UWORLDS Flashcards
where are these seen? are they all from the same disease?

NERP!
ALZHEIMERS.
A= Senile plaques in gray matter: extracellular
β-amyloid core; may cause amyloid angiopathy intracranial hemorrhage; Αβ (amyloid-β) synthesized by cleaving amyloid precursor protein (APP).
ALZHEIMERS STILL
B= Neuro brillary tangles: intracellular, hyperphosphorylated tau protein = insoluble cytoskeletal elements; number of tangles correlates with degree of dementia.
Frontotemporal dementia
C=Inclusions of hyperphosphorylated tau (round
Pick bodies; (can also see ubiquitinated TDP-43)
this Congenital heart defect is:
*Caused by anterosuperior displacement of the infundibular septum.
*Is the Most common cause of early childhood cyanosis.
whats the disease? what are the 4 main features?
Tetrologoy of Fallot
Pulmonary infundibular stenosis (most important determinant for prognosis)
Right ventricular hypertrophy (RVH)— boot-shaped heart on CXR
Overriding aorta
VSD (harsh systolic murmur)
Clinical syndrome characterized by acute onset respiratory failure, bilateral lung opacities “white out on CXR), LOW Pao2/Fio2, _no evidence of HF/ fluid overload.= NORMAL PCWP._
whats the diagnosis and what is characteristically seen on histo?
ARDS
Intra-alveolar hyaline membranes
what the MOA behind the AE of osteoporosis caused by corticosteroid use

man has a painless scrotal mass
no transillumination
PALPABLE WHEN STANDING BUT DISAPPEARS WHEN LAYING RECUMBANT
whats the Dx?
VARICOCELE
note: testicular cancer, spermatocele, testicular torsion DO NOT change in size when laying and although a communicating HYDROCELE (patent process vaginalis) DOES change in size it TRANSILLUMINATES SO varicocele is the only option
know how to seperate wernicke encephalopathy from korsakoff syndrome.
wernicke you get, for eaxmple. from thiamine def and it has a triad of
- ataxia
- confusion
- oculomotor dysfuntion
that resolves when given thiamine
KORSAKOFF is A COMPLICATION OF WERNICKE AND its hallmarks are PERMAMENT MEMORY LOSS AND CONFABULATION!
describe the extensive step wise tx of RA
NSAIDs, glucocorticoids,
use as a BRIDGE TO
disease-modifying agents ((DMARDS)
- methotrexate
- sulfasalazine,
- hydroxychloroquine,
- leflunomide
and when DMARDS dont work try: TNF-a inhibitors
- Etanercept -(Fusion protein (receptor for TNF-α + IgG1 Fc), produced by recombinant DNA. its a tnf decoy receptor
- Infiximab & adalimumab [Anti-TNF-α monoclonal antibody]
whats the MOA of diphendyramine of Dimenhydrinate or Meclizine?
1st gen: Reversible inhibitors of H1 histamine receptors (can cross BBB).
used for
- Allergy
- motion sickness (THIS IS DUE TO THEIR Antagonist effect at muscarinic-3 (M3) receptors)
- b (bc since they cross the BBB and have CENTRAL effects too, they cause drowsiness)

which Plasmodium class has an exoerythrocytic (dormant form (hypnozoite) in liver) form?
and how would you treat this?
is there a particular AE to look out for ?
For P vivax/ovale (not falciparum),
this how you would treat
Chloroquine (for sensitive species), which blocks Plasmodium heme polymerase;
if resistant, use mefloquine or atovaquone/ proguanil
If life-threatening, use intravenous quinidine or artesunate (test for G6PD de ciency)
AAAAND FINALLY TO ANSWER THE ACTUAL Q:
add primaquine for the exoerythrocytic (dormant form (hypnozoite) in liver)
(test for G6PD de ciency)!!!!!!
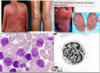
17 y/o boy
non blanching palpable purpura after taking penicilin
on biopsy what wil you see?
leukocytoclastic (cutaneous small vessel vasculitis) vasculitis!!!! (shows fragmented neutrophili nuclei + inflamed smal bv’s with Fibrinoid necrosis)
this only affects the skin and normally arises from exposure to a drug or pathogen (Hep B or C virus or penicillin, cephalsporin)
similar to what is seen in in HENOCH (leukocytoclastic angitis + IgA + C3)
which 2 vasculitis’ give you +ve p-ANCA
Microscopic Polyangitis & Churg-Strauss (eosinophilic granulomatosis with polyangitis)
Does COX-1 or COX-2 protect the GI mucosa? and how? explain which SPECIFIC PGs are made from each pathway and their diff fxs.
COX-1 (from PLTS) makes TXA2 + PGI2 and E2 where as
COX-2 (from ENDOTHELIUM) two makes PGI2
PGE2 is PROTECTIVE TO GI MUCOSA SO COX-1 IS MORE PROTECTIVE TO GI MUCOSA.
note: PGI2 is in charge of 1. dec plt. aggregation 2. vasodilation
where as COX-1 makes TXA2 which opposes (or balances) PGI2 by promoting PLT aggregation + vasoCONSTRICTION
where is the biggest O2 content difference when compared to the Aorta (that has High O2 content)?
pick one
Pulmonary Artery
IJV
Hepatic Vein
Coronary Sinus
Brachial Vein
you may want to say Pulmonary Artery BUT NO! answer is = CORONARY SINUS
the coronary sinus receives blood from the cardiac veins which are the most DEOXYgenated (O2 poor) veins in the body bc EXTRACTION/use/sucking up of O2 in the heart is the greatest out of all the veins in the body (eg: skeletal muscle) so since the CORONARY SINUS receives blood from the cardiac vein and gives it to the RA, IT IS THE PLACE THAT RECEIVES THE LEASE OXYGENATED BLOOD.
AGAIN, why not the PA?
bc it receives blood from the Coronary sinus (via the right hear) ANDDDD also from the vena cava which is MORE oxygenated than the plain ‘ol cardiac veins so since Coronary sinus JUST received SUPER SUPER DEOXY BLOOD IT IS THE PLACE THAT DIFFERS THE MOST FROM THE AORTA AS FAR AS O2 CONTENT.
main mode of transmission of HEP A?
Blood!!!!!
(IVDU, post- transfusion)
how do the levels of absorption and hence levels of Dxylose measured in blood & urine CHANGE in
- pancreatic insufficiency or removal of panc
- GI mucosal defects
- bacterial overgrowth
- NO CHange! if panc messed up it can still be absorbed bc dxylose is a MONOsaccharide (like galactose and gllucose) so they can be absorbed at proximal SI by either fac diffuusion or the SGLT1
the other 2 would DECREASE levels of dxylose seen in urine and blood
which disease has the following characteristics:
female of reproductive age
Verrucous (Libman-Sacks) Endocarditis—nonbacterial, verrucous thrombi usually on mitral or aortic valve. (DESCRIBE THE VEGETATIONS SEEN on the valve leaflets)
Associated with diffuse proliferative glomeruloneprhitis (proliferative and necrotizing lesions with crescent formation during active disease)
-what does this light microscopy look like? (looking for a buzz word here)
SLE
vegetations are seen on BOTH surfaces of valve leaflets and are composed of STERILE platelet thrombi interwined with strands of fibrin, immunecomplexes and mononuclear cells. *they are easily dislodged and can result in systemic embolization.
LM: diffuse thickennig of the glomerular capillary walls with “WIRE LOOP” structures due to subendothelial immune complex deposition”
after passing the inguinal ligament, the external iliac artery becomes the_______
Common femoral artery
What accounts for HCVs genetic instability during the replication process?
lack of 3-5’ exonuclease activity
or
lack of 5-3’ exonuclease actiivity?
they vary at sequences encoding for its 2 envelope glycoproteins
lacks 5-3’ exonuclase activity!!!!
pt with
RUQ pain (acute onset) + nausea + vomit
receiving TPN (total parenteral nutrition)
moderate leukocytosis
gallstones seen on ultrasound
why/how does TPM lead to the complication of Gallstones?
qID: 77
normally, enteral passage of fatty acids & amino acids into the duodenum–> +release of CCK–> contraction of gall bladder.
if TPN=no enteral stimuation–> no CCK released–> BILIARY STASIS–> INC RISK OF GALL STONES
side note: resection of the ileum ca also cause inc risk of gall stones due disruption of normal enterohepatic circulation of bile acids
PATIENT HAS SEPSIS AND SHOCK after pnm and after three days his hb levels drop and nasogastric suction shows bright read blood?
why?
bc THE SHOCK AND SEPSIS DECREASES BLOOD FLOW TO MUCOSA AND THIS LEADS TO “STRESS RELATED MUCOSAL INJURY!!”
