Abdomen Flashcards
What are the laters of the abdomen lateral to rectus sheath?
Skin
Camper fascia (fatty layer)
Scarper Fascia (membranous layer)
Thin layer of deep fascia
External obliue muscle
Internal obliue muscle
Transversus abdominus
Fascia Transversalis
Extraperitoneal tissue
Parietal peritoneum

What are the abdominal wall layers anterior to the rectus sheath above arcuate line?
Skin
Campers fascia
Scarpas fascia
Thin later deep fascia
Anterior wall of rectus sheath
Rectus abdominus muscle
Posterior wall rectus sheath
Fascia transversalis
Extraperitoneal connective tissue
Parietal peritoneum

Abdominal wall layers in midline
Skin
Scarpers fascia
Campers fascia
Thin layer deep fascia
Linea alba
Transversalis fascia
Extraperitoneal connective tissue
Parietal peritoneum

Why is the membranous layer of superficial fascia important in the extravasation of urine?
Important as closed space that does not open into the thigh
Membranous rupture of the urethra may be followed by extravasation of urine into scrotum, perineum, penis and lower part of ant. abdominal wall deep to membranous layer of fascia
Urine excluded from thigh due to attachment of fascia to fascia lata
External oblique
origin: ribs 5-12
insertion: iliac crest and pubic tubercle
innervation: thoracoabdominal nerves

Internal oblique
origin: inguinal ligament, iliac crest, lumbodorsal fascia
insertion: ribs 10-12
innervation: thoracoabdominal nerve

Transversus abdominis
origin: inguinal ligament, costal cartilage, iliac crest and thoracolumbar fascia
insertion: conjoint tendon, xiphoid process, linea alba and pubic crest
innervation: thoracoabdominal muscles, subcostal

Rectus abdominis
origin: Crest of pubis
insertion: xiphoid process and sternum and costal cartilage 5-7
innervation: thoracoabdominal nerves

Pyramidalis
origin: pubic crest, pubic symphysis
insertion: linea alba
innervation: subcostal nerves

Rectus sheath
Formed by the aponeurosis of three flat muscles
Anterior wall - aponeurosis of external oblique and internal oblique
posterior wall - aponeurosis of internal oblique and transversus abdominis
ARCUATE LINE - midway from umbilicus to pubic symphysis where the posterior wall also lies anterior to the rectus sheath

What occurs at the arcuate line?
Inferior epigastric vessels pierce rectus abdominus and pass upward to anastamose with the superior epigastric vessels
\Post and ant rectus sheath passes anterior to rectus abdominus muscle below Arcuate line
Posterior abdominal wall
Quadratus lumborum
Psoas major
psoas minor

Quadratus lumborum
origin: iliac crest and iliolumbar ligament
insertion: transverse process of L1-L4
innervation: T12- L4

Psoas major
origin: T12-L5
insertion: Lesser trochanter
innervation: L1-L3

Psoas minor
origin: T12, L1
insertion: superior ramus of pubis
innervation: L1 action: flexion fo vertebral column

Fascia of the posterior wall
Psoas fascia - encloses psoas major & minor thoracolumbar fascia - divided into 3 layers, anterior, middle and posterior layer

Peritoneum
Continous layer divided into parietal and visceral peritoneum
Squamous epithelial cells from mesothelium

Parietal peritoneum
Somatic sensation thus well localised sensitive pain, laceration, temperature
Visceral peritoneum
Splanchnic mesoderm origin poorly localises, referred to pain in dermatomes
Sensitive to chemical and stretch
Retroperitoneal organ
SAD PUCKOR. Can be primary or secondary. Primary if developed and remain outside of parietal peritoneum.
Suprarenal glands
Aorta
Duodenum (except 1st part)
Pancreas (except the tail)
Ureters
Colon (ascending & descending)
Kidneys
Oesophagus
Rectum
Peritoneal reflections
Mesentery
Greater omentum
Lesser omentum

Mesentery
Double layer of the visceral peritoneum
Connects the organs to the posterior abdominal wall
Small bowel
Transverse colon
Sigmoid mesocolon
Mesoappendix

