8 Genetic Arrhythmias Flashcards
What are 7 inherited arrhythmias?
- Long QT syndrome (LQTS)
- Brugada syndrome (BrS)
- Catecholaminergic polymorphic ventricular tachycardia (CPVT)
- Short QT syndrome (SQTS)
- early repolarization
- sudden unexplained death syndrome
- idiopathic V fib
Describe the multimeric structure of ion channels
- alpha units are pore forming/mediate currents
- beta units are regulatory
- often encoded by separate genes!
What are some common findings in inherited arrhythmias?
Patients may be affected at any age, presenting with:
- syncope
- sudden cardiac death
- SIDS
- other vague symptoms (hypotension, brady/tachy, palpitations, angina, dyspnea, dizziness, sweating)
- distinct EKG patterns clarify disorders
Describe LQTS
Long QT syndrome;
- clinically identified by prolonged QT, T wave abnormalities, and Torsades de pointes
- presents with syncope with exertion, SCD, and possibly seizures
- as QTc interval increases, risk for cardiac event goes up (positive linear relationship)
What are some causes of LQTS?
- acquired= more common
- MI, myocarditis, cardiomyopathy
- electrolyte imbalances
- autonomic and drug influences
- hypothermia
- congenital
- Romano-Ward syndrome (RWS)
- Jervell and Lange-Nielson syndrome
What are the top 3 mutated genes that can cause LQTS?
- KCNQ1 (LQTS1) 30-35%
- broad T wave
- exercise/emotion triggers event
- KCNH2 (LQTS2) 25-30%
- notched T wave
- exercise/emotion, postpartum, sleep triggers
- SCN5A (LQTS3) 5-10%
- long ST segment, small T wave
- sleep triggers event
Describe Jervell and Lange-Nielson Syndrome
- congenital syndrome that can cause
- QT prolongation
- deafness
- increased risk for SIDS
- autosomal recessive
- most commonly LQTS type 1 (KCNQ1 gene)
Describe LQTS genetic testing
- current detection rate= 75% (25% of families don’t have a detectable gene mutation)
- negative test does NOT rule out LQTS!
What is the treatment for LQTS?
- avoid QT prolonging medications and strenuous exertion
- replete electrolytes
- beta blockers and antiarrhythmic medications (can tailor therapies to specific mutation)
- pacemakers and implantable cardioverter defibrillators (ICDs)
- left cardiac sympathetic denervation (LCSD) for patients with breakthroughs on BBs/ICD
- ablation of left stellate ganglion
Describe Brugada syndrome
- more common in southeast Asia, more prevalent in males
- cardiac conduction abnormalities, ST elevation in V1-3
- high risk for ventricular arrhythmias can result in SCD
- present with angina, palpitations, labored breathing during sleep, syncope, VT, SIDS
- several genes associates with BrS (difficult to diagnose… current detection rate 25-30%)
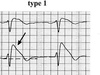
How do you diagnose Brugada syndrome?
- “Coved” ST segment elevation followed by negative T wave
- Plus at least one of the following
- documented VF/PMVT
- family history of SCD or coved EKG
- inducible VT at EPS
- syncope from arrhythmia cause
- nocturnal agonal respiration
What can create Brugada-like EKG patterns?
- antiarrhythmic drugs (IA, IC)
- antianginal drugs (Ca blockers, nitrates)
- psychotropic drugs (tricyclics, phenothiazines, SSRIs)
- cocaine
- alcohol
**Many differential diagnoses for Brugada-like EKGs
How can you treat Brugada syndrome?
- avoid triggering drugs/alcohol
- treat fevers immediately
- ICD is the only proven effective treatment
Describe CPVT
Catecholaminergic Polymorphic ventricular tachycardia
- triggered by exercise or acute emotion
- mean onset 7-12 years
- structurally normal heard and often normal resting EKG
How do inherited arrhythmia conditions often present?
- sudden cardiac arrest/death
- syncope
- palpitations
**often absence of structural heart disease!