LIKE HELLO…THIS IS ACUTE GASTRITIS!! EROSIONS AND THEY CAN ALSO PERFORATE.
REMEMBER WE think of nsaids and cushings and curling ulcers but SHOCK is a huge one bc our stomach NEEDS BLOOD AS A PROTECTIVE BARRIER!!!!!!!!
27-year-old primigravid woman at 18 weeks gestation comes to physician for routine prenatal examination. The uterus consistent in size with 18 week gestation. Ultrasonography shows a male fetus. The collecting system and pelvis of the left kidney is dilated and the renal cortex appears compressed.
The left and right ureters are not dilated. The right kidney appears normal. Amniotic fluid volume is normal. Which causing renal finding in this fetus ?
Incomplete recanalization of proximal ureter
a patient with a taenia infection in the intestine or (intestinal tapeworm) or Cysticercosis (eg: in muscle) would be treated with Praziquantel
BUT
neurocysticercosis is treated with….
albendazole !!!!!! for neurocysticercosis
t(8;14)—translocation of c-myc (8) and heavy-chain Ig (14)
t(14;18)—translocation of heavy-chain Ig (14) and BCL-2 (18)
t(11;14)—translocation of cyclin D1 (11) and heavy-chain Ig (14)
t(8;14)—translocation of c-myc (8) and heavy-chain Ig (14)———–Burkitt lymphoma
t(14;18)—translocation of heavy-chain Ig (14) and BCL-2 (18)———-Follicular lymphoma
t(11;14)—translocation of cyclin D1 (11) and heavy-chain Ig (14) ——–Mantle cell lymphoma
anti-U1 RNP (speckled ANA) antibodies are associated with….
MIXED CONNECTIVE TISSUE DISEASE
diff btw libman sacs endocarditis and bacterial endocarditis?
LS endo has vegetations composed of sterile platelet thrombi with immune complexes (SMALL) vegetations on both surfaces of valve)-mitral and aortic
Bacterial endocarditis has LARGE vegetations on valve cusps that contain inflammatory cells and bacteria (staph or strep)
both contain fibrin
homeless alcholic man ingests ethylene glycol and 24-72 hours later will manigest with signs of acute renal failure bc he has ATN….what is his acid base status?
WHATS THE ANTIDOTE FOR ETHYLENE GLYCOL?
MOA?
IS THIS ANTIDOTE USED FOR ANYTHING ELSE?
HIGH ANION GAP METABOLIC ACIDOSIS
FOMEPIZOLE: INHIBITS ALCOHOL DH
(cant go from ethanol to acetaldehyde)
can also use for METHANOL INTOX
Nf kappa beta normally does what and what drug class inhibiits it classically?
Nf kappa beta normally upregulates synthesis of inflammatory proteins
Corticosteroids
The pathognomonic microscopic feature in this disease is the GRANULOMATOUS TISSUE CONTAINING lipid-laden foamy macrophage
Xanthogranulomatous Pyelonephritis
what are the 3 main complications associated with the disease that is confirmed when Asbestos (ferruginous) bodies are golden-brown fusiform rods resembling dumbbells are found in alveolar septum sputum sample, visualized using Prussian blue stain, often obtained by bronchoalveolar lavage.
Risk of
1. bronchogenic carcinoma >> 2. risk of mesothelioma.
3. risk of pleural effusions.
what oxidase +ve bug causes Contact lens keratitis? and whats the property of this bug that enables this?
pseudomonas
can form a biofilm
4 main manifestations of Protein malnutrition—–Kwashiorkor
Kwashiorkor results from a protein-deficient (carbs>protein) BUT total caloric intake is NORMAL (unlike marasmus)
kid with big belly (ASCITES!) + dec CMI (inc risk for parasites) +Apathy, listlessness, poor appetite –> POOR PROGNOSIS!!
MEAL:
Malnutrition
Edema (pittng)
Anemia: RBC hypoplasia; iron/ folic acid/vitamin B12 deficiencies
Liver (fatty)–(due to dec apolipoprotein synthesis..NEED APO B100 FOR vldl to leave liver)–> massive hepatomegaly
dont confuse with Marasmus! which is Total calorie malnutrition resulting in emaciation (tissue and muscle wasting, loss of subcutaneous fat); +/– edema.
HYPOPLASTIC THYMUS (absent thymic shadow) is seen in…name 2 diseases
DI GEORGE (low Ca2+)
SCID (normal Ca2+)
fibrinoid necrosis is seen in what two disease processes
- Vasculitis (eg: PAN)
- Malignant HTN
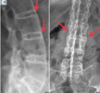
whats the diagosis? whats the genetic principle underlying this disease?
hyperphagia, obesity, intellectual disability (mental retardation), hypogonadism, and hypotonia, almond shaped eyes, temperature instability,
balanced translocation at chr. 15
this disease is due to deleted/mutated genes on CHROMOSOME 15!!!!
PRADER WILLI syndrome!
IMPRINTING!!!!
At some loci, only one allele is active; the other is inactive (imprinted/inactivated by methylation). With one allele inactivated, deletion of the active allele disease.
25% of cases due to maternal uniparental disomy (two maternally imprinted genes are received; no paternal gene received).
proximal tubular cell balooning and vacuolar degeneration in a pt with acute renal failure who has Ca2+ oxalate crystals (buzz word for this!) has ATN bc of why?
WHAT PT POPULATION SHOULD YOU WATCH OUT FOR AS HAVING A TENDENCY TO BE ASSOCIATED WITH THIS
ethylene glycol!!!!
glycolic acid is toxic to tubule cells AND
oxalic acid precipates to Ca2+ OXALATE stones!!!!!!!!!
watch out for antifreeze ingestion in (homeless) ALCOHOLIC PTS bc they ingest it in place of alcohol!
massive consumption of EGG whites (which contain lots of Avidin) can lead to what vit def?
BIOTIN!!!! b7!!!!!!!
avidin binds b7 and prevents its reabsorption
needed for carboxylase reactions
which need ABCs
ATP
Biotin (b7)
Co2
what are two diseases that are commonly associated as examples of the concept of Mosaiciam
Turners syndrome (XO and XX in one person)
McCune Albright Syndrome
[due to mutation affecting G-protein signaling. Presents with unilateral café-au-lait spots, polyostotic
brous dysplasia,precocious puberty,multiple endocrine abnormalities.
—–Lethal if mutation occurs before fertilization (affecting all cells), but survivable in patients with mosaicism.
what is the difference in how a a person with HIV is affected by CANDIDA versus a person who is NEUTROPENIC?
[this is very important]
side question: what other bug is known to affect neutropenic pts?
T cells (Th) protect against SUPERFICIAL Candida infections (oral, cutaneous, vulvovaginitis, MUCOCUTANOUS) so someone with HIV who has a LOW T CELLS COUNT is affected with SUPERFICIAL CANDIDIASSIS
VERSUS
NEUTROPHILS PREVENT HEMATOGENOUS SPREAD OF CANDIDA (dissemmmmminated infections: CANDIDEMIA/endocarditis) affected NEUTROPENIC PTS or otherwise immunocompromised (CHEMOTHERAPY or INHERITED IMPAIRMENTS OF PHAGOCYTOSIS)
aspergillus and psuedomonas bad for neutropenics too
GIVE ALL THE MAIN EFFECTS OF CORTISOL
THINK: Cortisol is a “BIG FIB”
WHAT AE CAN Exogenous corticosteroids HAVE AS IT RELATES TO TWO SPECIFIC MICROBIAL INFECTIONS?
