Week 1 Flashcards
(114 cards)
What are some common problems in insulin treatment?
Giving an incorrect dose
Omitting insulin (forgetting, if ill etc.)
Giving the wrong type of insulin
Which structure in the neck is the first complete cartilagenous ring (if travelling superiorly to inferiorly)?
The cricoid cartilage
The thyroid cartilage isn’t a complete ring!
How many ATP are produced per glucose molecule?`
36
The carotid sheaths blend inferiorly with which structure?
At what level does the common carotid bifurcate, and which branch remains within the carotid sheath?
Blends with the mediastinal fascia
Bifurcates at the level of C4, and the internal carotid artery remains within the carotid sheath
Very generally, how do Type I and Type II Diabetes Mellitus differ?
Type I - loss of most of the beta cells responsible for secreting insulin, resuling in high levels of blood Glucose
Type II - beta cells lose the ability to sense changes in blood Glucose due to hyperglycaemia taking Glucose concentrations outwith the Km of Glucokinase, the beta cells have “been worked very hard and are likely to be very stressed”
Can hormones bound to a carrier molecule cross capillary walls and activate receptors?
No - only ‘free’ (i.e. unbound) hormones can cross the capillary wall
Glucagon (lowers/raises) blood glucose.
How does it do this?
What other hormone is involved?
Glucagon raises blood glucose
It does this by stimulating hepatic glycogenolysis and gluconeogenesis
Unlike insulin, it does not affect the uptake of glucose into muscle and adipose tissue. However, adrenaline does inhibit this, resulting in an increased plasma glucose
How is control of Diabetes measured?
Home blood glucose monitoring - used in day-to-day diabetes management and allows for adjustments in insulin dose, but only provides a snapshot at one particular time point. Continuous glucose monitoring provides the whole picture
Urinalysis to measure ketones and glucose
HbA1c measurements
What are some of the functions that carrier proteins provide?
Allow for a reserve of hormones
Increase the amount of hormones transported in the blood
Extend the half-life of the hormone in circulation
Describe the synthesis and structure of insulin
Synthesised in the Rough ER of pancreatic Beta cells as a larger single chain prehormone - Preproinsulin
Preproinsulin is then cleaved to form Insulin
Insulin contains 2 polypeptide chains linked by disulphide bonds
What is the early clinical effect on vision of a pituitary gland tumour?
A pituitary tumour will initially result in midline compression of the optic chiasm
This results in disruption of the action potentials from the nasal retinas, meaning the patient loses the ability to see structures in the temporal side of the visual field, bilaterally
This is known as bilateral hemianopia

Insulin (lowers/raises) blood glucose.
How does it do this?
Insulin lowers blood glucose by inhibiting hepatic glycogenolysis and gluconeogenesis
It also stimulates uptake of glucose into muscle and adipose tissue
In embryological development, at what time does the thyroid gland reach its final position in relation to the larynx/trachea?
7th week of development
How does T1DM classically present?
Is there typically evidence of microvascular disease at the time of diagnosis?
Pre-school and peri-puberty, with a small secondary peak in late 30s
Usually lean
Acute onset and severe weight loss, thirst, polyuria
Weakness, fatigue, lethargy, blurred vision. Possibly presenting with thrush
Ketonuria +/- metabolic acidosis
Typically no signs of microvascular disease at the time of diagnosis
Name to surgical approaches to accessing the pituitary fossa
Transcranial - under the frontal lobe
Transsphenoidal - via the nasal cavities and sphenoid sinus
What is the name of the structure that connects the Hypothalamus to the Pituitary gland?
The infundibulum

What are the blood glucose targets in insulin treatment pre- and post meal?
3.9-7.2 mmol/L pre-meal
<10 mmol/L 1-2 hours following a meal
Insulin is a hormone of the ____ state.
What happens to Insulin upon feeding? What is it’s action?
FED state
Insuline is RELEASED from pancreatic beta cells in response to feeding. This results in a LOWERING of blood Glucose
To what group do the platysma muscles belong to? What is their nerve innervation?
The muscles of facial expression
The facial nerve (CNVII)
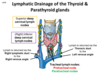
What structures lie near the Thyroid gland?
Describe the order of contents in the Carotid Sheath
Thyroid gland is covered in pretracheal fascia
Trachea (anterior) and Oesophagus (posterior) lie in the centre line. In between these are the Recurrent Laryngeal Nerves
Either side of the Thyroid gland, outside the pretracheal fascia, are the carotid sheaths, and laterally to medially these go Internal Jugular Vein, Vagus Nerve, Carotid Artery

What common embryological variations are seen in the thyroid?
Pyramidal lobe - 28-55% prevalence, most commonly originating from the left lateral lobe
Incomplete/missing isthmus
What structures are found within the carotid sheath?
Vagus nerves
Carotid arteries - common then internal
Internal jugular vein
Deep cervical lymph nodes
In the transsphenoidal transnasal surgical approach to the pituitary, which sinuses of which bone need to be passed through?
This approach requires the surgical fracture of the nasal septum, as well as the floor and roof of the sphenoid sinuses, which are located in the sphenoid bone
Describe the secretion of Insulin
Glucose enters Beta cells through the GLUT2 glucose transporter and is phosphorylated by glucokinase
This increased metabolism of Glucose results in an increase in intracellular ATP, which inhibits the ATP-sensitive K+ channel, KATP
Inhibition of KATP = depolarisation of cell membrane = opening of voltage-gated Ca2+ channels
Opening of Ca2+ = fusion of secreteory vesicles with cell membrane = RELEASE OF INSULIN