Week 2 - D - Myeloma, MGUS, AL AMyloidosis, Waldenstroms - B/Plasma cells/Ig - electropheresis/immunofixation, Signs&Tx Flashcards
Bcells are derived in the bone marrow from haemopoietic stem cells Which immune system are they part of? What is the dual function of the Bcells?
They are part of the adaptive immune system B cells have the dual function of producing antibodies and acting as an antigen presenting cell
Antibodies are produced by B cells and plasma What is the difference in antibody produced by both these cells?
When B cells produce antibodies, they stick to the surface of the B cell Plasma cells actively secrete antibodies
The term antibodies and immunoglobulins are interchangeable - usually when speaking of the functional aspect we use the term antibodies and when speaking of the structural aspect we use the term immunoglobulin What are the chains from which immunoglobulins are made?
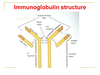
Immunoglobulins are made from 2 heavy chains and 2 light chains
Does the type of immunoglobulin produced depend on the light chain or heavy chains? What are the different heavy chains?
The type of immunoglobulin produced by the B cell depends on the type of heavy chain that is used There are five different heavy chains (α, δ, ε, γ, μ) Alpha (IgA), Delta (IgD), Epsilon (IgE), Gamma (IgG), Mu (IgM)
IN B cells –antibody is stuck to the surface of the B cell IN plasma cells – the cell is actually secreting the antibody into the blood steam Proteins made up of 2heavy and 2 light chains The type of antibody depends on the type of heavy chains used (5types) The 2 light chains are kappa or lambda chains (κ or λ) What forms the backbone of the immunoglobulin and what are the bonds that join them?
The backbone of the immunoglobulin is formed by the heavy chains The two heavy chains are joined by disulphide bonds
Each antibody recognises a specific antigen The basic functional unit of each antibody is an immunoglobulin (Ig) monomer (containing only one Ig unit) WHat are the different stuctures of each immunoglobulin?
IgD, IgE, IgG are all monomers IgA is a dimer IgM is a pentamer
https://s3.amazonaws.com/classconnection/403/flashcards/11907403/png/paella-recipedocxpngjpg-162217023AA3D155A85.png

- Question 1 - IgA
- Question 2 - IgD
- Question 3 - IgE
- Question 4 - IgG
- Question 5 - IgM
IgG is the most abundant antibody type IgM is the first antibody in response to infection (M for iMMediate)
Name what the different boxes are referring to What is the bond that the black box is pointing to? What regions are represented by the purple and blue areas of the chains?

- The green box is the antigen binding site
- The blue box is the light chain
- The black box is pointing to the disulphide bones that connect both heavy and light chains
- The heavy chain is the backbone of the immunoglobulin
- The yellow box refers to the Fc fragment
- The red box refers to Fab fragement of the immunoglobulin
Purple = variable regions Blue = constant regions
Antigens bind at the antigen binding site of the immunoglobulin Where do the Fc fragments bind?
The Fc fragments bind to Fc receptors which is a protein found on certain cells that antibodies can then join onto and await for antigens to bind to the binding sites

B cell Initial production and development is in the bone marrow under control/influence of microenvironment What is the Ig variable element determined by?
The Ig variable element is determined by the V-D-J region recombination early in development of the cell
After the VDJ region recombination, the Ig variable element is determined - thousands of combinations can be produced form this VDJ region recombination Immature B cells with (Ig) on their surface exit bone marrow ready to meet their target. Where do B cells mature?

The B cells mature in the lymph nodes
The process of generating antibodies with increased binding affinities is called affinity maturation. Affinity maturation occurs in mature B cells after V(D)J recombination, and is dependent on help from helper T cells Where do the B cells travel in the lymph node to mature?
The B cells travel to the follicle germinal centre to mature The B cells are exposed to antigens - the ones that bind antigens well will survive, the ones that don’t bind as well will undergo aspoptosis
Once the B cell is matured in the lymphoid follicle germinal centre, it may return to the bone marrow as what two cells?
The B cell may return to the bone marrow as a plasma cell or a memory B cell

Plasma cells pump out antibodies What is the appearance of the plasma cell on blood film described as? What does the plentiful blue cytoplasm of the plasma cell contain? What is the open chromatin synthesising? On blood film, there may be a slight perinuclear pale area (perinuclear halo) - what is this?
The appearance of the plasma cell on blood film is described as a fried egg appearance Open chromatin is synthesising mRNA to help make proteins which are found in the plentiful blue cytoplasm There is also a perinuclear halo which is where the golgi apparatus lies

Plasma cells are large lymphocytes with a considerable nucleus-to-cytoplasm ratio and a characteristic appearance on light microscopy. What is the normal number of plasma cells to find on a bone marrow aspirate?
Usually only about 2% of the bone marrow is found to have plasma cells but in conditions affecting the plasma cells, can see more than this 2%
Because plasma cell malignancies arise from one cell, they are monoclonal It is monoclonal therefore giving the same one abnormal immunoglobulin When is there a polyclonal increase in immunoglobulins?
There can be a polyclonal increase in response to reactive things such as: * Infection * Autoimmune * Malignancy * Liver disease
What is a monoclonal rise in immunoglobulins due to? Are the antiboides produced identical or not?
A monoclonal rise in immunoglobulins is due to clonal expansion of a single B-cell The antibodies are identical in structure and specificity (size and charge)
Presence of a monoclonal immunoglobulin implies there is a clone of faulty B cells or plasma cells somewhere What is the name given to a monoclonal immunoglobulin?
The name given to a monoclonal immunoglobulin is a paraprotein
Again, what is the marker of underlying clonal B-cell disorder?
This would be a monoclonal rise in immunoglobulins is a marker of an underlying clonal B-cell disorder
If a patient presents ie with back pain that is not improving and systemic cancer symptoms WHat test can be carried out to measure for monoclonal protein bands?
Look for monoclonal protein bands in serum or in urine by using electropheresis
The electropheresis separates the proteins in the serum into distinct bands(or zones) WHich protein lies nearest the positive charge of the electropheresis and why?
Albumin is very negatively charged and therefore lies nearest to positive charge on electrophereisis Gamma proteins are positively charged and therefore move furthest away form the positive charge on electropheresis
It is in the gamma proteins in the blood where the immunoglobulins are found On electrophereisis, what is it that affects the rate at which proteins move?
Proteins move at different rates dependent on their size and charge

On electropheresis the gamma band should be very fuzzy as there should be polyclonality and not a monoclonal immunoglobulin rise which would cause what?
A monoclonal rise in immunoglobulins would cause a distinct zone in the gamma band and this would warrant further investigation

If an abnormal protein band is identified on serum or urine electropheresis, what is carried out to identify what type of paraprotein (monoclonal immunoglobulin) is present?
Serum immunofixation would be carried out - this enables the paraprotein present to be identified