INC Blood pressure:
- Upregulates α1-receptors on arterioles
sensitivity to norepinephrine and
epinephrine
- At high concentrations, can bind to
mineralocorticoid (aldosterone) receptors
INC Insulin resistance (diabetogenic)
INC Gluconeogenesis, lipolysis, and proteolysis DEC Fibroblast activity (causes striae) InFLammatory and Immune responses:
- Inhibits production of leukotrienes and prostaglandins
- Inhibits WBC adhesion neutrophilia!!!! INCREASED NEUTROPHILS BC NOT MARGINATING!
- Blocks histamine release from mast cells
- Reduces eosinophils
- Blocks IL-2 production
DEC Bone formation ( DEC osteoblast activity)
Exogenous corticosteroids can cause reactivation of TB and candidiasis (blocks IL-2 production).
what are 3 RFs for Neonatal respiratory distress syndrome?
- Prematurity
- Maternal diabetes (due to fetal insulin)
- C-section delivery (release of fetal glucocorticoids).
Trypanosoma cruzi
which causes
Chagas disease—dilated cardiomyopathy with
apical atrophy, megacolon, megaesophagus; predominantly in South America
Unilateral periorbital swelling (Romaña sign) characteristic of acute stage
is transmitted by WHAT and is treated HOW
Reduviid bug (“kissing bug”) feces, deposited in a painless bite (much like a kiss)
Benznidazole
or nifurtimox;
Cruzing in my Benz, with a fur coat on
is Sirolimus (Rapamycin) M TOR inhibitor NEPHROTOXIC?
what drug is is SYNERGISTIC WITH
NO!!!!!!!!
hence why it can be synergistic with Cyclsporine which IS nephrotoxic
abnormal ristocetin cofactor activity—no aggregation upon addition of Ristocetin…….
WHAT DISEAES IS THIS DIAGNOSTIC FOR
-how does this Ristocetin cofactor assay work?
whats one weird-ish treatment for this disease but totally makes sense once you know the MOA?
von Willebrand disease
Platelet agglutination caused by ristocetin can occur only in the presence of von Willebrand factor multimers, so if ristocetin is added to blood lacking the vwf, the platelets will not clump.
The antibiotic ristocetin causes von Willebrand factor to bind the platelet receptor glycoprotein Ib (GpIb), so when ristocetin is added to normal blood, it causes agglutination.
Treatment: desmopressin, which releases vWF stored in endothelium.
alcoholic takes acetaminophen
now he is jaundice
has inc PT
and real high AST
whats the pathogenesis
too much NADH?
not enough glutathione?
Overdose produces hepatic necrosis; acetaminophen metabolite (NAPQI) depletes glutathione —> and forms toxic tissue byproducts in liver.
N-acetylcysteine is antidote—regenerates glutathione.
Minoxidil
what would be the effect of placing Minoxidil in a solution of just saline and THEN adding a piece of vascular Sm to it?
DIRECT vasodilation
Minoxidil is a Direct arteriolar vasodilator.
uses for:
-Androgenetic alopecia
severe refractory hypertension.
note that the fact that norepi or epi but just saline were added to the solution IMPLIES the the effect of this drug MUST be a direct effect on vasc sm NOT one mediated IN THE PRESENCE of norep or epi
which is why adding something like Phentolamine would NOT cause the same vasodilatory effect even though we think of an alpha antag as opposing vasocontstriction and hence vasodilating. but it does it in the presence of Norepi. (thats the catch)

causes ORAL ULCERRRRR
can survive INTRACELLULARLY
prediliction for mononuclear phagocyte system so can lead to HEPATOSPLENOMEGALY
cannot be transmitted person to person unlike to TB but like TB can form granulomas
its smaller than an RBC
its a mold in the cold and a yeast in the heat
bird or bat droppings!!!!
its HIDES in macrophages
can cause pnm in a health chap but disseminates in IC people
what organism is this
HISTOPLASMOSIS
what are the labs values like for a pt
who is pregnant or taking OCPs?
give what the levels of Transferrin (TIBC) and
% Transferrin Saturation would be and why
(inc Transferrin; dec % sat Transferrin)
Estrogen (as is seen in inc amt in both Pregnancy & OCP use)—> upregulation of TRANSFERRIN SYNTHESIS in the liver
this, in turn, alters the ratio that makes up % Transferrin Saturation):
Fe2+: TIBC
same as:
Fe2+/TIBC
in such a way that bc the liver is making MORE TIBC and the amt of Fe2+ has not changed or is even DEC in pregnancy bc of INC demand, the numerator gets smaller so the %saturation DECREASES
On inspirtation, is Jug Venous pressure supposed to normally increase or decrease?
what is it called when this normal way doesnt happen?
JVP is supposed to DECREASE on inspiration
Kussamaul sign: JVP increases on inspiration instead. seen in:
Constrictive pericarditis
Restrictive CM
RA or RV tumors
which disease is being described:
can present as severe hemorrhagic diathesis due to vitamin K deficiency (which creates a HYPOcoagulable state) and bleeding.
is an unusual susceptibility to bleed (hemorrhage) mostly due to hypocoagulability, in turn caused by a coagulopathy (a defect in the system of coagulation). Several types are distinguished, ranging from mild to lethal.
Celiac sprue
(due to malabsortion)
young child
not vacinnated
paroxysm of machine gun-like coughing and forced expiratory grunt
INC LEUKOCYTES WITH LYMPHOCYTE PREDOMINANCE
the culprit of this condition has “defective Neutrophil chemotaxis and oxidative metabilism due to increased activity of ADENYLYL CYCLASE (cAMP)
whats the orgnaism, describe it, what stain, name the clinical disease and whats the MOA behind this Increased cAMP?
B. pertussis
grame -ve cocobacillus
stain = Bordet Gengou medium
“WHOOPING COUGH”
PERTUSSIS EXOTOXIN (ab toxin) Overactivates adenylate cyclase (cAMP) by disabling Gi, impairing phagocytosis to permit survival of microbe.
what lung cancer is this
grows along alveolar septa—> apparent “thickening” of alveolar walls.
Tall, columnar cells containing mucus.
its a subtype of adenocarcinoma IN SITU !!!!!
called: Bronchioloalveolar subtype
mucin +ve! Just like adenocarcinoma!
what in the world is so unique about Trypanosoma brucei?
what is a big diff btw Trypanosoma brucei & Trypanosoma cruzi
famously causes recurring fever (due to antigenic variation)!!!!!!! changes its VARIANT SURFACE GLYCOPROTEINs every time host mounts and immune response!!!!
Trypanosoma brucei = Tsetse fly= a PAINFUL bite
Trypanosoma cruzi = Reduviid bug (“kissing bug”) feces, deposited in a PAINLESS bite (much like a kiss)
Lymphocytes are derived from
Lymphocytes of mesenchymal origin.
what vit deficiency can OCPs lead to clasically?
Vit b6!!! (PLP)
along with INH
Aldesleukin (IL-2) is used to treat what two conditions mainly?
Renal cell carcinoma
metastatic melanoma
which lung cancer can secrete b-hcg?
large cell lung ca
Highly anaplastic undifferentiated tumor; poor prognosis. Less responsive to chemotherapy; removed surgically.
peripheral location
Homer-Wright rosettes characteristic of:

neuroblastoma and medulloblastoma.
whats the AE of having LOW Mg2+?
Tetany, torsades de pointes, hypokalemia
anti-Jo-1 abs are AKA?
what disease has these?
whats it like on histo?
CD4 OR 8 + T CELLS?
WHATS THE MAIN MANIFESTATION?
what other antibody is associated with it?
anti-histidyl trna synthetase abs!!!!
POLYMYOSITIS
ENDOMYSIAL (vs PERImysial inflamm in Dermatomyositis) INFLAMMATION WIHT CD8+ T CELLS
PROGRESSIVE/INSIDIOUS PROXIMAL MUSCLE WEAKNESS “TROUBLE GOING UP STAIRS, GETTING OUT OF CHAIR”
ANA ab
ANTI-SRP ab
ANTI-Mi-2 ab
Increased CK and aldolase in serum
segemental demyelination of peripheral nerves with ENDONEURAL INFLAMMATORY INFILTRATE (with lymps and macs) is CHARACTERISTIC OF WHAT
GUILLAIN BARRE!
