Week 1/2 - B - Histology 1/2 - G.I Wall Layers, Epithelium of tract, Enteric nervous system, sphincters, tongue, liver, G.B, pancreas Flashcards
The alimentrary canal is a series of hollow organs running from mouth to anus (oral to aboral) that are separated by sphincters, controlling movement What are the four major functions of the alimentary canal?
Motility - movement - mechanical activity Secretion - for digestion, protection and lubrication Digestion - chemical breakdown of foods Absorption - transfer of the absorbable products made by the breakdown of foods
Which type of muscle in the GI tract is the motility mostly due to? Where does the other type of muscle (obviously not cardiac) become involved in the GI tract?
GI tract motility is mainly due to the activity of smooth (involuntary) muscle Skeletal muscle is important in the mouth, pharynx, upper oeseophagus and external anal sphincter
The generalised structure of the digestive tract wall is made from four named layers - each layer is made up of different components What are the layers of the GI tract wall?
Inner layer to outer layer - mucosa submucosdia muscularis externa serosa
Which layer of the gI tract wall is the musclcular layer found? What are the two different muscles?
Muscular layer of GI tract is the muscularis externa Circularis muscle layer and longituindal muscle layer is found in the muscularis externa layer

What controls the circular and longitudinal muscle functions? - it is also found in the muscularis externa What are the different functions of the circular and longitudinal muscle contractions?
Myenteric (Auberach’s) plexus controls the muscle functions Circular muscle - lumen becomes narrower and longer - usually happens behind the food bolus Longitudinal muscle - intestine becomes shorter and fatter - usually happens in front of the food bolus

Autonomic inneration of the GI tract Where do the preganglionic parasympathetic fibres synapse and what do they release? What are the excitatory and inhibitory influences of the parasympathetic innervation on the GI tract?
Preganglionic fibres (releasing acetylcholine) synapse within ganglion cells essentially on the walls of organs within the enteric nervous system Excitatory influences - increases secretions, blood flow and smooth muscle contraction Inhibitory influences - relaxation of sphincters

Where do the preganglionic and postganglinic sympathetic fibres synapse and what do they release? What are their excitatory and inhibitory influences?
Preganglionic fibres (releasing ACh) synapse in the prevertebral ganglion (except for adrenal) - the postganglionic fibres (releasing ) innervate mainly the enteric nervous system Excitatory influences - increased sphincter tones Inhibitory influences - decreased secretions blood flow and motility,
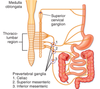
The enteric nervous system is embedded in the lining of the gastrointestinal system, beginning in the esophagus and extending down to the anus. The neurons of the ENS are collected into two types of ganglia: * What are these ganglia known as and what layers of the GI tract wall are they found in?
Submucous plexus (Meissner’s plexus) found in the submucosal layer of the GI tract wall Myenteric plexus (Auerbach’s plexus) found in the muscularis externa layer of the GI tract wall

What is the function of both the submucous plexus and myenteric plexus?
Submucous (Meissner’s) plexus - mainly modulates epithelia and blood vessels (also controls the muscularis mucosae of the mucosal layer) Myenteric (Auerbach’s) plexus - mainly regulates motility (circular/longitudinal muscle) and sphincters
What controls the enteric nervous system?
The enteric nervous system is intrinsic to the GI tissue and reflex circuits can operate independently however hormones and extrinsic nerves exert a strong regulatory influence
What are the 6 sphincters of the alimentary canal (excluding the sphincter of Oddi) ? State whether they are smooth muscle or skeletal muscle They act essentially as one way valves by maintaining a positive resting pressure relative to two adjacent structures (e.g. oesophagus and stomach)
Upper oesophageal sphincter aka cricopharyngeus - skeletal Lower oeseophageal sphincter - smooth Pyloric sphincter - smooth Ileocaecal valve - smooth Internal anal sphincter - smooth External anal sphincter - skeletal

State the function of each of the sphincters of the GI tract (why do they open and why do they close)
Upper oeseophegeal sphincter - relaxes to allow swallowing, closes during inspiration Lower oeseophageal sphincter - relaxes to allow entry of food to stomach, closes to prevent reflux of gastric contents to oeseophagus Pyloric sphincter - regulates gastric emptying, usually prevents duodenal gastric reflux Ileocaecal valve - regulates flow from ileum to caecum, distension of ileum opens it, distension of proximal colon closes it Internal and external anal sphincters - opens to allow defecation, closes to prevent defecation
What type of epithelium lines the oral cavity, oropharynx and laryngopharynx? What type of epithelium lines the nasal cavity and nasopharynx?
Oral cavity, ororopharynx and laryngopharynx are lined by stratified squamous epithelium that is generally not keratinized Nasal cavity and the nasopharynx is lined by respiratory epithelium - ciliated pseudostratified columnar epithelium with goblet cells
What type of epithelium lines the tongue?
The tongue is lined by keratinised stratified squamous epitherlium but is referred to as specialized mucosa because of the presence of lingual papillae
The lingual papillae are the structures on the upper surface of the tongue that give it its characteristic rough texture The four types of lingual papillae have different structures * What are they classified as? * Which has no taste buds? * Which is the most abundant papillae?
Fungiform papillae Circumvallate papillae Foliate papillae Filiform pappillae - has no tastebuds but is the most abundant papillae of the tongue

The pharynx (orophaynx) contains a ring of lymphoid tissue What makes up this ring of lymhpoid tissue and what is it known as?
Waldeyer’s ring consists of four tonsillar structures; namely, * Palatine tonsils x2 * Tubal tonsils x2 * Lingual tonsils * Pharyngeal tonsils (adenoids) as well as small collections of lymphatic tissue disbursed throughout the mucosal lining of the pharynx (mucosa-associated lymphoid tissue, MALT).