Greater omentum
Greater curvature of stomach and proximal part of duodenum to anterior surface of transverse colon
Act as immunological barrier

Lesser omentum
Lesser curvature of stomach & proximal part of duodenum to liver
Hepatogastric ligament & hepatoduodenal ligament
Greater sac
Divided by transverse mesocolon
Supracolic - stomach, liver and spleen
Infracolic - small intestine, colon

Lesser sac
posterior to stomach and lesser omentum
connected to greater sac via EPIPLOIC FORAMEN
situated posterior to the free edge of the hepatoduodenal ligament

Boundaries of epiploic foramen?
Greater and lesser sac are in communication with each other through epiploic foramen
Boundaries:
- *Anteriorly**: Portal vein, hepatic artery & common bile duct
- *Posteriorly**: IVC
- *Superiorly**: Caudate lobe of liver
- *Inferiorly**: first part duodenum

What is the Pringle manouvere?
Clamping of the hepatoduodenal ligament (ant boundary of the epiploic foramen)
This will include clamping:
- hepatic artery proper
- portal vein
- common bile duct
Peritoneum in pelvis
Male - rectovesical pouch - CLOSED
female - vesicouterine pouch and rectouterine pouch (pouch of douglas)

Inguinal canal - borders
MALT: (2M, 2A, 2L, 2T)
Starting from superior, moving anticlockwise in order to posterior:
Superior wall (roof): 2 Muscles
internal oblique Muscle
transverse abdominus Muscle
Anterior wall: 2 Aponeuroses:
Aponeurosis of external oblique
Aponeurosis of internal oblique
Lower wall (floor): 2 Ligaments
inguinal Ligament·
lacunar Ligament
Posterior wall: 2 Ts
Transversalis fascia
conjoint Tendon

Inguinal canal content
Spermatic cord (men)
Round ligament (women)
Ilioinguinal nerve

Spermatic cord content
3 fascia - external spermatic (external oblique aponeurosis), cremaster muscle & fascia (internal oblique aponeurosis) and internal spermatic fascia (transversalis fascia)
3 arteries - testicular, cremaster, vas
2 nerves - autonomic, genital branch of genitofemoral nerve
4 others - pampiliform, lymphatics, vas deferens, tunica vaginalis

Formation of inguinal canal
GUBERNACULUM guides the descend of gonad (testis/ovaries) from posterior abdominal wall to scrotum
Inguinal canal is the pathway by which the testes leave the abdominal cavity and enter the scrotum
Processus vaginalis (part of peritoneum) degenerates but if not - leads to indirect hernia

GI Tract - oesophagus
approx 25cm in length
C6 to T11
pierces diaphragm at T10
attached to the phrenoesophageal ligament
consists of internal circular and external longitudinal muscles
Upper oesophageal sphincter - cricopharyngeus muscle, striated muscle
Lower oesophageal sphincter - PHYSIOLOGICAL (acute angle of entry, gets compressed with raised IAP, folds of mucosa and right crus of diaphragm

What is the arterial supply of the oesophagus?
Split into 1/3s
Upper 1/3: Inferior Thyroid artery
Middle 1/3: Direct branches from descending aorta
Lower 1/3: Branches from L gastric. Splenic artery dorsally

What is the venous drainage of the oesophagus?
Blood supply split into 1/3s

What is the lymphatic drainage of the oesophagus?
- *Lymph drainage:**
- *Proximal third:** deep cervical lymph nodes, and subsequently into the thoracic duct.
- *Middle third:** superior and posterior mediastinal nodes.
- *Distal third:** follow the left gastric artery to the gastric and celiac lymph nodes.
What cell type is found in the oesophagus?
Stratified squamous epithelium - prolonged exposure to acid causes metaplasia to stomach’s columnar epithelium.
AKA Barrett’s oesophagus - type of metaplasia
What are the points of narrowing of the oesophagus?
3 points:
Behind the cricoid cartilage of the larynx
Left bronchus & arch of aorta cross the front of the oesophagus
Right Crus of the diaphragam where oesophagus crosses

What is acalasia of the cardia?
Assoc with degeneration of the parasympathetic plexus (Auerbach’s plexus) in the wall of the oesophagus
Primary site of disorder may be innervation of the cardioesophageal sphincter by vagus nerves
Common symptoms:
Dysphagia & regurgiation
Later accompanied by proximal dilatation and distal narrowing of the oesophagus

What structures are found at the transpyloric plane?