(aka: acute inflammatory demyelinating polyradiculopathy)
herniation of gallbladder mucosa into the muscular wall
is histologically called what and is associated with what type of Gall bladder disorder?
CHRONIC CHOLECYSTITIS
(Rokitansky-Aschotf sinus,
Chronic inflammation of the gallbladder
Due to chemical irritation from longstanding cholelithiasis, with or without
superimposed bouts of acute cholecystitis
Characterized by herniation of gallbladder mucosa into the muscular wall
(Rokitansky-Aschotf sinus, Fig. 11.3A)
Presents with vague right upper quadrant pain, especially after eating
Porcelain gallbladder is a late complication (Fig. 11.3B).
- Shrunken, hard gallbladder due to chronic inflammation, fibrosis, and dystrophic calcification

AE of heparin?
one REALLY IMPORTANT ONE
Bleeding, thrombocytopenia (HIT), osteoporosis drug-drug interactions.
(NOTE: enoxaparin, dalteparin: LMWH does NOT cause osteoporosis),
Heparin-induced thrombocytopenia (HIT)—development of IgG antibodies against heparin- bound platelet factor 4 (PF4) BC (this complex acts as a hapten) THAT ACTIVATES our immune system to form those antibodies
Antibody-heparin-PF4 complex (now all three things are together forming a complex which THEN activates platelets–> thrombosis and thrombocytopenia (due to depletion).
For rapid reversal (antidote), use protamine sulfate (positively charged molecule that binds negatively charged heparin).
- note: PF-4 is a chemokine that is released from alpha-granules of activated platelets during platelet aggregation, and promotes blood coagulation by moderating the effects of heparin-like molecules*
- replace hep with*
- direct thrombin inhibitors (argatroban,*
- bivalirudin, dabigatran)*
name 4 toxins that are taken up via retrograde axonal transport
polio
rabies
herpes
tetanus toxins
are (except herpes which is taken up via sensory fibers) take up via retrograde trasports via axons that innervate skeletal muscle
how much of the tensile strength will be regained after 3 months time in a scar?
70–80% of tensile strength regained at 3 months;
little additional tensile strength will be regained afterward.
what interleukin is used to treat Thrombocytopenia? number and pharm name
Oprelvekin (IL-11)
Restrictive lung diseases can be due to Interstitial lung diseases or Poor breathing mechanics, for example due to:
1. Poor muscular effort: LIST 3 EXAMPLES
2. Poor structural apparatus: LIST 2 EXAMPLES
what is the AA gradient in these?
these are due to Poor breathing mechanics, not an interstitial lung issue so the DIFFUSING CAPACITY is UNAFFECTED and therefore–> normal A-a gradient):
the issue is Extrapulmonary, peripheral hypoventilation (normal Aa with Hypoventilation, we know this)
Poor muscular effort—polio, myasthenia gravis, Guillain-Barré syndrome
Poor muscular effort—scoliosis, morbid obesity
anti-smooth muscle abs seen in
autoimmune hepatitis
middle aged woman with sxs of chronic hep
List all the CYP450 INDUCERS
SCR(a)PP NC BIGG
St. John’s wort
Chronic alcohol use
Rifampin
(a)
Phenytoin
Phenobarbital
Nevirapine (NNRTI)
Carbamazepine
Griseofulvin
Ginseng
&
which vitamin can prevent morbidity and mortality from MEASLES (rubeola) especially in kids?
only ONE single association here.
VIT A!!!!!!!!!
whats the relationship betwen cross sectional area and resistance to flow?
where is resistance to flow the LEAST in the respiratory tree?
and why????
Resistanace=P/Area x Velocity
note: also the relationship btw Cross sectional area and Velocity of flow are INVERSE. inc A (cross sectional area)–> DEC in Velocity of flow. (look at how flow velocity is different in capillaries vs, venules etc (KNOW THIS CONCEPT)-there are graphs showing this
so if you increase cross sectional area you DECREASE resistance to flow as is seen in the TERMINAL bronchioles where resistance to flow is the LEAST of anywhere in the Respiratory tree and this is bc even though the diameters of the term are small there are many (inc cross sectional area) lined up in PARALLEL so this decreases the resistnace!
(highest resistnace is seen in MEDIUM sized bronchii like: segmental and lobar bronchi)
STERILE PYuria
and NEGATIVE urine cultures
suggests what UGI infection
neisseria
or
chlamydia
URETHRITIS!
sterile pyuria is wbcs in urine “without bacteria”—but this is bc neiss and chlam are not seen on a gram culture!
systemic mastocytosis
what the hell is that


whats the urachus?
if a remnant of the urachus remains, what cancer can this cause?
In the 3rd week the
yolk sac forms the–> allantois, which extends into urogenital sinus.—> Allantois becomes the—> urachus (a duct between fetal bladder and umbilicus)
yolk sac—> allontois—> urachus
ADENOCARCINOMA OF THE BLADDDDERRR!!!!!!!
1. a urachal remnant-eg: urachal cyst (fluid-filled cavity lined with uroepithelium, between
umbilicus and bladder) -(tumor develops at the DOME of the bladder),
LIST 3 drugs with Zero-order elimination
[Capacity-limited elimination] not flow dependent like first order elim
Examples of drugs—
Phenytoin, Ethanol, and Aspirin (at high or toxic concentrations).
Rate of elimination is constant regardless of Cp (ie, constant AMOUNT of drug eliminated per unit time).
Calcium phosphate needs inc or dec PH to form?
how about calcium oxalate?
Calcium phosphate: INC pH
hypocitraturia (with DEC ph)–> calcium oxalate or phosphate
radioopaque can see on xray
which local anesthetics (in the Amide category) has an AE of: severe cardiovascular toxicity
Bupivacaine
note: Esters just have 1 “i” in their name, ulike the amides.
but both end in: -caine
Red “currant jelly” stools means what in an adult vs an infant?
Acute mesenteric ischemia (adults)
intussusception (children)
whats the most common presentation of an eldersly person with atherosclerosis who has ATHERO-EMBOLIC disease after an invasive procedure, like an cardiac catheritizatoin)
ATHERO-EMBOLIC DISEASE (THINK ABOUT THE NAME)
-during that invasive procedure like aortic catheritizatoin, CHOLESTEROL containing debris can DISLODGE and travel to smaller vessels where they block the area and cause ischemia to that tissue which presents a few days to weeks post surgery as:
MOST COMMONLY:
acute kidney injury!!!! (oliguria and azotemia)—-THE PATIENT WOULD NOT HAVE A FRANK INFARCTION WITH HEMATURIA AND FLANK PAIN AND THE WHOLE SHABANG BC CHOLESTEROL EMBOLI ARE WITTLE.
ON HISTO (if in the kidney) you could see needle shaped cholesterol clefts that partially or completely obstruct the arcuate or intralobular renal arteries
other organs that can be involved are: GI, CNS (like retina vessels)
what makes up the RMP of a muscle cell whose RMP is -70?
High K+ conductance (efflux) and some Na+ conductance
“no platelet clumping” seen on blood smear.
what diseae?
what are the labs
Glanzmann thrombasthenia
DEC GpIIb/IIIa–> defect in platelet-to-platelet aggregation.
Labs: blood smear shows no platelet clumping + INC BT
the are characteristic labs of what disease
Findings: CSF protein with normal WBC cell count (albuminocytologic dissociation).
protein may cause papilledema.
Guillain-Barré syndrome.
IV drug users who get infected with candida can get WHAT manifestation?
endocarditis!!!!!
from candida! in (IV drug users)
what is the
- pathogenesis
- lab values seen (are these same lab values shared with any other disease?)
