24 - Diagnostics for Detection of Infectious Diseases in Respiratory Tract Infections Flashcards
(56 cards)
WHat are teh 2 forms of infection for mycobacterium tuberculosis?
latent (90%) and active (10%)
What are the symptoms for latent TB and how do you test for it?
Asymptomatic, noncontagisou
Test the patient’s T cells for reactivity against M tuberculosis (TB Quantiferon)
What are the symptoms of active tuberculosis? How do you test for it ?
persistent cough, fever/chills, night sweats
upper lobe predominant nodular disease with areas of bronchiectasis
contagious
*test by culturing for mycobacterium in sputum
why would doing PCR for TB of patietns blood not help diagnose TB?
TB usually isn’t found in the blood
Who is at risk of progressing from latent Tb to active TB and what is the risk? How do we prevent this progression?
immuncompetent: 10% lifetime
immunocomromised (ex AIDs): 10-15%/year
prevent progresion
What is the Mantoux tuberculin skin test?
- TST/PPD
- Tuberculin purified protein derivative (PPD) subcutaneous
- read between 48-72 hours looking at area of induration, inexpensive screen

How do we interpret the TST/PPD?
Look at area of induration!
- interpretation stratified by risk/exposure
- >5mm high risk
- HIV, recent contact with TB+, suppressed (prednisone, TNFa inhibitors)
- > 10nm medium risk
- recent immigration from endemic region, IV drug users, laboratory/healthcare workers
- >15mm low risk
- low risk populations, pre-employment screening
- >5mm high risk
What is the sensitivity and specificity of the TST/PPD test?
- Sensitivity: 85-95%
- false negative in patients with HIV. immunosuppression or overwhelming infection (anergic)
- Specificity 80-90%
- false positive if had BCG, cross-reactivity with other Myco spp.
- somehwat subjective (induration vs erythema)
What is the Quantiferon (IGRA) test for TB?
- uses TB specific peptides (ESAT-6, CFP, TB7.7) and measures T-cell mediated IFN-y response against M. tuberculosis
What are the advantages of the Quantiferon TB test?
- specific for MTB: not cross reactive with BCG, M kansassii, M sulgai, M marinum
- in-tube, whole blood test, no need for patient follow-up
- automated, internal standard curve on each plate
- sensitivity 75-85% (in culture confirmed cases)
- specificity >99%
What are the disadvantages to the Quantiferon test?
- 50%/test reagent stability
- pre-analytic steps contribute to variablity
- collection (0-16 h window for incubation), transport (RT), mixing
- 5-30% unresolved rate
- package insert for TNFa inhibitors
- no equivocal range, no risk based interpretation
Which test TST/PPD or Quantiferon (IGRA) is better for people from TB endemic areas
Quantiferon! If they are from an endemic rea they likely received the BCG vaccine which will give them a false positive TST/PPD
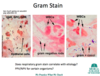
What is the advantage os using a flourescent stain versus a non-fluourescent stain?
the fluorescent stain allows the lab to identify organisms that are present in lower quantities
the fluorescent stain allows the technologist to “pick out” organisms from a clinical matrix
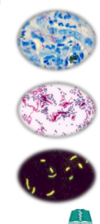
What are the 2 methods to the direct exam “Smear” test? What are benefits to each? what are the major drawbacks?
- Acid-Fast
- cheap, easy
- Ziehl-Neelson/Kinyoun stain
- carbol fischin (heat or phenol to increase uptake)
- decolorize
- methylene blue or brilliant greeen
- carbol fischin (heat or phenol to increase uptake)
- Auramine-Rhodamine (fluourescent)
- binds acid fast cell wall
- more sensitive, still fairly cheap
- requires fluourescent microscope
major drawbacks: specificity…species specific morphology. You know it is mycobacterium, but not necessarily mycobacterium tuberculosis
So the Quantiferon will tell us that it is mycobacterium, but not if it is mycobacterium tuberculosis. How can we test for sure that it si mycobacterium tuberculosis?
PCR! Very commonly used, even more specific would be to do sequencing (which will also tell you about resitance)
You can also do a culutre, but this takes 8 weeks to get results!
What are some advantages of PCR vs smear or culture when looking for mycobacterium tuberculosis?
- MUCH faster! only 2 hours vs 19-25 days culture
- important bc potentially can save money, make appropriate treatment decision, and get patients out of isolation faster!
- specificity: much more specific than smear positive
What are the disadvantages to doing PCR to test for mycobacterium tuberculosis?
- money! especially in resource limited countries where TB is endemic. It is cheap, but not when you have to do a TON of them
- it requires electricity
- it requires technical expertise
WHat is the gold standar in TB testing?
culture!
- Medium
- Lowstein-Jensen
- egg, potato flour, malachite green, glycerol
- suitable for most mycobacterium (toxic to RGM, M.bovis)
- may liquify if bacterial contamination is high
- Middlebrook
- defined medium
- more permissive-bacteria grow faster (not toxic to RGM)
- it is clear aka easier to spot colonies
- can be agar or broth
- Lowstein-Jensen
What is a phenotypic antimicrobial suseptibility testing (AST)?
- broth or agar methods
- drug concentration
- single concentration “critical concentration”
- inhibitory 95% of wild type isolates
- single concentration “critical concentration”
- hold time
- 3 weeks
- required for all strains
- test initial isolate, repeat if patient fails to concert to smear negative in 3 months
- test only first line drugs unless MDR, then test second line
not done as often anymore bc it is slow and molecular AST is fast! (sequencing or PCR)
What is a molecular antimicrobial suseptibility test?
sequence the bacteria or PCR for resistance genes
What is DNA sequencing?
the process of determining the precise order of nucleotides within DNA molecule
What is Sanger sequencing?
- “PCR on steroids”
- Sequencing that is done primarily by hand. Is much slower than next gen
- take a sample, break apart DNA and add small primers, assign each letter A, T, G etc a color and determine the sequence

what is Next generation sequencing? What are some advantages and disadvantages?
basically the same thing as Sanger sequencing but more automated! MUCH faster!
- Advantages
- much cheaper vs snager sequencing
- much more data-can sequence a human genome in a week vs 10 years with sanger
- can identify minor populations
- Disadvantage
- expensive
- time consuming
- difficult to assemble
What are the top 4 drugs to treat TB? How good are we at detecting their molecular resisitance via sequencing?
- Rifampin: mutation in rpoB
- detects 95-98%
- Isoniazid
- detects 95% of mutations
- Ethambutol: mutations in embB prevent binding of drug
- detects 80% of mutations
- Pyrazinamide
- detects 85% of mutations
so we are pretty good. some drugs have more possible mutations than others so we are better at detecting some drugs than others