GI tract - Stomach
Cardia - fundus - body - pylorus (ANATOMICAL SPHINCTER)
Greater curvature - reaches the pyloric antrums
Lesser curvature: has the angular notch which divives the body and pylorus
Drains to Left and & right gastric - hepatic portal vein
Gastro omental into SMV

Where does the left gastric originate from and what does it supply?
Arteries are derived from branches of the coeliac trunk
Left gastric (direct branch of coeliac artery) passes upwards and left to reach oesophagus and then descends on lesser curve of stomach - supplies upper right part stomach & lower 1/3 oesophagus

Where does the right gastric originate from and where does it supply?
Right Gastric: (CHA at upper border of pylorus) and runs to the left along the lesser curvature. Supplies lower right part stomach

Where do the short gastric arteries originate from and where do they supply?
Short Gastric arteries (arise from the splenic artery at the hilum of spleen) and pass forward to supply stomach along upper part of greater curvature

Where does the left gastroepiploic artery arise from and what does it supply?
Left gastroepiploic: Arises from splenic artery at the hilum of the spleen and pass forward in the gastrosplenic omentum to supply stomach along the upper part of greater curvature

Where does the right gastroepiploic artery arise from and what does it supply?
Right gastroepiploic: (gastroduodenal branch of hepatic artery) supplies stomach along the lower part of greater curvature

What is the venous drainage of the stomach?
Drains into portal circulation
Left & Right gastric veins drain directly into portal vein
Short gastric & gastroepiploic veins join the splenic vein
Right gastroepiploic vein joins the SMV

GI tract - Small interstine
Duodenum
Jejunum
Ileum

Duodenum
4 parts
1st - intraperitoneal, attached to liver by hepatoduodenal ligament, common area for ulcers
2nd - retroperitoneal, major duodenal papilla (posteromedial wall)
3rd - crosses over IVC and aorta, posterior to SMA
4th - duodenojejunal flexure, suspensory muscle of the duodenum supplied by gastroduodenal artery and inferior pancreaticoduodenal artery (SMA)

What is the arterial supply of the duodenum
& venous drainage?
Upper 1/2 supplied by superior pancreatoduodenal artery a branch of the gastroduodenal artery
Venous drainage - Sup. pancreatoduodenal vein drains into portal vein
Lower 1/2 supplied by inferior pancreatoduodenal artery which is a branch of Superior mesenteric artery
Venous drainage - Inf. pancreatoduodenal vein drains into IVC

What is the lymphatic drainage of duodenum?
Lymph vessels follow the arteries and drain upward via pancreaticoduodenal nodes to the gastroduodenal nodes and then to coeliac nodes

Jejunum and Ileum
attached the posterior wall by mesentery starts at the duodenojejunal flexure and ends at ileocaecal junction
Jejunum - thicker wall, longer vasa recta, less arcadesm red
ileum - thinner wall, shorter vasa recta, more arcades and pink

What is the lymphatic drainage of the Jejunum and Ileum?
Superior mesenteric nodes
Caecum
Surrounded by peritoneum
Muscle - is 3 longitudinal flat bands called teniae coli which converge at the base of the appendix
Ileocecal sphincter controls flow of contents from ileum into colon.
Gastrin leads to relaxation of the ileocecal sphincter

Appendix
Vermiform shaped blind end tube located posteromedial to caecum, at the end of tinea coli (longitudinal muscle). Form the base of the appendix
Found at McBurneys point. 2/3 between umbilicus and ASIS
Pre ileal - 1 (anterior)
Post ileal - 2 (posterior)
sub ileal - 3 (alond)
pelvic - 4
subcaecal - 5 (below caecum)
para caecal - 6 (lateral to caecum)
retro caecal - 7 (posteiror to caecum)