- treatment for
Hemochromatosis
- pathogenesis: Recessive mutations in HFE gene (C282Y chromosome 6) abnormal iron sensing and INCREASED intestinal absorption
2. LABS: (INC ferritin, INC iron, DEC TIBC–>INC transferrin saturation)—SAME as SIDEROBLASTIC ANEMIA
- TX: repeated phlebotomy, chelation with deferasirox, deferoxamine, oral deferiprone.
what genetic principle is this an example of?
Different mutations
in the same locus
produce the same phenotype.
give 2 relevant clinical examples of this.
Allelic heterogeneity
- b or a-Thalassemia
- G6PD deficiency (there are over 400 diff mutations on the same disease-causing locus in G6PD that are knows to cause this deficiency)
if a Diabetic patient taking diurects (volume depleted)
shows albuminuria
so you decide to give her an ACE-I to treat her “early diabetic nephropathy”
and then the next day the pt returns to you and says they are lightheaded and almost fainted,
why is this happening?
first dose HYPOtension (AE) can occur if someone is volume depleted and also takes an ACE-I since they block vasoconstriction
Degenerative disorder of CNS associated with Lewy bodies (composed of α-synuclein—intracellular eosinophilic inclusions
brain slice on gross looks like…

the pathologic hallmark of Parkinson’s disease remains synuclein-filled Lewy bodies in the nigrostriatal system.
eg:
67-year-old man with 1 year progressive difficulty writing and walking. Pt is stooped and talks slowly. PE shows bland facial expression, fine resting tremor in both hands, no tremor when moves, walks with difficulty starting and stopping, cogwheel rigidity.
Brain tissue histology shown as well as gross cross sections of midbrain both normal and diseased.

whats the MOA of (sodium) NITROPRUSSIDE?
whats the main AE? and what can you give as an antidote?
WHATS SITUATION IS IT USED IN as the DOC?
MOA is that NITROPURSSIDE DIIIIRREEECCCTTTLLLLYYYYYYYYY releases NO and causes and increase in cGMP leading to VASO and VENO dilation and is the:
DOC for HYPERTENSIVE 911’s bc of its SHORT t1/2
main AE= CN toxicity (cn is a metabolite)
antidote: SODIUM THIOSULFATE helps make thiocyanate which can be eliminated:)
what are the TWO DIFFERENT mechanisms by which THYROID HORMONE INC SNS ACTIVITY AND BASAL METABOLIC RATE?
INC SNS activity: via stim of β1 receptors in heart = CO, HR, SV, contractility
INC basal metabolic rate via INC synthesis of: Na+/K+-ATPase!!!!!!!!!!!!!!!–> activity INC O2 consumption, RR, body temperature!!!!!!!!
what two lab values are INC in
Wiskott-Aldrich syndrome
Mutation in WAS gene;
T cells unable to reorganize actin cytoskeleton.
X-linked recessive.
INC
IgA!!!!
IgE!!!!!
WATER
what are the 3 main (general) RFs contributing to the general formation of Gall bladder stones (cholelithiasis)
INC cholesterol and/or bilirubin
DEC bile salts,
gallbladder stasis
all cause stones
a PRIMARY CNS lymphoma.
whats is the FIRST AND MAIN ASSOCIATION you should think of ?
HIV/AIDS!!!!!!!!!!!!!!!!!!!
Considered an AIDS-defining illness.
Variable presentation: confusion, memory loss, seizures. Mass lesion(s) on MRI, needs to be distinguished from toxoplasmosis via CSF analysis or other lab tests.
what are the three ways one could get ADENO CA of the bladder
weird, right?
note: these all have to be things that either already have glandular columnar epi or cause it to form
(bc normally bladder is transitional epi)
Malignant proliferation of glands, usually involving bladder
Arises from
- a urachal remnant-eg: urachal cyst-(tumor develops at the DOME of the bladder),
- cystitis glandularis (causes columnar metaplasia!)
- bladder exstrophy (congenital failure to form the caudal portion of the anterior abdominal and bladder walls)…bc bladder exposed to outside world and can cause is to get cancer and change epi
Endometriosis. what are some defining features that make it DIFF from leiomyoma
Non-neoplastic endometrial glands/stroma outside endometrial cavity F . Can be found anywhere; most common sites are ovary (frequently bilateral), pelvis, peritoneum. In ovary, appears as endometrioma (blood- lled “chocolate cyst”).
May be due to retrograde ow, metaplastic transformation of multipotent cells, transportation of endometrial tissue via lymphatic system.
Characterized by cyclic pelvic pain, bleeding, dysmenorrhea, dyspareunia, dyschezia (pain with defecation), infertility; normal-sized uterus.
NSAIDs, OCPs, progestins, GnRH agonists, danazol, laparoscopic removal.
Symptoms can vary depending on location of implants.
ITS CYCLICAL and IT HURTS!!!
leiomyomacause===> abnormal uterine bleeding, or result in miscarriage. Severe bleeding may lead to iron de ciency anemia.
extra manifestations of endometriosis!
- Large intestine: Pain during defecation, abdominal bloating, or rectal bleeding during menses!!!!!!!!!!!!!
- Bladder: Dysuria, hematuria, suprapubic pain (particularly during urination), or a combination
- Ovaries: Formation of an endometrioma (a 2- to 10-cm cystic mass localized to an ovary), which occasionally ruptures or leaks, causing acute abdominal pain and peritoneal signs
- Adnexal structures: Formation of adnexal adhesions, resulting in a pelvic mass • Extrapelvic structures: Vague abdominal pain (sometimes)
HEMATOCHEZIA IS MOST COMMONLY ASSOCIATED WITH WHAT TWO CAUSES OF GI BLEEDING
DIVERTICULOSIS (left sided!)
ANGIODYSPLASIA (right sided!
--cecum, terminal ileum, ascending colon
BOTH COMMON IN PPL GREATER THAN 60
also ischemia colitis (colonic ischemia) which unlike acute (due to embolism in SMA) and chronic mesenteric ischemia (due to atherosclerosis of celiac, sma, or ima), is NOT due to obstruction.
*while the mesenteric ischemias present with lots of pain
Colonic ischemia is due to HYPOPERFUSION eg: Hypotension; presents with crampy pain
pyloric stenosis is associated with WHAT class of antibiotics?
billious or non billious vomit?
whats the clinical buzz word?
whats the time frame relative to birth?
MACROLIDES!!!!!!
NON billious (unike duodenal atresia)
“palpable olive mass” in the epigastric region
2-6 WEEKS post birth (inlike duodenal atresia seen 1-2 DAYS)
side note on AE of macrolides:
MACRO:
Gastrointestinal Motility issues**************
Arrhythmia caused by prolonged QT interval
acute Cholestatic hepatitis,
Rash,
eOsinophilia
phenytoin, sulfonamides, methotrexate, trimethoprim all have in common that they can cause what type of vit def?
what are the labs in this def?
homocysteine & methylmalonic acid levels specifically.
WHY?
draw out the pathway please
folate vit b9
INC homocysteine
normal methylmalonic acid levels.
read the description to understand also refer to FA for a simpler version of the pathway

new holosystolic murmur
Immune mediated Type II hypersensiticity (due to molecular mimicry)
Interstitial myocardial granulomas (which have another name)
10 year old boy with: fever, poor appetite, hypotension, tachycardia (are sxs of what characteristic finding in this disease process)
what disease
*Rheumatic fever
*Immune mediated (type II hypersensitivity); not a direct effect of bacteria. Antibodies to M protein cross-react with self antigens (molecular mimicry).
*Interstitial myocardial granulomas aka: ASCHOFF BODIES
*Murmur bc an Early lesion is mitral valve regurgitation
boy had signs and sxs of MYOCARDITIS
Amphotericin B & sodium stibogluconate treat a condition that is diagnosed by seeing
Macrophages containing amastigotes
what condition is this
Visceral leishmaniasis (kala-azar)—spiking fevers, hepatosplenomegaly, pancytopenia
Cutaneous leishmaniasis—skin ulcers
Sandfly trasmits it!!!
its a protozoal infection
resting membrane potential for a cells is determined by conductance of….
high K+ conductance
(some) Na+ conductance
what cytokine is inc in Multiple Myeloma?
what type of Amyloidosis is seen?
