28 . Tumors Flashcards
Generally, how do metastatic tumors present in the CNS?
- Multiple, well-circumscribed lesions, most often at the grey-white junction.
- Top 3 metastic cancers are: lung, breast and kidney cancers.
Generally, do primary malignant tumors of the CNS metastasize?
- No, they are locally destructive.
- Rarely metastasize.
What are the key cells in the brain that produce tumors?
- Glial cells (astrocytes, oligodendrocytes, ependymal cells); 50%= supports and surrounds neurons
- Neurons (50%)
- Meningothelial cells = surround brain
Astrocytes produce what tumors in kids and adults
- Kids = Pilocytic astrocytoma
- Adults = Glioblastoma (MC CNS tumor in adults)

Oligodendrocytes produce what tumors and in who are they MC in
Oligodendromas = adults

Ependymal cells produce what tumors and in who are they MC in
Ependymomas = children

Neurons produce what tumors and in who are they MC in
Medulloblastomas (from neuroectoderm) = children

Meningothelial cells produce what tumors and in whome?
Meningioma = adult females

Where are brain tumors most common in kids and adults?
- Kids => infratentorial (posterior fosssa): cerebelleum & brainstem
- Adults => supratentorial (above tentorium)

What are the MC brain tumors in children?
MC infratentorial
- Astrocytoma
- Medulloblastoma
- Ependymoma
- Craniopharyngioma
What are the MC brain tumors in adults?
MC supratentorial
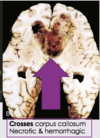
- Glioblastoma **
- Meningioma
- Schwannoma
- Oligodendroma
- Hemangioblastoma
- Pituitary Adenoma
If you have a new onset of a seizure in a adult, think ________.
Brain tumor
Which grade of tumor is considered infiltrative?
Grade II
In which decade of life are Grade II, III, and IV Astrocytomas found?
- Grade II: usually 30-40s
- Grade III: usually 50s
- Grade IV: usually 60s +
What are gliomas?
MC group of primary brain tumors: astrocytomas, oligodendrogliomas, ependymomas
Pattern of growth and spread in tumors in CSF
- Most infiltrate extenselively, even if benign, displaying malignant behavior
- Spread via CSF, but even most malignant gliomas RARELY metastasize ouside CSF
What are Pilocytic Astrocytomas?
- Usually occur when?
- Where in the brain do they typically occur?
Low-grade benign tumor of astrocytes that are the MC brain tumor in chidren; slow growing and prognostically favorable
- 0-20 (First 2 decades)
- Cerebellum, floor/walls of 3rd ventricles, between hemispheres

What grade of tumor is a Pilocytic Astrocytoma?
Benign I/IV; they commonly extend into subarachnoid space, but not sign of aggression and optic nerve lesions
What are the distinguishing morphological characteristics of Pilocytic Astrocytomas?
- Well-circumscribed, CYSTIC tumors w/ a mural nodule
- - Biphasic pattern: loose glial cells w cystic changes and dense piloid tissue
- Low cellularity
- - Hair-like cells w/ long bipolar processes
- - Rosenthal fibers = long-standing gliosis
- - Eosinophilic granular bodies (EGBs)

Marker of Pilocytic astronoma
GFAP

what do these findings signify in pilocytic astronomas?

- EGB = PAS + protein drops that mark a slow growing, low grade tumor that is prognostically favorable
- Rosenthal fibers = long standing gliosis
Which disease predisposes patients to Pilocytic Astrocytomas and due to what?
NF-1 (neurofibromatosis 1) due to functional loss of neurofibromin
Most common presenting signs and symptoms of Infiltrating Astrocytomas?
- Seizures
- HA
- Focal neurologic deficits
related to the site of involvement
Infiltrating astrocytoma range from what kind of tumors?
- Grade II/IV: Diffuse astrocytoma
- Grade III/IV: Anaplastic astrocytoma
- Grade IV/IV: Glioblastoma (this is malignant)