What is the blood supply of the appendix?
Appendicular artery which is a branch of posterior cecal artery

Colon
It has omentum appendices, teniae coli, haustra
Ascending - retroperitoneal up to hepatic flexure
Transverse - mesocolon up to splenic flexure
Descending - retroperineal up to sigmoid flexure
Sigmoid - intraperitoneal up to rectosigmoid junction
Supplied by SMA (right colic, middle colic) and IMA (left colic, sigmoid)
Lymphatic drainage follows blood supply eg Caecum, ascending colon and 1/3 of transverse colon drain to SM nodes.
Watershed area - marginal artery of Drummond

Rectum
Stores faeces, 15cm long begins at S3 superior third covered by peritoneum from 3 sides and middle third covered on anterior side
sympathetic - lumbar splanchnic - inferior hypogastric plexus parasympathetic - S2-S4

What is the blood supply of the rectum?
Supplied by Superior rectal (IMA), middle rectal (IIA) anastamoses with sup rectal and inf recta;, inferior rectal (pudendal)
Drains into superior/middle/inferior rectal veins where superior one drains into IMV thus postal system

Sup and Inf
What is the lymphatic drainage of the rectum?
Superior rectum drain into the pararectal nodes (which further drain into IM nodes)
Lower rectum drains into internal iliac nodes following the middle rectal artery

Anal canal
located at the anal triangle, right and left ischioanal fossainternal sphincter - involuntary external sphincter - voluntary puborectalis muscles

What are the features of the anal canal above pectinate line?
ABOVE pectinate line:
Endoderm origin (hindgut origin)
Columnar epithelium
organised into anal column and anal valve
supplied by SRA (branch from IMA)
What are the features of anal canl below pectinate line?
BELOW pectinate line
ectoderm origin
non keratinised stratified squamous epithelium until intersphincteric groove -
supplied by IRA (branch from the pudenal artery)
What is the lymphatic drainage of the lower half of the anal canal?
Drains into medial group of superficial inguinal nodes
What is the nerve supply of the anal sphincters?
Involuntary internal sphincter: sympathetic fibres from the hypogastric plexus
Voluntary external sphincter: Inferior rectal nerve (branch of pudenal nerve)
What is the rectal veins contribution to the porto-venous anastamosis
Superior rectal vein drains into IMV which drains into splenic vein into portal vein
Inferior rectal vein drains into systemic system
Liver - surface
Intraperitoneal organ
4 ligaments - falciform ligament (ligamentunm teres - umbilical vein), coronary ligaments, triangular ligaments, lesser omentunm (hepatoduodenal/hepatogastric)
3 recesses - subphrenic, subhepatic and morison’s pouch
2 supply - hepatic portal and systemic

Liver lobal anatomy
2 lobes divided by falciform ligament: Large right lobe and small left lobe
- *Right lobe is further divided into 2 lobes:**
- *Caudate** - separated by IVC and ligamentum venosum (remnant of ductus venosus)
Quadrate - separated by ligamentum teres (umbilical vein) and lies with the gall bladder anatomically part of right but functionally part of left lobe
Can also be divided in 8 hepatic segments

What is the anatomy of portal canals?
Lie in between the lobules of the liver
Contains branches of hepatic artery, portal vein and a tributory of a bile duct

Gall bladder
Located at L1
Stores bile, connected through the cystic duct and joins the CBD
Fundus - body - neck - Hartmann’s pouch - cystic duct
Body lies in contact with visceral surface of the liver
Supplied by cystic artery (branch of hepatic artery)
Vagus nerve stimulates as well but main stimulant is Cholecystokinin

Biliary tree
Right and left hepatic duct
Common hepatic duct (+ cystic duct )
Common biliary duct (+ pancreatic duct)
Ampulla of Vater