IL-6
It has been demonstrated to be involved in the proliferation of plasmablastic cells in bone marrow and in the differentiation of these cells into mature plasma cells.
AL (primary) 1º AMYLOIDOSIS!!!!
Due to deposition of proteins from Ig Light chains. Can occur as a plasma cell disorder or associated with multiple myeloma. Often affects multiple organ systems, including renal (nephrotic syndrome), cardiac (restrictive cardiomyopathy, arrhythmia), hematologic (easy bruising, splenomegaly), GI (hepatomegaly), and neurologic (neuropathy).
compare type 1 and 2 diabetes in all the ways you can

Rib notching (inferior surface, on x-ray) is seen in what condition commonly how come?
Coarctation of the aorta
Aortic narrowing near insertion of ductus arteriosus (“juxtaductal”).
Associated with bicuspid aortic valve, other heart defects, and Turner syndrome.
Hypertension in upper extremities and weak, delayed pulse in lower extremities (brachial-femoral delay).
With age, intercostal arteries enlarge due to collateral circulation; arteries erode ribs notched appearance on CXR.
Complications include HF, risk of cerebral hemorrhage (berry aneurysms), aortic rupture, and possible endocarditis.
pt has a disease that is classicaly treated with:
metronidazole or oral vancomycin. For recurrent cases, consider repeating prior regimen, fidaxomicin, or fecal microbiota transplant.
caused by: an anaroebic, spore forming gram +ve bacteria
Diagnosed by detecting one or both toxins in stool by PCR.
Presents with: watery diarrhea most commonly
whats the etiology of this disease usually?
whats the disease?
what are the two toxins and their mechanism?
Toxin A, enterotoxin, binds to the brush border of the gut.
Toxin B, cytotoxin, causes cytoskeletal disruption
via actin depolymerization–> diarrhea–> pseudomembranous colitis!!!!!
due to antibiotics
any time a CoA is seen in a biochem rxn WHAT vitamin is also needed
Vitamin B5!!!! (pantothenic acid!)
eg: FA oxidation (FaCoA SYNTHASE and CPT (an acyl transferase) need it!!!
FA–> fatty acyl co A
A staccato cough is consistent with what..
with a viral or atypical pneumonia (eg: NEONATAL PNM CAUSED BY CHLAMIDYA —–here you also eosinophilia)
what two carcinogens can lead to ANGIOSARCOMA of liver
ARENSIC
VINYL CHLORIDE
Hirstuism + SECONDARY amenorrhea
PCOD
Thrombosis and (in pregnancy) fetal demise associated with various autoimmune antibodies directed against one or more phospholipid-binding proteins (eg, β2-glycoprotein I, prothrombin, annexin). These proteins normally bind to phospholipidmembrane constituents and protect them from excessive coagulation activation. The autoantibodies displace the protective proteins and, thus, produce procoagulant endothelial cell surfaces and cause arterial or venous thromboses.
whats the diag?
Antiphospholipid Antibody Syndrome
(Anti-Cardiolipin Antibodies; Lupus Anticoagulant)
in someone with COPD exacerbation, if you give HIGH flow O2 shortly after they become increasinly lethargic and confused, what is this due to?
ROS production
or
dead space ventilation
inc physiological dead space ventilation leading to v/q mismatch bc poorly ventilated areas are perfused!
see attached photo for the three reasons you get
OXYGEN INDUCED HYPERCAPNEA IN COPD!!!!
note: ROS prod would present differently like pleuritic chest pain, cough, dyspnea, WITHIN 24 HOURS OF BREATHING PURE 02

Most common ectopic thyroid tissue site is the (lingual thyroid) located where…
Thyroglossal duct cyst presents as mass where….
Most common ectopic thyroid tissue site is the tongue (lingual thyroid) @ base of tongue! note: Removal may result in hypothyroidism if it is the only thyroid tissue present.
Thyroglossal duct cyst: presents as an anterior midline neck mass that moves with swallowing or protrusion of the tongue
note: (vs persistent cervical sinus leading to branchial cleft cyst in lateral neck).
name the 6 main post translational modifications that consist of Covalent alterations
“m-a-p h-u-g”
methylation,
acetylation
Phosphorylation,
hydroxylation,
ubiquitination.
glycosylation,
bivalirudin
argatroban
dabigatran
are….
DIRECT THROMBIN INHIBITORS!
if you’re bleeding too much
Since theres no specifoc reversal agent. Can attempt to use activated prothrombin complex concentrates (PCC) and/or fibrinolytics (eg, tranexamic acid).
PBG deaminase def–>
Uropor Decarboxylase def—>
PBG Deaminase def–> Acute intermittent porphyria
note: this is the 2nd enzyme used in the CYtoplasm during heme syn (the first is ALAD)
Uropor Decarboxylase def—> Porphyria cutanea tarda
note: this is the 4th enzyme used in the CYtoplasm during heme synth
DOES THE REID INDEX FOR CHRONIC BRONCHIITS INCLUDE THE CARTILAGE LAYER?
NOOOO!!!
JUST THE PARTS BTW THE RESP EPITHELUM AND CARTILAGE
Fever + Absolute neutrophil count of__________is called Febrile Neutropenia and it puts pts at high risk of being infected with what 3 types of bug classes?
Absolute neutrophil count of <500mm
FUNGI and VIRUSES & bacteria (pseudomonas)
eg: Aspergillus Fumigatus–> Invasive Pulmonary Aspergilosis (pneumonia)
does neisseria meningitis grow on blood agar?
how is it transmitted?
NOOOOO
needs chocalate agar! in 5% CO2 atmosphere
RESPIRATORY DROPLETS
since both Riedel thyroiditis AND anaplastic carcinoma can extend to local structures (eg, trachea, esophagus)
HOW DO YOU TELL THE DIFF ON AN EXAM (ASIDE FROM HISTO BC Riedel thyroiditis IS HARD AS A ROCK BC ITS ALLLLL FIBROSED.
WHAT OTHER CLUE CAN YOU USE?
AGEEEEE!!!!!!!!!!
Riedel thyroiditis is young female!!!!
AND anaplastic carcinoma is ELDER!!!!!!!!!!!
dont you frickin fall for this trick on the test day.
timeline is the key diff btw PTSD and acute stress disorder
whats the diff
GREATER (>1month) for ptsd
3d-1 month and no longer! for brief psychotic disorder
Angiography revealed multiple or anomalous renal arteries going to each kidney are associated with what renal congenital defect?
horseshoe kidney!
due to the halted ascent, renal vascular anomalies are common: usually multiple renal arteries arise from the distal aorta or iliac arteries; this is important when these patients undergo any procedure, particularly a renal angiogram
not multiple ureters,
“AZUROPHILIC” + immature (blast cells) on blood smear SHOULD IMMEDIATELY MAKE YOU THINK OF WHAT
FREAKIN AML!!!!!!!!!!
AZUROPHILIC RODSSSSSSSSSSS PLUS IMMATURE CELLS HTEY ARE MPO +VE INCREASED NUMER OF MYELOBLASTS
Lithium and amiodarone both require what kind of test bf starting meds
TSH
what cell in the stomach is this?
parietal cells
light pink with blue nucleaus in the middle
looks like a fried egg
This slide shows several parietal cells. Parietal cells have a characteristic “fried-egg” appearance, with a basophilic, peripherally located nucleus and a rather eosinophilic cytoplasm. These cells secrete HCl and intrinsic factor. Under the electron microscope, the parietal cell appears pyramidal, with a central nucleus and many mitochondria. Why may mitochondria be so numerous in parietal cells?
Thyroid tissue is derived from….
Parafollicular cells (aka, C cells) of the thyroid are derived from…
Thyroid tissue is derived from endoderm.
Parafollicular cells (aka, C cells) of the thyroid are derived from neural crest.
derived from the 4th pouch
eg: medullary Ca of the thryroid is a
autosomal recessive, profound bilateral sensorineural deafness + LONG QT interval + congenital
what disease?
