10b.) CKD Flashcards
Describe adult polycystic kidney disease, include:
- Abnormal cysts (swellings filled with fluid) form on kidneys and other organs
- Autosomal dominant
- Mutation in:
- PKD 1 gene (85%)
- PKD 2 gene
- Diagnosed via ultrasound (but may do genetic testing if family history)
- Prognosis depends on rate of increase in kidney size and age- eventually leads to kidney failure
- Symptoms:
- Pain in kidneys
- Haematuria if cyst bursts
- High blood pressure
- Infection
- Renal stones
- Any other symptoms of kidney failure

Explain why adult polycycstic kidney disease generally presents in adulthood
- Cysts grow with age and we diagnose on ultrasound so cysts might not be visible till adulthood (this is why you can’t exclude APCKD with ultrasound if patient under 30 years old)
- Takes time for renal failure to develop
For adult polycystic kidney disease, the mutation can be in PKD 1 gene or PKD 2 gene; which mutation causes earlier disease?
PKD 1 gene (it is also more common ~85%)
What happens to the size of kidneys in adult polycytic kidney disease?
Increase

Hypertension is often the first sign of adult polycystic kidney disease and it occurs before renal function changes; true or false?
True
Patients with adult polycystic kidney disease have an increased incidence of what 2 conditions?
- Intra-cranial aneurysm
- Heart valve abnormalities
Describe the managemetn of adult polycystic kidney disease, including pharmacological and general management
- Treat hypertension: block RAAS e.g. ACE inhibitor, angiotensin blocker
- Diet:
- Lots of fluid (4L)
- Low salt
- Normal but not excessive protein
- Tolvaptan: vasopressin II antagonist hence causes increased urination (a lot therefore can have low compliance)
- Others e.g. somatostain analogues
Describe how GFR and hence the general aims of treatment changes as you progress through stages of chronic kidney disease

How many nephrons do humans have in total?
How many do we need to survive?
- 2 x106 nephrons (1 x106 in each kidney)
- Only need 40,000 to survive
IDEA IS JUST TO SHOW SCALE OF DAMAGE NEEDED TO CAUSE RENAL FAILURE
Define chronic kidney disease
Progressive and irreversible loss of renal function over a period of months to years
Describe what happens to renal tissue in CKD
Damaged renal tissue is replace by extracellular matrix (fibrosis) histologically giving rise to glomerulosclerosis and tubuler interstitial fibrosis
CKD is associated with substantial cardiovascular morbidity and mortality even with mild CKD; true or false?
True
Describe how we stage CKD
We look at GFR in combination with albuminuria

State 4 categories of people that CKD is more common in
- Elderly
- Ethnic minorities
- Multi-morbid
- Social deprivation
What % of population in UK have CKD?
6.1%
State some common causes of CKD
- Diabetes (MOST COMMON)
- Arteriopathic kidney disease
- Hypertension
- Immunological e.g. glomerulonephritis
- Infection e.g. pyelonephritis
- Other systemic diseases e.g. lupus
- Obstructive and reflux nephropathies
- Genetics (family history of CKD stage 5 or adult polycystic kidney disease)
If a child presents with polycystic kidney disease what is the inheritance pattern likely to be?
Autosomal recessive
Describe what happens to size of kidney in CKD
Kidney size decreases (renal cortex size decreases)

Histology shows fibrosis
What are the two most common causes of CKD?
- Diabetes (45%)
- Hypertension (33%)
State some factors, other than the underlying disease process, that may cause progressive renal injury (3)
- Any form of AKI (including nephrotoxins or decreased perfusion)
- Proteinuria
- Hyperlipidaemia
State some symptoms of CKD
- Tirendess
- Breathlessness
- Restless legs
- Sleep reversal
- Aches & pains
- Nausea & vomitting
- Ithcing
- Chest pain
- Seizures
CKD is a systemic disease; state effects on:
- General effects
- Cardiovascular
- Haematology
- Bone
- CNS
- GI
- Endocrine
- Metabolic

What happens to the:
- Life expectancy
- Quality of life
… of patients with CKD?
Both decrease
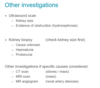
When investigating CKD what 5 things must we do?
- Define degree of renal impairment
- Defince cause of reanl impairment
- Provide patient with diagnosis & prognosis
- Identify complications of CKD
- Plan long term treatment (delay progression & plan for for dialysis and transplantation)