8 - Haemostasis Flashcards
What is haemostasis?
The process of stopping haemmoraghe, needs blood vessels, platelets, coagulation factors and anticoagulant factors

What are the steps of haemostasis?
- Severed blood vessel (artery not vein) contracts to decrease the pressure downstream
- Primary haemostatic plug of activated platelets forms at the hole sticking to the blood vessel wall and connective tissue outside it. Seconds to minutes.
- Secondary haemostatic plug forms as fibrin filaments stabilise platelet plug into blood clot. In about 30 mins 4.
- Fibrinolysis and replacement with granulation tissue or scar

What are platelets activated by?
- Collagen surfaces
- ADP (released by activated platelets and injured RBC)
- Thromboxane A2 (aggregator from activated platelets)
- Thrombin
What are the different steps of platelets forming a primary plug?
1. Adhesion: Damage to vessel wall exposes von Willebrand factor on the subendothelial basement membrane that platelets adhere to with collagen
2. Activation: secrete granules of ADP, thromboxane, coagulation factors, fibrinogen to activate other platelets
3. Aggregation: change shape to spheres and cross link to form platelet plug that is temporary and weak

How does aspirin work as an anti-coagulant?
Inhibits cyclooxygenase which is involved in produced thromboxane A2
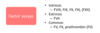
To form a fibrin clot, what factors are needed, and what is essential for their production?
Vitamin K needed for the ones with stars

What are the two pathways of clotting?
Intrinsic: No vessel needs to be broken for it to occur, factors are contained in the blood and are triggered by a negative surface
Extrinsic: Needs tissue factor which is present outside of the blood. Triggered by thromboplastin released from damaged cells adjacent to area of haemorraghe

What are the natural anti-coagulants in the body?
- Anti-thrombin II, Protein C, Protein S
- Dilution of clotting factors

How is the vascular wall involved in haemostasis?
- Contracts when artery damaged
- Releases Von-Wilebrand and tissue factor activating clotting
- Release tissue plasminogen activator and thrombomodulin to activate protein C to oppose clotting
Why and how do blood clots get smaller?
- Platelets in the clot die and pling to fibrin and pull by their actin-myosin filaments
- Pulls together sides of the wound and toughens clot by squeezing out fluid

How is fibrinolysis activated, what is the process of it?
- Initiated at the same time as clotting
- Activated by streptokinase, tpa, urokinase
- D-dimers are FDP’s

How can you treat someone with a thrombus?
- Give them streptokinase but only once as it is antigenic
- Give them tissue plasminogen activator multiple times
What does a high blood FDP indicate?
- Conditions with thrombosis, e.g DIC, DVT, PE

After surgery why are you at risk of DVT?
- Immobility so stagnant blood
- Less fibrinolytic activity for 7 to 10 days
What are different ways of measuring blood clotting?
- Prothrombin Time PT: measure extrinsic pathway and common pathway so VII, X, prothrombin, fibrinogen
- Activated Patial Thromboplastin time APPT: measure intrinsic pathway and common pathway, VIII, IX, XII, V, X, XI, prothrombin and fibrinogen

What factors are involved in the extrinsic, intrinsic, and common pathways?
What is haemophilia A?
- X-linked recessive lack of factor VIII
- Mild symptoms with 6-50% normal function, majoy with less than 1%
- Easy bruising and haemorraghe into muscles and joints 12-24 hours after trauma or surgery
- Joint deformities can occur with haemarthrosis

Why do you not see petechiae in haemophilia A?
Petechiae results from blood leaking from capillaries which is normally due to malfunction of the number of platelets

How do you diagnose and treat haemophilia A?
- Normal platelet count, bleeding time (platelet activity measure) and PT
- Prolonged APTT
- Low factor VIII assay
- Infuse with remcombinant VIII

What is haemophilia B?
- Factor IX defiency with similar presentation to haemophilia A
- X-linked recessive, same blood results as haemophilia A, e.g prolonged APPT but different enzyme assays
- Treat with recombinant IX

What is Von Wilebrand disease?
- Range from asymptomatic to severe bleeding
- Autosomal dominant
- Lack of vWF so low VIII and issue with platelet aggregation
- Increased APPT and bleeding time
- Often superficial mucosal bleeding

What are some symptoms of vessel wall abnormalities and some disease that cause theses?
- Ehler’s Danlos
- Hereditary Haemorrhagic Telangiectasia (dilated microvascular swellings rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation in the skin, mucous membranes, and often in organs such as the lungs, liver, and brain)
- Steroids
- Scurvy
- Infections

How does thrombocytopenia appear clinically and with blood tests?
- Prolonged bleeding time, normal PT and APPT as these assessing clotting cascade not platelets
- Spontaneous bleeding from small vessels, e.g skin, GI, intracerebal bleeding
- Appears as petechiae

What are the different causes of thrombocytopenia?
1. Decrease platelet production (bone marrow infiltration, drugs etc)
2. Decreased platelet survival (autoimmune)
3. Sequestration (splenomegaly)
4. Dilution (e.g blood transfusions)

What blood tests are affected by DIC?
- Raised PT and APTT
- Low fibrinogen
- Raised D-dimers
- Anaemia due to microangiopathic haemolytic anaemia as squeezing past microthrombi

What are some conditions that can be caused by DIC?
Microthrombi and haemorraghing can lead to:
- Gangrene of skin
- Renal failure
- Gastrointestinal ulceration
- Bleeding intracerebally, gastrointestinally
- Petechiae
- Haematuria

How do you treat DIC?
- Triggered by things such as sepsis, severe trauma, burns, complications of child birth, snake bite etc due to systemic activation of coagulation with factors
- Treat underlying cause, transfudse platelets and plasma, heparin

Why would sepsis and trauma cause DIC?
- Gram-negative bacteria could produce endotoxin that activated clotting
- Trauma causes release of thromboplastin (tissue factor)
What is thrombophilia?
- Inherited or acquired defect in haemostasis so predisposition to thrombosis
- Factor V Leiden, anticoagulant deficiencies, antiphospholipid syndrome
- Family history is key