Jervell and Lange-Nielsen syndrome
45-year-old man with hypertension not compliant with medications. bp 160/100. Cardiac exam shows apical impulse displaced laterally, loud S2 and S4 gallop. Echo shows thickening of left ventricular wall. Mechanism of change in cardiac muscle? The levels of the following are inc or decreased?
Transcription factor c-Jun is…
beta-myosin heave chain is..
Endothelin is…
what even is endothelin? side q: what med inhibits endothelin and what is this med used to treat?
c-Jun is a protein that in humans is encoded by the JUN gene. c-Jun in combination with c-Fos, forms the AP-1 early response transcription factor.
NOTE! C-JUN and C-FOS are nuclear proto-oncogenes and are induced in patients with hypertrophic cardiomyopathy,
Overexpression of c-jun in cells results in decreased level of p53 and p21, and exhibits accelerated cell proliferation (hence the hypertrophic CM).
rugal hypertrophy (lots of mucus prod)
dec acid secretion
loss of protein (albumin)–> edema
stomach looks like brain gyri
Menetrier!!!!!
is smoking a RF for mesothelioma?
NOOOO!!!!!!!
but asbestos is!
QID 79 GREAT PATHOGENESIS OF ACUTE CALCULOUS CHOLECYSITIS
which worm worm infection gives you granulomas!
schistosoma!!!!!!!!
tx: DOC prazi
List 3 meds (antihypertensives) that increase Plasma Renin activity (specific names too)
ANTIHYPERTENSIVE MEDS
- Diuretics (HYDROCHLOROTHIZIDE)
- ACE inhibitors (Captopril, enalapril, lisinopril, ramipril )
- Antiotensin II receptor blockers (Valsartan. Losartan, candesartan,)
can a Tzank smear where epithelial cells are scraped from an ulcer base and stained which show the presence of multinucleated giant cells suggest Herpes be able to tell you whether the infection is
HSV vs Varicella Zoster?
NO!
therefore, PCR has largely replaced it.
how do you mainly diff btw lambert eaton and MG?
Proximal muscle weakness (cant go up stairs, get up from chair) that improves with use
Autonomic symptoms are huge and not seen in MG like:
DRY MOUTH
IMPOTENCE
also see HYPO or AREFLEXIA!!!!!!
whats the “wheel shaped virus and all its defining characteristics”
here is the nbme q on it
2-month-old female with T 102F, vomiting, diarrhea, dehydration. Exam of stool shows viral particles with wheel-like shape. Properties of virus?
Type of nucleic acid/envelop/capsid symmetry
- Double-stranded RNA (weird)
segmented
/no envelope-NAKED
/icosahedral bc +VE sense!
REO the weirdo causes ROTAvirus
(also causes Colorado tick fever)
all negative sense are HELICAL
which gram POSITIVE bug has an ENDOtoxin? not common.
are exo or endo toxins ACTIVELY secreted?
eXO toxins are actively secreted ENDO toxins are not
Listeria monocytogenes
listerolysin O
and it helps the organism evade phagocytosis
- New-onset hypertension with either proteinuria or end-organ dysfunction after 20th week of gestation (< 20 weeks suggests molar pregnancy).
- whats the pathogenesis of this condition?
- Incidence in patients with pre-existing
hypertension, diabetes, chronic renal disease,
autoimmune disorders.
- Complications: placental abruption, coagulopathy, renal failure, uteroplacental insufficiency, eclampsia.
Pre eclampsia
May proceed to eclampsia (pre-eclamp + maternal seizures) and/or HELLP syndrome.
Caused by abnormal placental spiral arteries
endothelial dysfunction, vasoconstriction &
ischemia.
Treatment: antihypertensives, IV magnesium sulfate (to prevent seizure); de nitive is delivery of fetus.
- lipohylainosis + microatheroma –> small vessel occulusion
- thalamic stroke (VENTRAL POSTERIOR THALAMUS) with PURE SENSORY LOSS
eg: DCML and ALS (anterolat/aka: spinothalamci) messed up
* history or uncontrolled HTN and DM
WHAT KIND OF INFARCT DO YOU NEED TO BE THINKING OF?
LACUNAR INFARCT they are result of small vessel occlusion due to lipohyalinosis and microatheroma in pentrating vessels of DEEP brain structures
Malignant mesenchymal proliferation of immature skeletal muscle; rare
Presents as bleeding and a grape-like mass protruding from the vagina or penis of a child (usually< 5 yrs of age); also known as sarcoma botryoides
Rhabdomyoblast, the characteristic cell, exhibits cytoplasmic cross-striations and
positive immunohistochemical staining is seen FOR….what two things
what disease is this?
positive immunohistochemical staining for desmin and myogenin.
rhabdomysosarcoma
DRY INSPIRATORY CRACKLES
COUGH
“PATCHY INTERSTITIALLLLLL INFILTRATION”
DYSPNEA
FEVER
are an AE of which of the following drugs?
- prednisone
- sotalol
- amiodarone
- levothyroxine
AMIODARONE!
i was describing characteristic features of inflamation and FIBROSIS in the pulmonary intersitium!
will present with
PROGRESSIVE DYSPNEA & DRY COUGH!
AMIODARONE CAUSES INTERSTITIAL PNEUMONITIS (pulmonary fibrosis!)!!!!!!!!
whats a very common cause of:
Neonatal hemorrhage with PT and aPTT but normal bleeding time
what is done to prevent this
whats the pathogenesis of this
Vit K deficiency
Vit K is Synthesized by intestinal flora.
(neonates have sterile intestines and are unable to synthesize vitamin K).
***Can also occur after prolonged use of broad-spectrum antibiotic
Newborns, as mentioned above, fit into this category, as their colons are frequently not adequately colonized in the first five to seven days of life
since Vit K is not in breast milk; neonates are given vitamin K injection at birth to prevent hemorrhagic disease of the newborn.
what bug does this:
Causes acute diarrhea or pseudoappendicitis (right lower abdominal pain due to mesenteric adenitis and/ or terminal ileitis).
Yersinia enterocolitica
Gram ⊝ rod. Usually transmitted from pet feces (eg, puppies), contaminated milk, or pork.
whats the diff btw ACUTE and CHRONIC mesenteric ischemia
Critical blockage of intestinal blood flow (often embolic occlusion of SMA) small bowel necrosis–> abdominal pain out of proportion to physical findings.
^^^[May see red “currant jelly” stools.]
“Intestinal angina”: atherosclerosis of celiac artery, SMA, or IMA–> intestinal hypoperfusion postprandial–> epigastric pain–> food aversion and weight loss.
whats the difference between the pathogenesis btw Albinism and Vitiligo?
match:
decreased TYROSINASE activity–> decreased MELANIN production (with NORMAL NUMBER OF MELANOCYTES)
autoimmune destruction of MELANOCYTES–> depigmentation (strongy associated with other autoimmune disorders such as: Graves, Autoimmune thyroiditis, Type 1 diab, pernicious anemia)
decreased Tyrosinase activity and decreased/absent MELANIN prod = ALBINISM
autoimmune destruction of MELANOCYTES= VITILIGO
ae of CCBs
both types
verap, dili! Non-dihydropyridine: cardiac depression, AV block, hyperprolactinemia, constipation.
the -dipines! Dihydropyridine: peripheral edema, ushing, dizziness, gingival hyperplasia.
MOA below

what is one pathogenic mechanism why gynecomastia is seen in cirrhosis?
decreased degradation of estrogen by the liver.
degrad/metabolism of estrogen to its metabolites bf being urinated out occurs in large part by the CYP450 enzymes in the lIVER
a baby has jejunal/ileal atresia.
how is the bowel affected? name 3 distinct features in order from most proximal bowel to most distal.
- the proximal jejunum ends in a BLIND POUCH
- followed by an are of absent bowel
- KEY: terminal ileum distal to atresia spirals (like an APPLE CORE OR XMAS TREE) around an ileocecel bloodvessel (aroudn a “ thin vascular stalk)
which ligament contains the Portal triad?
what are the contents of the portal triad?
