9 HF- pressure volume loops Flashcards
(24 cards)
How do you calculate cardiac output?
CO = HR x SV
What are 3 major determinants of stroke volume?
- contractility
- preload
- afterload
How is cardiac output a function of preload?
- The more a normal ventricle is distended during diastole, the greater the amount of blood ejected during the next contraction
- Frank-starling relationship
- Higher preload= higher SV
- preload measured as EDV/EDP (indicates degree of stretchin at the end of diastole)
How do you calculate wall stress?
- Law of LaPlace
- σ = P x r / 2h
- P=ventricular pressure, r=ventricular radius, h=ventricular wall thickness
- Wall stress rises in response to higher pressure load (HTN) or increased chamber size (e.g. dilated LV)
- Increased wall thickness is a compensatory mechanism to reduce wall stress
Describe afterload
- The resistance the ventricle must overcome to empty its contents
- Formally defined as the ventricular wall stress that develops during systolic ejection
- Estimated by the LaPlace relationship
What affects the contractility of the heart?
Contractility accounts for changes in myocardial force for a given set of preload and afterload conditions
**dependent on chemical and hormonal influences

Describe a pressure-volume loop

How does changing preload affect the pressure-volume loop?
Increased preload= increased EDV
(ESV stays the same so SV increases as well)

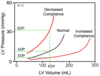
How does a change in compliance affect the pressure-volume loop?
Increased compliance= decreased slope (more stretch results in less pressure for the same EDV)
How does changing afterload affect the pressure-volume loop?
- Increased afterload increases pressure generated during ejection
- More work expended to overcome resistance to eject
- ESV is greater but EDV stays the same
- increased afterload= decreased SV (EDV-ESV)
- ESPVR= end systolic pressure volume relationship (linear)

How does a change in contractility affect the pressure volume loop?
- Slope of the ESPVR line is a function of contractility
- Increased contractility= steeper slope
- Therefore the ventricle empties more completely as contractility increases, resulting in a smaller ESV (thus, increased SV)

What factors affect ESV?
ESV depends on the afterload and contracitliy, but NOT preload
What are the 3 main pathophysiological reasons for heart failure?
Reduced EF:
- Impaired ventricular contractility
- Increased afterload
Preserved EF:
- Impaired relaxation and filling

Describe heart failure with reduced ejection fraction
- Ventricle has diminished capacity to eject blood because of impaired contractility or pressure overload
- Loss of contractility from:
- myocyte destruction
- abnormal myocyte function
- fibrosis
- Pressure overload= increased resistance to outflow= impaired ejection fraction

Describe heart failure with preserved ejection fraction
- usually abnormalities in diastolic function
- impaired early relaxation
- increased wall stiffness
- possible causes:
- acute ischemia
- hypertrophy
- fibrosis
- restrictive cardiomyopathy
- pericardial diseases
Describe some causes of right sided heart failure
- cardiac causes
- left sided heart failure
- pulmonic valve stenosis
- right ventricular infarction
- pulmonary parenchymal diseases
- COPD
- interstitial lung disease (sarcoidosis)
- chronic lung infection/bronchiestasis
- pulmonary vascular diseases
- pulmonary embolism
- pulmonary arteriolar HTN
How can frank starling mechanisms worsen heart failure?
- Normally, body increases EDV to increase SV
- However, in heart failure an increase in EDV cannot significantly increase SV and instead causes pulmonary congestion
- Heart failure= severely depressed contractile function

How does neurohormonal activation affect heart failure?
- Activation results in…
- Symp/RAAS/antidiuretic activation
- increases peripheral vascular resistance (maintaining perfusion of organs during reduced CO)
- promotes Na/water retention -> increases vascular volume -> increases preload -> maximizes CO (frank-starling)
- Initially benefitial, but continued activation ultimately proves harmful

What are the natriuretic peptides?
- atrial (ANP) natriuretic peptide
- released from atrial cells in response to stretch
- B-type (BNP) natriuretic peptide
- produced by ventricular myocardium in response to hemodynamic stress (HR/MI)
- BNP levels used to gauge HF severity
- degraded by neprilysin
- OPPOSE actions of other hormone systems
- promote Na/water excretion
- vasocilation
- inhibit renin secretion
Compare the symptoms of left and right heart failure
- left
- dyspnea
- orthopnea
- paroxysmal nocturnal dyspnea
- fatigue
- right
- peripheral edema
- right upper quadrant disconfort (because of hepatic enlargement)
Compare the physical findings of left and right heart failure
- left
- diaphoresis
- tachycardia, tachypnea
- pulmonary rales
- loud P2, S3/S4 gallop
- right
- JVD
- hepatomegaly
- peripheral edema
Describe the New York heart association (NYHA) classification of heart failure
- class I= mild
- cardiac disease by no physical symptoms
- class II= mild
- slight limitation of physical activity (dyspnea/fatigue with moderate exertion)
- class III= moderate
- marked limitation of physical activity (dyspnea with minimal exertion)
- comfortable only at rest
- class IV= severe
- severe limitiation of activity, symptoms present at rest
What are some diagnositc studies for heart failure?
- chest radiograph
- changes in appearance of pulmonary vasculature (Kerley lines)
- evidence of interstitial/alveolar edema
- cardiomegaly
- serum BNP
- ECG
What is the prognosis of heart failure?
- 5 year mortality= 45-60% (severe symptoms= 40% 1 year survival)
- mortality due to heart failure and also sudden cardiac death (increased risk for arrhythmias)
- similar prognosis with preserved and reduced EF


