13 - Hepatology Flashcards
What are the functions of the liver?

What are some causes of unconjugated hyperbillirubinaemia and conjugated hyperbilirubinaemia?
Unconjugated:
- Haemolytic disorders (e.g malaria)
- Drugs affecting liver (e.g paracetamol)
- Impaired conjugation (e.g Gilbert’s)
Conjugated
- Hepatocellular dysfunction (e.g viruses like hepatitis and CMV, liver metastases, a1-antitrypsin)
- Cholestasis (e.g primary sclerosing cholangitis, CBD gallstones, Mirizzi syndrome)

What are some drugs that cause drug induced jaundice?

If a patient is jaundiced what investigations should you order?
- Liver screen (inc albumin and total protein)
- Paracetamol level
- Urine to check for billirubin in post-hepatic jaundice
- FBC, clotting, reticulocytes, malaria film, parasites, Coombs
- Blood cultures
- Hepatitis serology
- US of bile ducts
- Liver biopsy

What is the definition of liver failure and what are some causes of this?
Development of coagulopathy (INR>1.5) and encephalopathy
If occurs in previously healthy liver it is acute liver failure, however more often occurs on top of cirrhosis so chronic liver failure
Causes: infections, drugs, toxins, vascular, alcohol, autoimmune conditions

It is important to distinguish whether liver disease in a patient is acute or chronic. What questions should you ask the patient in the history to work this out?
- Any blood transfusions?
- Any IV drug use?
- Operations with dubious sterile procedures?
- Sexual exposure?
- Medications taken (prescribed/OTC)?
- FHx of liver disease, diabetes and IBD?
- Alcohol?
- Foreign travel?
- Obesity?

What are some causes of acute liver failure?
- Drugs (e.g Paracetamol OD, halothane)
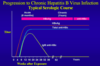
- Viral Hepatitis
- Amanita Phalloides mushroom
- Wilson’s disease
- Fatty liver of pregnancy
- Malignancy

What are some signs of acute liver failure?

Acute: jaundice, hepatic encephalopathy, fetor hepaticus (sweet musty breath), asterix/flap, constructional apraxia
Chronicity: spider naevi, clubbing, ascites, palmar erythema

What is hepatic encephalopathy and how is the severity of it graded?
Decline in brain function as a result of severe liver disease due to a build up of toxins in the blood stream

What are some blood investigations you should do in suspected acute liver failure?
IMPORTANT
- FBC: often thrombocytopenia if liver fibrosis
- LFTs: ALT raised if hepatocytes damaged, ALP and gamma-GT raised if ducts damaged, albumin may be decreased
- Clotting: INR often increased
- Paracetamol Level
- TFTs, Lipids and Glucose
- Rest of liver screen: see image

What other investigations should you order for a patient with acute liver failure after bloods?
- Blood and urine cultures
- Abdominal US of liver and pancreas
- CXR
- Doppler US of hepatic vein if Budd-Chiari suspected
What is included in an LFT panel?
Hepatocellular damage/Cholestasis:
- ALT
- ALP
- AST
- Gamma GT
Synthetic Function of Liver:
- Billirubin
- Albumin
- PT/INR
What are some causes of an isolated ALP increase (no gamma GT increase)?
- Metastases or primary bone tumours
- Vitamin D deficiency
- Recent bone fractures
- Renal osteodystrophy
What are some causes of an isolated rise of billirubin (no derangement of ALT/ALP)?
- Haemolysis
- Gilbert Syndrome
What are some causes of the following:
ALT>AST
AST>ALT
- Chronic liver disease
- Cirrhosis and Acute alcoholic hepatitis

If an LFT panel shows a cholestatic abnormality, what test is carried out next?
Need to do an US to look for any obstructive jaundice, which would have dilatation of the bile ducts
What are some causes of hepatic and cholestatic derangement of LFTs?
Hepatic: ALT raised mostly
Cholestatic: ALP and gamma GT raised markedly and ALT/AST slightly raised

What might you find on abdominal US with cirrhosis?
- Nodularity
- Coarse texture
- Splenomegaly
- Ascites
What is the immediate management of acute liver failure?
- Refer to critical care and nearest liver transplant unit as may need transplant
- Place urinary and central venous catheter to measure urine output hourly
- Treat the cause if known (e.g paracetamol poisoning) and complications
- 10% glucose IV 1L/12h to reduce risk of hypoglycaemia, check BM every 1-4h
- Avoid sedatives
- Haemodialysis if renal failure develops
- Provide nutritional support

What are some of the complications of acute liver failure and how are they managed?
- Cerebral oedema
- GI Bleeding/Varices
- Encephalopathy
- Hypogylcaemia
- Sepsis
- Renal failure

What is the criteria for predicting poor outcome with paracetamol induced acute liver failure?
King’s College Criteria
If fulfill these criteria should promptly consider transplant!!!!
(pH<7.3, signs of encephalopathy, INR 3, plasma creatinine >200)

What are some of the signs and symptoms of paracetamol overdose? (>12g/24 tablets)
- Initially nothing
- Nausea/vomiting
- RUQ pain
- Jaundice
- Encephalopathy
- AKI

What are some investgiations you should do for a patient coming in with paracetamol OD?
- Patient’s weight for treatment
- Paracetamol levels after 4h of ingestion and compare with treatment graph
- FBC and INR
- LFTs, U+Es, Phosphate
- VBG for pH, lactate, glucose, bicarbonate

How is a paracetamol overdose managed initially?
<4hours since OD: activated charcoal
4 hours: take glucose, U+Es, LFT, INR, ABG, FBC, HCO3, paracetamol level
<10-12h after OD and paracetamol level over treatment line: 3 consecutive acetylcysteine IV infusions over 20 hours, checking paracetamol levels at end of 2nd infusion
>8-24h after OD and suspect large OD: acetylcysteine