13 - Large Intestine and IBS Flashcards
(26 cards)
Where is the large instestine and what is it’s main role?
- From the caecum to the anal canal
- Simple columnar
- Removes water from indigestible gut contents to make semi solid faeces
- Also synthesises vitamins, stores faeces and has a microbiome

How does the microbiome survive in the colon?
Ferments short chain fatty acids from dietary fibre, producing CO2, methane and hydrogen gas

Does the colon have a mesentry?
- Only the sigmoid and transverse colon
- Ascending and descending colon are secondarily retroperitoneal

What is the arterial supply to the colon?
- Mid gut portion from the SMA
- Hind gut portion from the IMA

What is the superior rectal artery?
A continuation of the IMA when it passes over the pelvic brim

What is the venous drainage of the colon?
- IMV joins splenic vein

What are some of the differences between the small and large intestine?
- Colon is shorter but wider (6ft and 6cm diameter)
- Colon has crypts not villi
- In colon external longitudinal muscle is incomplete and forms three bands of muscle called teniae coli which contract to form haustra

How is water absorbed in the colon?
- Aldosterone sensitive ENaC channels
- 1500mls enters colon but only 100mls excreted in faeces

What is inflammatory bowel disease?
A group of conditions characterised by idiotpathic inflammation of the GI tract, most commonly Crohn’s and UC

What are the key features of Crohn’s disease?
- Affects anywhere in GI tract from mouth to anus, mostly terminal ileum involved
- Transmural
- Skip lesions

What are the key features of ulcerative colitis?
- Starts in the rectum and works backwards so continuous
- Superficial mucosal inflammation
- Only in colon but if pancolitis can backwash to cause terminal ileum inflammation

What are some extra-intestinal manifestations of inflammatory bowel disease?
- Joint issues like arthritis
- Skin issues like erythema nodosum, pyoderma gangrenosum, psoriasis
- Liver problems like PSC
- Eye problems

What can be some causes of inflammatory bowel disease?
- Unknown but genetic risk if 1st degree relative
- Triggers can be antibiotics, smoking (Crohn’s), infections, diet

What would be a typical presentation of Crohn’s disease?
- Young female 15-30 most commom
- Multiple non-bloody loose stools a day
- Weight loss
- Right lower quadrant pain
- Joint pain
- Maybe a smoker
- Mildly anaemic
- Perianal inflammation
- Low grade fever

What is the gross and microscopic appearance of Crohn’s disease?
Gross:
- Skip lesions
- Cobble stone appearance (grout being ulcers)
- Transmural inflammation so narrowed lumen and thick wall
- Mucosal oedema
- Fistula to bowel/bladder/vagina/skin
Microscopic:
- Granulomas

How can we investigate a patient if we suspect them to have Crohn’s disease?
- Bloods for anaemia
- CT/MRIs to check extramural problems
- Barium enema or follow through only if no strictures or fistulas
- Colonoscopy/endoscopy to see gross changes
- Biopsy for granulomas

What would be a typical presentation of ulcerative colitis?
- Multiple blood stools a day
- Mild abdominal pain/cramping
- 20-30 yeards old
- Weight loss
- Normal temperature
- No perianal disease

What would you see histologically when looking at a biopsy of a bowel with ulcerative colitis?
- Chronic inflammatory filtrate of lamina propria
- Crypy abscesses (neutrophils)
- Crypt distortion
- Reduced number of goblet cells

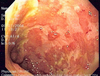
What would you see macroscopically on a colonoscopy with ulcerative colitis?
- Pseudopolyps that are non neoplastic due to inflammation then healing
- Loss of haustra due to inflammation (can be seen on contrast x ray)

How would you investigate a patient if you suspected that they had ulcerative colitis?
- Bloods for anaemia
- Stool cultures for blood
- Colonoscopy (usually when not bad episode to minimise bleeding - continuous)
- Barium enerma
- CT/MRI (less used)
Sometimes after testing it is hard to determine the difference between UC and Crohn’s, what will the diagnosis be?
Has features of both

Fill in the following tables to confer the difference between UC and Crohn’s?


What sign might you seen on a barium follow through of Crohn’s?
String sign of kantour (long strictures)

What sign might you see on a double contrast (barium and air) enema with UC?
- Lead pipe colon (lack of haustra)
- Continous lesions without skipping
- Really active UC will see granular appearance due to mucosal inflammation