What is the ampulla of Vater?
Combination of the Bile duct and pancreatic duct

What is the function of the gallbladder?
When digestion not taking place sphincter of oddi remains closed and bile accumulates in gallbladder
Entrance of fat into duodenum causes release of cholecystokinin from mucous membrane - this causes gallbladder to contract
Sphincter of oddi is then relaxed
Pancreas
Retroperitoneal
Exocrine and endocrine organ
Endocrine: insulin & glucagon
Exocrine: Secretions which hydrolyse protein, fats and carbohydrates
Lies posterior to SMA/SMV
Tail is closely related to spleen via splenic artery and splenorenal ligament

Where does the pancreatic duct drain?
Pancreatic secretions begin in the tail and run the length of the gland - opens into second part of the duodenum at the middle with the bile duct on the major duodenal papillae
Accessory duct when present drains the upper part of the head - opens into minor duodenal papillae (sup to maj. papillae)

What is the blood supply of the pancreas?
Blood supply is pancreatic branch of splenic artery.
Blood supply to head is from Sup. pancreatoduodenal (coeliac trunk) and Inf. pancreatoduodenal (SMA)
Venous drainage is via SMA branches into hepatic portal vein

Spleen
Immunological & haematological organ
Intraperitoneal Ligaments - splenorenal ligament, gastrosplenic ligament
7 ounces (200g), ribs 9-11
Splenic artery has segmental supply thus subtotal resection is possible - branch of coeliac trunk

Adrenal glands
Retroperitoneal organ, endocrine organ
Cortex: zona glomerulosa (mineralocorticoid), zona fasciculata (glucocorticoid), zona reticularis (sex hormones)
Medulla - chromaffin cells - adrenaline

Blood supply of adrenal glands
Supply - 3 arteries:
Superior adrenal - inferior phrenic artery
Middle adrenal - aorta
Inferior adrenal - renal artery

What is the venous drainage of the adrenal glands?
Right side: IVC
Left side: Renal vein

Kidneys
Retroperitoneal organ - T12-L3
Clear toxin from circulation & maintain circulatory homeostasis (volume & electrolyte)
Right kidney lies slightly lower than left kidney because large size right lobe of liver.
Medulla - renal pyramids - calyx - pelvis - ureter
Supply - renal artery - interlobar - arcuate
Drains into renal veins (left side drains adrenal & gonadal as well)

What is the structure of the coverings of the kidney and the kidney?
Coverings:
Fibrous capsule
Perirenal fat
Renal fascia
Pararenal fat
Renal structure:
Cortex
Medulla

What level do the kidneys lie at?
Left kidney: T12 - L3
Right kidney: slightly lower
Blood supply of the kidneys?
Renal artery arises from the aorta at the level of L2
Renal vein anterior to artery at the hilum.

What is the blood supply of the ureter?
Blood supply is split into three sections:
Upper end: Renal artery
Middle portion: Testicular / ovarian artery
Pelvis: Superior vesical artery

What is the course of the ureter and points of constriction?
Leaves the hilum posterior to vessels
Runs down on psoas muscle - adjacent to transverse tips of lumbar vertebrae
- *3 constrictions along course:**
- *Renal pelvis**
Crosses pelvic brim (crosses over CIA)
Pierces the bladder wall

What is the lymph drainage of the ureter?
Lateral aortic nodes and the iliac nodes

Aorta - Abdominal branches
In Case My Students Really Love Games I‘m Monopoly
Inferior phrenic
Coeliac(T12)
Middle adrenal
SMA(L1)
Renal
Lumbar
Gonadal (L2),
IMA(L3),
Median sacral (L4),

Coeliac trunk
T12
Left gastric (oesophageal branches)
Splenic (L gastroepiploic (greater curve stomach), short gastric arteries
Common hepatic artery : gives rise to R gastric, R + L hepatic, cystic and sup. gastroduodenal (head of panc.)

