name uurine sediment that correlated w/ dz

define CKD
Progressive loss of renal function that persists for more than 3 months
Commonly irreversible
Usually caused by long-term diseases such as DM, HTN
pathophys of CKD
- 1.Underlying etiology causes Adaptive hyperfiltration and nephron damage
- 2.In response to any damage the kidney - kidney ↑ filtration rate to normal undamaged nephrons (Hyperfiltration)
- 3.Hyperfiltration over time = glomerular hypertrophy, distortion of the glomerular architecture, sclerosis and l_oss of remaining nephrons_
- 4.Manifested by proteinuria and progressive renal failure
RAAS and AII impact on CKD
RAAS and AII activated trying to maintain GFR w/ resultant hyperfiltration however…
↑ Pore size in GM by AII = increasing protein leak across the glomerular basement membrane
Consequence of repeated and continued activation of the RAAS = Microalbuminuria/Proteinuria - toxic to the tubules
define azotemia and how it rekates to uremic syndrome
Uremic Syndrome: clinical manifestations of uremia / advanced renal failure (stage 5)
- Symptomatic manifestations associated with Azotemia
Azotemia = the accumulation of urea and other nitrogenous compounds and toxins caused by the decline in renal function
define CKD stages
Stage 1
Stage 2
Stage 3
Stage 4
Stage 5
Stage 1: GFR ≥ 90
Stage 2: GFR 60-89
Stage 3: GFR 30-59
Stage 4: GFR 15-29
Stage 5: GFR <15 or dialysis
CKD maging modality of choice
Renal US (consider other imaging) – imaging modality of choice
CKD When to Refer to Nephrology?
- GFR < 30ml/min (CKD Stages 4 and 5)
- Rapidly progressive CKD
- Poorly controlled HTN despite 4 agents
- Rare or genetic causes Suspected renal artery stenosis


