Acid base and Fluids Flashcards
describe Acid-Base Homeostasis
normal arterial pH?
- Respiratory mechanism
- Renal mechanism
•Arterial pH is maintained between 7.35 – 7.45 by extracellular and intracellular chemical buffering systems along with respiratory and renal mechanism
•Respiratory mechanism:control arterial CO2 tension (PaCO2 )
•Renal mechanism: control plasma bicarbonate (HCO3 - )
components of Abg
uses?
pH
Oxygen tension (Pa02 )
Carbon dioxide tension (PaCO2 )
Oxyhemoglobin saturation (Sa02 )
Bicarbonate concentrations (HCO3 -)
USES
Identify acid-base disturbances
Measures partial pressures of O2 and CO2
Assessment of the response to therapeutic interventions
Procurement of blood samples in emergencies when venous blood is not feasible
blood pH values identify:
- Acidemia –
- Alkalemia –
- Acidosis –
- Alkalosis –
- Acidemia – arterial pH < 7.35
- Alkalemia – arterial pH > 7.45
- Acidosis – ↓extracellular fluid pH
- Alkalosis – ↑extracellular fluid pH
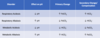
describe changes seen in (pH, HCO3, CO2)
- Metabolic acidosis –
- Metabolic alkalosis –
- Respiratory acidosis –
- Respiratory alkalosis -
- Metabolic acidosis – ↓serum HCO3- & pH
- Metabolic alkalosis – ↑serum HCO3- & pH
- Respiratory acidosis – ↑arterial pCO2 & ↓ pH
- Respiratory alkalosis - ↓ arterial pCO2 & ↑pH
define
- Primary respiratory disturbance →
- Primary metabolic disturbances →
•Primary respiratory disturbance →
- primary change in PaCO2 →
- invokes compensatory metabolic response →
- secondary change in HCO3 –
•Primary metabolic disturbances →
- primary change in HCO3 - →
- invokes compensatory respiratory response →
- secondary change in PaCO2
arrows in
- Metabolic acidosis –
- Metabolic alkalosis –
- Respiratory acidosis –
Respiratory alkalosis
pH & CO2
Opposite = respiratory process
Same direction = metabolic process
CO2 in
Respiratory Acidosis
Respiratory Alkalosis:
Respiratory Acidosis: TOO MUCH CO2 = TOXIC
Respiratory Alkalosis: LOSING TOO MUCH CO2
Hyperventilation Syndrome: panic attack causes what ?
Respiratory Alkalosis
arrow in
Respiratory Acisodis
Respiratory Alkalosis
pH & CO2 going in OPPOSITE directions!!!

arrows in
Metabolic acid
Metabolic Alk
OPPOSITE DIRESTION

resp acidosis is caused by?
tx?
- Severe pulmonary failure
- Respiratory muscle fatigue
- Abnormalities in ventilatory control
Reverse underlying cause
Tracheal intubation and assisted mechanical ventilation
si/sx of Respiratory Alkalosis:
Dizziness
Mental confusion
Seizures
Hypotension
Decreased cardiac output
Cardiac arrhythmias
metabolic acidosis causes
- ↑ endogenous acid production (lactate or ketoacid)
- Loss of bicarbonate (diarrhea)
- ↑endogenous acid bc of ↓ excretion of acid by the kidneys (CKD)
si/sx of metabolic acidos
LOOK SICK
- Increase in ventilation and TV (Kussmaul respirations)
- ↓cardiac contractility
- Peripheral arterial vasodilation
- Central venous constriction
- Decrease in central and pulmonary vascular compliance → pulmonary edema
- Depressed CNS function → headache, lethargy, stupor, coma
normal anion gap acidosis is defines as
The presence of a metabolic acidosis with a normal anion gap and hyperchloremia
causes of high anion gap met acidosis
MUD PILES
- Methanol
- Uremia
- Diabetes
- Paraldehyde
- Iron (and Isoniazid)
- Lactate
- Ethylene glycol
- Salicylate
non-anion gap avidosis is describes ad
Bicarbonate loss from the GI tract or kidneys – kidneys over excrete bicarb
- Vomiting
- Diarrhea
si/sx of Metabolic Alkalosis
what electro;yte abnorm are seen?
- ↑ in HCO3 –
- ↓ nonvolatile acid (usually HCl) from the extracellular fluid (vomiting or NG tube suction)
- Failure of the kidneys to eliminate HCO3 –
Often accompanied by hypochloremia and hypokalemia
si/sx Metabolic Alkalosis
Similar to those of hypocalcemia
- Mental confusion
- Obtundation
- Predisposition to seizures
- Paresthesia
- Muscle cramping
- Tetany
- Aggravation or arrhythmias
- hypoxemia
_Frequently occurs as a mixed disorder in association wit_h
- respiratory acidosis
- respiratory alkalosis,
- metabolic acidosis
Metabolic Alkalosis
tx of Metabolic Alkalosis
Treat hypokalemia with potassium replacement
- Stop loop / thiazide diuretics
- Acetazolamide – Diamox = weak diuretic makes you hold onto your bicarb!
arrows in
metabolic acid
metabolic alk
pH CO2 in SAME direction

causes of high anion gap acidosis
Lactic Acidosis= ↑lactateKetoacidosis
Drug/Toxin Induced
Chronic Kidney Disease
Lactic Acidosis= ↑lactate
- Poor tissue perfusion (type A)
- Aerobic disorders (type B)
- D-Lactic acid acidosis
Ketoacidosis
- Diabetic Ketoacidosis (DKA)
- Alcoholic Ketoacidosis (AKA)
Drug/Toxin Induced
- Salicylates
- Ethylene Glycol
- Methanol
- Propylene Glycol
- Isopropyl Alcohol
- Pyroglutamic Acid
Chronic Kidney Disease
caused by injestion of asprin & accompanied by a respiratory alkalosis
high anion gap met acidosis - Salicylates