From the oesophagus to the anal canal the architecture of the digestive tract is composed of 4 major layers (starting from the lumen and going out): State again what the 4 layers are and what is in them?
Mucosa - epithelium, lamina propria, muscularis mucosae Submucosa - loose connective tissue and submucous (Meissner’s) plexus Muscularis externa - inner circular layer and outer longitudinal layer of muscle, myenteric (Auerbach’s) plexus Serosa or adventitia - outer layer of connective tissue

What is the transition in epithelium from oeseophagus to the epithelium of the cardia of the stomach?
There is an abrupt transition from stratified squamous epithelium of the oesophagus to the simple columnar epithelium of the stomach

What are the most numerous cells of the small intestine? - they are also the principle absorptive cell of the small intestine
These are the enterocytes
There is a substantial amount of lymphoid tissue associated with the gut (hence ‘gut associated lymphoid tissue’ or ‘GALT’). Much of this consists of scattered lymphocytes, but areas of relatively large aggregations of lymphoid tissue exist, particularly in the ileum. What are these relatively large areas of GALT in the ileum known as?
These are known as Peyer’s patches

What is the change in mucosa from rectum to anal canal to surrounding skin of anus?
Rectum - simple columnar epithelium Anal canal - non-keratinized stratified squamous epithelium The 2-3cm long anal canal is then continuous with the keratinized stratified squamous epithelium of the surrounding skin.

The digestive tract has its own nervous system called the enteric nervous system, which has about the same number of neurons as the spinal cord! The ENS receives input from the autonomic nervous system, but is capable of coordinating gut motility locally. This interconnected network of fibres has two plexuses, one in the submucosa (submucosal) and one between the muscle layers of the muscularis externa (myenteric). * What is the function of both of these plexueses?
Submucosal plexus (Meissner’s) - mainly modules epithelium (eg epithelial secretions) and blood vessels (also controls the muscle of muscularis mucosae) Myenteric plexus (Auerbach’s) - regulates gut motility and sphincters
The liver has classically been viewed as made up of segments called lobules. What is the vein known as that drains each lobule? What drains into this vein? What is found in each corner of the liver lobule?
Each lobule is approximately hexagonal in shape and hepatic sinusoids drain into a branch of the hepatic vein called the centrolobular vein (or central vein) There are portal triads at each corner of the liver lobule - branch of hepatic artery, hepatic portal vein and bile duct

What are the main cells of the liver known as? What are the simple cuboidal cells that line the bile ducts known as?
The main cells of the liver are the hepatocytes. The simple cuboidal cells that line the bile ducts are also known as cholangiocytes
Bile is an alkaline solution containing water, ions, phospholipids, bilirubin and bile salts What gives faeces its brown colour from the bile? Where is this produced? What are bile salts necessary for? What cells produce bile?
The bilirubin is a pigment which results from the breakdown of hemoglobin in the spleen, and when excreted in the bile, is the principal cause of the brown colour of feces. The bile salts are necessary for the emulsification of fats in the digestive tract. Bile is produced by the hepatocytes

What is the function of the gallbladder? What stimulates the gallbladder to contract?
The function of the gallbladder is to store and oncentrate the bile The gall bladder is stimulated to contract both under nervous control (chiefly vagal) and via the release of cholecystokinin (chole - bile, cysto -gall bladder, kinin - move) by the endocrine cells of the duodenum when fatty food enters it
The pancreas is unusual in that it is both an exocrine and an endocrine gland. What is produced by the exocrine pancreas?
The exocrine pancreas produces digestive juices containing proteases to break down proteins, lipases to break down lipids, nucleases to break down DNA/RNA, amylase to break down starch etc

The pancreas produces both active enzymes such as pancreatic amylase and pancreatic lipase as well as inactive forms known as proenzymes What converts the proeznymes to enzymes and where is this secreted from?
Once the pancreatic secretion arrives in the duodenum an enteropeptidase (aka enterokinase) converts the inactive proteolytic enzyme trypsinogen into the active form, trypsin. This begins a cascade that results in the activation of the other enzymes.

What is produced by the endocrine pancreas?
The endocrine pancreas consists of small, scattered islands of tissue called islets of Langerhans, which produce a number of hormones including insulin and glucagon.

What does the main pancreatic duct join with? What does it form and where does it open into?
The main pancreatic duct joins with the common bile duct (common hepatic duct + bile duct) to form the hepatopancreatic ampulla (ampulla of Vater) This empties into the 2nd part of the duodenum via the major duodenal papilla