Superior mesenteric artery
L1
Major branches:
Inferior pancreaticoduodenal artery
Jejunal & ileal arteries (forms the anastamotic arcades)
Right & middle colic
Ileocolic (gives rise to branches supply illeum, caecum, colon and appendix) - can ligate appendicular artery in appendix

Inferior mesenteric artery
L3, supplies the hindgut, retroperitoneal main branches:
Left colic (from distal 1/3 of transverse colon)
Sigmoid
Superior rectal
Anastomosis with middle colic - Marginal artery of Drummond

Inferior vena cava
Formed by CIV at L5
Drains - Lumbar veins, right gonadal, right adrenal, right and left renal, inferior phrenic and hepatic veins

Portal venous system
Drains the GIT content and supplied to liver
At L1 Formed by SMV & Splenic
Drains R&L gastric, cystic, para-umbilical veins
Splenic - short gastric, left gastroomental, pancreatic, IMV
SMV - right gastroomental, anterior and posterior inferior pancreaticoduodenal, jejunal, ileal, ileocolic, right & middle colic

Portosystemic anastomosis
Oesophageal - left gastric and azygous
Rectal - superior rectal and inferior rectal
Retroperitoneal - mesenteric to reperitoneal
Paraumbilical - portal vein to anterior abdominal wall

What is the nerve root blood supply at the
Xiphoid process
Umbilicus
Pubis
Xiphoid process: T7
Umbilicus: T10
Pubis: L1

Where does the superior epigastric artery run and what does it supply?
Superior epigastric artery:
terminal branch of int. thoracic artery
Enters upper part of rectus sheath between sternal and costal edges of the diaphragm

Where does the inferior epigastric artery run, what is its origin and what does it supply?
Inferior epigastric artery:
Branch of external iliac artery just above inguinal ligament
Runs upward and medial along medial side of deep inguinal ring
Pierces fascia transversalis to enter rectus sheath ant to arcuate line
Supplies:
Lower central part of abdominal wall

Where does the deep circumflex iliac artery supply, what is it a branch of and where does it run
Deep circumflex iliac artery:
Branch of ext. iliac above inguinal ligament
Runs upward and laterally to ASIS
Supplies lower lat. part of abdo wall

What is the lymphatic drainage of the superficial abdominal wall

What is the lymphatic drainage of the testes?
Testicular lymph vessels ascend through the inguinal canal and pass posterior abdominal wall to reach para-aortic lymph nodes

Common facts indirect inguinal hernia?
Remains of patent processus vaginalis therefore congenital in origin
More common than direct inguinal hernia
M>F
R>L
Common facts direct inguinal hernia
Rarer than indirect hernias
Common in old men with weak abdominal muscles
Hernial sac bulges through posterior wall of inguinal canal medial to inferior epigastric vessels
Neck of hernial sac is wide
Lies above and medial to pubic tubercle
What is a spigelian hernia?
Hernia of linea semilunaris
Occurs through aponeurosis of the transversus abdominus just lateral to lateral edge of rectus sheath
Occurs just below level of umbilicus

What is a Lumbar hernia and where does it occur?
Rare
Occurs through weakness in Lumbar triangle in posterior part of abdominal wall
What is a paramedian incision?
Advantages and disadvantages

What is a pararectus incision?
Advantages & Disadvantages
Anterior wall of rectus sheath incised lateral margin of rectus muscle
Rectus retracted medially - exposing segmental nerves entering its posterior surface
Posterior wall of the sheath is then incised
Disadvantage:
Opening is small
Any longitudinal extension will cause post operative rectus muscle weakness

What is a midline incision?
Advantages and disadvantages?
Made through Linea Alba
Rapid method of gaining access to the abdomen.
Does not damage blood vessels or nerve supply
Can be extended into T shape incision

Pfannestial incision
Obstetric access
Rectus muscle should be retracted
If sufficient access not gained from retraction
If the muscle is to be transected, the inferior epigastric artery and vein on the lateral border of the muscle must be clamped, incised, and ligated prior to cutting the muscle.

