Ventilation/Perfusion Flashcards
(44 cards)
total exhaled ventilation
Ve

- Total amount of ventilation in and out of lung at any moment, or averaged over time. Called Total Exhaled Ventilation.
- Why exhaled? Don’t want to confuse with TV (total or tidal volume). Also, in the laboratory most measurements are taken with respect to exhaled
- Ve can be broken into two components:
Dead space ventilation
- Dead Space Ventilation (Vd): ventilation stuck in airway and cannot participate in gas exchange, which only occurs in the alveolus.
- Its functionally dead in terms of gas exchange but that portion of the lung is alive and well.
Alveolar ventilation
•Alveolar Ventilation (Va): Component that makes it down into the alveolar air space. It is the component that’s responsible for the uptake of O2 into the blood and the excretion of CO2.
Relationship between 3 types of ventilation
Va = Ve - Vd

What does total ventilation reflect?
work performed by respiratiory system
•The total ventilation reflects the work that your respiratory system is performing. Very clinically relevant; SOB (dyspnea) is considered to be an elevated or increased work of breathing until it becomes uncomfortable. Work load has to reflect total ventilation.
Brain can only control output the muscle which controls total ventilation. Cannot control only alveolar ventilation
what does dead space ventilation reflect?
vol of ventilation that does not participate in gas exchange
25% of TV in normal subjects - increased by disease
•Dead space does not participate in gas exchange and accounts for approximately 25% of the tidal volume for those of us sitting in the room. A normal tidal volume might range from 500-600, the dead space volume is around about 125-150 ccs and so if you divide those 2 numbers you will come up with about 25% of the tidal volume. That 25% is an insufficiently in the system. It becomes increased in a variety of pulmonary diseases; thus we want to measure as an indication of how much insufficiency a patient has.
what does alveolar ventilation reflect?
volume of ventilation that participates in gas exchange! most important for determinng arterial PCO2
•Alveolar ventilation participates in gas exchange. It is very important in determining the arterial partial pressure for CO2.
measurement of dead space ventilation
inspiration - no CO in dead space (at end of inspiration!)
in expiration - volume exhaled is diluted by volume of dead space -
- At end of inspiration there is no Co2 in dead space volume because there is no gas exchange. To measure dead space we allow subject to exhale and collect exhaled gas in chamber. Shown in end of expiration diagram on right.
- Lung volume is now smaller, dead space volume now has Co2 in dead space because when first aliquot of air came out of lung that is air already in the airways (no Co2). As patient continues to exhale you have alveolar gas entering through airways such at there is a partial pressure of Co2 in the airways that is present and measurable.
- Fraction of Co2 in airway should be the same as fraction in alveoli. Looking at exhaled chamber (in box), there will be a lower fraction of Co2 because it includes dead space volume (that has no Co2) mixed with alveolar volume (which has Co2) resulting in a lower Co2 fraction than that which was present in alveolar gas.
- Thus, the concentration of Co2 in exhaled gas reflects how much alveolar gas is diluted by the dead space.
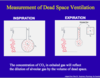
equation for measurement of dead space
VD/VT = (PaCO2 -PeCO2)/PaCO2

measurement of alveolar ventilation
measure dead space ventilation (using exhaled PCO2) and then subtract from total ventilation
equation for the arterial pressure of CO2
metabolic CO2 production/alveolar ventilation

•How do we measure total volume of Co2 being produced all over body?
•At STEADY STATE, it has to reflect the volume made at tissues. Thus, metabolic Co2 production equals volume of exhaled Co2 at steady state.
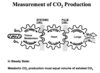
how do we measure CO2 production?
volume of exhaled CO2 = total exhaled ventilation x PP CO2 in air
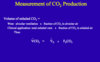
alveolar ventilation equation
PaCO2 = K x VCO2/VA
VCO2 can be estimated by body size and metabolic state
In a healthy subject, what would 50% increase in metabolic rate do to arterial PCO2?
nothing! body compensates
hyperventilation
reduced arterial CO2
must occur due to an increase in VE since VD can’t change
- Low pCo2 is alveolar hyperventilation. Only way occurs is if alveolar ventilation goes up and only way to do that is to increase total ventilation because can’t selectively reduce dead space.
- Low pCo2 is probably most common blood gas abnormality you will encounter in clinical medicine. If you take people with resp. disease most common finding is low pCo2. Reason is not known but probably due to a variety of factors including probably a variety of receptors in lung parenchyma that feedback to resp. control system via vagus nerve and result in increase in ventilation. Normal response to a disease, and if a patient chooses to breathe at an elevated ventilatory rate, so be it. But nothing of interest in terms of an abnormality in the system.

hypoventilation
elevated arterial CO2
may occur due to decreased VE or increased VD
- More interesting phenomenon is when pCo2 goes up because that tells you that there is failure of the respiratory system to excrete Co2 and that is a type of resp. failure that you’ll learn next week. Does pCo2 go up because reduction in ventilation or increase in dead space?
- Lung disease reduces ventilation and increases dead space. Neuromuscular diseases generally result in reduced ventilation. Sleep also reduces ventilation, but metabolic rate also goes down. But the drop in ventilation is larger than drop in metabolic rate. pCo2 goes up 4, 5 or 6 mmHg in normal adults during sleep.
- Increase in dead space is generally attributed to disease states.

neuromuscular disease
drop in ventilation because can’t do effort
lung disease
drop in ventilation
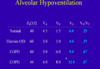
hypoventilation - heroin overdose
elevated CO2
decrease in VE - proportional decrease in VD and VA
ratio of dead space stays the same!

hypoventilation - COPD at rest
CO2 is increased
VE is high - so is VD and VA
VD is disproportionally high - much bigger ration, need more VE to get to get VA

hypoventilation - COPD on big breath
hugh increase in VE
HUGE VD
can raise VA and lower PCO2 enough but still have really high percent of dead space
how to assess level of ventilation
look at pCO2
how to assess oxygenation
measure PO2, pH
calculate O2 sat