What is McBurney’s incision?
Obliue skin incision 5cm above and medial to ASIS
External & internal obliue and transversalis muscles are incised or split in the line of their fibres
Disadvantages
poor vision - should only typically be used when there is no doubt as to diagnosis

How does the greater omentum help with localising infections?
Inflammatory exudate causes the omentum to adhere to the appendix and wrap itself around the organ
How does peritoneal fluid move around the abdomen particuarly in infection?
Peritoneal cavity is divided into upper part within the abdomen and lower part in the pelvis
Abdominal part is further subdivided by spaces and reccess
Attachment of transverse mesocolon and mesentery of the small intestine hinders the movement of infected peritoneal fluid from upper part to lower part of peritoneal cavity
Infection can spread from the peritoneum to the lung pleura via the diaphramatic lymph vessels.
What drains to the preaortic lymph nodes?
Preaortic lymph nodes:
Celiac
Superior Mesenteric
Infeior Mesenteric
Drains lymph from GI tract
From lower 1/3 oesophagus to halfway down anal canal
From spleen, pancreas, gallbladder and greater part of liver

What drains to the para-aortic lymph nodes
Lymph from kidneys and supraadrenals
From testes in males and from the ovaries, uterine tubes and fundus of uterus in females.

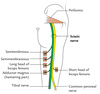
What is in the lumbar plexus & what nerves originate there?
Formed in the psoas muscle from the anterior rami of upper 4 lumbar nerves
I (twice) get laid on friday
All lateral other than genitofemoral (ant) and obturator (medial)
Iliohypogastric
Ilioinguinal
Genitofemoral nerve (anterior)
Lateral cutaneous nerve of thigh
Obturator nerve (medial)
Femoral nerve
What are the nerve root values of the lumbar plexus?
I (twice) Get Laid On Fridays - nerves
2 from 1, 2 from 2, 2 from 3
Iliohypogastric (L1)
Ilioinguinal (L1)
Genitofemoral (L1, L2)
Lateral cutaneous nerve of thigh (L2, L3)
Obturator (L2, 3, 4)
Femoral (L2 , 3, 4)

What is the sacral plexus formed from?
L4, 5 S1, 2, 3, 4
On anterior surface of piriformis muscle
- *superior gluteal nerve** L4/5 S1
- *Inferior gluteal** L5 S1/2
- *Posterior femoral cutaneous** S1/2/3
- *Pudendal** S2/3/4
- *Sciatic** L4, 5, S1, S2, S3

What is the route of the superior gluteal nerve?
L4, 5, S1
Passes superior to the piriformis via the greater sciatic foramen
Accompanied bu sup. gluteal vein and artery

What is the course of the inferior gluteal nerve?
L5, S1, S2
Leaves pelvis via greater sciatic foramen inferior to piriformis muscle
Motor function - gluteus maximus
What is the route of sciatic nerve
L4 - S3
2 components:
- *Fibular** (dorsal division L4 - S2)
- *Tibial** (ventral divisions L4 - S3)
Formed on anterior aspect of piriformis muscle
What muscles are innervated by the tibial componenet of the sciatic nerve?
Muscles in:
Posterior compartment of thigh (other than SH of Biceps femoris - innervated by fibular portion of sciatic nerve)
Hamstring component of adductor magnus
Posterior compartment of leg
Muscles in sole of foot
What muscles are innervated by fibular portion of sciatic nerve?
Short head of biceps femoris
Anterior and lateral compartments of the leg & extensor digitorum brevis muscle

What is the origin / route of the posterior cutaneous nerve of the thigh?
S1, 2, 3
Leaves pelvis via greater sciatic foramen. Enters inferiorly to piriformis muscle
Runs down back thigh to knee
Innervates skin of perineum, posterior surface thigh and leg.

Origin of the pudenal nerve & root?
S2, 3, 4
Leaves via greater sciatic foramen and then loops around sacrospinus ligament to enter pelvis via lesser sciatic foramen
Motor: Innervates EUS, EAS, levator ani muscle
Sensory: Innervates penis, clitorus and nerves of skin

What is Hesselbachs triangle?
The inguinal triangle is located within the inferomedial aspect of the abdominal wall. It has the following boundaries:
- *Medial** – lateral border of the rectus abdominis muscle.
- *Lateral** – inferior epigastric vessels.
- *Inferior** – inguinal ligament.

What are the borders of Calots triangle?
Inferiorly: Cystic duct
Medially: Common Hepatic duct
Superiorly: Inferior surface of the Liver
Cystic artery runs through Calots triangle