Hepatoduodenal
Falciform
Gastrocolic
Gastrohepatic
Hepatoduodenal
Portal triad:
proper hepatic artery,
portal vein,
common bile duct
if a patient comes in (kid or adult) with mucosal bleeding, easy brusing & pettichiae
AND THEIR ONLY LAB ABNORMALITY IS A DECREASED PLATELET COUNT
-OF, for example, 9,000
(NORMAL: 150,000-400,00)
WHAT ARE YOU THINKING OF since they have an absolutely normal physical exam otherwise.
freakin ITP!!!!!
autoimmune platelet destruction by autoimmune platelet antibodies (IgG autoantibodies against plt membrane glycoprotein GPIIb/IIIa)
in kids (eg: after viral infection or immunization) its self limited, in adults (most common in woman of child bearing age (or with SLE): can cause short lived thrombocytopenia in offspring since IgG can cross the placenta) its an insidious chronic course
*can see INC megakaryocytes on BM biopsy.
what arthropathy is Hemochromatosis associated with?
affects knee alot
Calcium pyrophosphate deposition disease
Deposition of calcium pyrophosphate crystals within the joint space. Occurs in patients > 50 years old; both sexes affected equally. Usually idiopathic, sometimes associated with hemochromatosis, hyperparathyroidism, joint trauma.
Pain and swelling with acute in ammation (pseudogout) and/or chronic degeneration (pseudo- osteoarthritis). Knee most commonly affected joint.
Chondrocalcinosis (cartilage calci cation) on x-ray.
Crystals are rhomboid and weakly ⊕ birefringent under polarized light (blue when parallel to
light)
Anticentromere ab associated with
Limited scleroderma (CREST syndrome) shows AntiCentromere abs!
C for C!!!
what are the two cell surface markers INHIBIT T cells (and their response to tumors, for example).
list 2 and their ligands
antibodies against these CD markers are used to treat what type of cancer
CTLA-4 (CD152) on ACTIVATED T cells binds CD80/86 (B7) on its target (APC, tumor cells)
MOA: competes with CD28 on t cells for binding to B7 on APCs how we are used to seeing (which is normally stimulatory) and CTLA4 has a higher affinity for B7 so it wins—> no t cells–> no tumor apoptosis–> cancer.
AND
PD-1 on ACTIVATED T cells binds PD-1L on its target (APC, tumor cells)
NOTE:used to treat ADVANCED MELANOMA
A 25-year-old woman comes to the physician because of a 2-year history of intermittent, diffuse, cramping lower abdominal pain. The pain is usually associated with 2 to 6 days of loose, watery stools, and is typically relieved with defecation. Between these episodes, her stools are normal. Her vital signs are within normal limits. Physical examination shows no abnormalities. Laboratory studies, including complete blood count, metabolic panel, and thyroid function tests show no abnormalities. A drug targeting which of the following mechanisms of action is most appropriate for this patient?
a. inhibition of TNF-a
b. accentuation of bile salt reabsorption
c. Accentuates of μ-opioid myenteric plexus receptor
intermittent
relieved with defecation
is IBS
for IBS diarrhea you can give
-
LOPERAMIDE: Accentuates of μ-opioid myenteric plexus receptor–> dec Ach release and then DECREASE GI motility.
note: Cholestyramine (now spelt colestyramine) has been given for many years for diarrhoea in patients with ileal resection (bc they cant absorb bile acids) so you give a bile acid binding resin in this case
what two things does cytokine IL-4 do?
Hows about IL-5?
IL-4
- promotes T helper cel differentiatoin into the Th2 subset
- Stimulates B cell growth adn isotype switch to IgE
IL-5
- promotes growth and differentiation of b cells and eosinophils
- Stimulates isotype switching to IgA
Synovial fuid non-in ammatory (WBC < 2000/mm3).
Involves
DIP (Heberden nodes)
PIP (Bouchard nodes)
and 1st CMC
not MCP.
OA or RA?
OA
WHAT PULMONARY COMPLICATION IS ASSOCIATED WITH MARFANS?
SPONTANEOUS PNEUMOTHORAX FROM APICAL BLEBS
whats another way to say reverse transcriptase?
RNA dep DNA pol
*NOTE RETRO has a RNA dep DNA pol (reverse transcriptase)
Naked nucleic acids of ⊝ strand ssRNA and dsRNA viruses are not infectious. need RNA dep RNA Pol (note these are all NEGATIVE)
BUT
most dsDNA (except poxviruses and HBV) and
⊕ strand ssRNA ( which is same as ≈ mRNA) viruses are infectious.
diff btw febrile non hemolytic and acute hemolytic transfusion rx?
febrile non hemo is due to host abs against donor HLA ags and wbcs (just fever, chills, flushing and HA)
vs
hemolytic type is due to abo group incompatibility or host abs against foreign ags on donor RBCS (more severe)…HEMOGLOBINURIA (this is due to COMPLEMENT MEDIATED CELL LYSIS)
macrophages containing golder cytoplasmic granules that turn dark blue with prussian blue stain are describing WHAT
and WHAT is the pathogeneiss and most common cause of this finding in the LUNG
THIS IS CRUCIAL TO KNOW!!!!
freakin
hemosiderin laden macrophages
MOST FREAKIN COMMONLY CAUSED BY LEFT HEART FAILURE LEADING TO INC HYDROSTATIC P IN THE CAPS==> PULMONARY EDEMA.
THE RISE IN PRESSURE OF THE BLOOD INTO THE LUNGS INC CAPILLARY PERMEABILITY AND DISRUPTS THE CAPILLARY ENDOTHEIAL AND ALVEOLAR EPITHELIAL BLOOD GAS BARRIER!!!!
BLOOD LEAKS INTO ALVEOLI (EXTRAVASTION) AND THERE YOU HAVE IT ALVEOLAR HEMMORAGE!!!!
RBC ARE PHAGOCYTOSED BY MACS AND IRON FROM THE HB IS CONVERTED TO HEMOSIDERIN!!!!
what autosomal recessive disease resulting from an ABNORMAL POST TRANSLATIONAL PROCESSING OF A TRANSMEMBRANE PROTEIN (WHERE ITS MISFOLDED AND NOT GLYCOSYLATED AND SO THE ER DIRECTS IT TO A PROTEOSOME FOR DEGRADATION)
CF
talk about: Infections causing brain abscess (fill in the blank)
Most commonly _____and____
If dental infection or extraction precedes abscess, _______commonly involved.
- *Multiple abscesses** are usually from ____
- *Single lesions** from _______
—-otitis media and mastoiditis—>what lobe in brain___________
——sinusitis or dental infection—-> what lobe in brain________
Toxoplasma is most commonly seen in________
Most commonly viridans streptococci and Staphylococcus aureus.
If dental infection or extraction precedes abscess, oral anaerobes commonly involved.
Multiple abscesses are usually from bacteremia; Single lesions from contiguous sites:
—-otitis media and mastoiditis—> temporal lobe and cerebellum;
——sinusitis or dental infection—-> frontal lobe.
Toxoplasma reactivation in AIDS.
name that pneumoconiosis!
“Ivory white,” calcifed, supradiaphragmatic and pleural plaques. pathognomonic of ….
aerospace and manufacturing industries. Noncaseating granulomas on histology in the lung, hilar lymph nodes, and systemic organs and therefore occasionally responsive to steroids.
Sandblasting mines, “Eggshell” calcification of hilar lymph nodes + Macrophages respond to this particle and release broncogenic factors, leading to fibrosis… may disrupt phagolysosomes and impair macrophages, increasing susceptibility to TB!!!!!!!!!!!!!!!!!!!!
asymptomatic (not a pneumoconiosis) condition found in many urban dwellers exposed to sooty air.
Carbon dust; Massive exposure leads to diffuse fibrosis (‘black lung’)
name that pneumoconiosis!
“Ivory white,” calci ed, supradiaphragmatic and pleural plaques. pathognomonic of–> Asbestosis
aerospace and manufacturing industries. Noncaseating granulomas on histology in the lung, hilar lymph nodes, and systemic organs and therefore occasionally responsive to steroids. –> Berrylliosis
Sandblasting. mines“Eggshell” calcification of hilar lymph nodes + Macrophages respond to this particle and release bronchogenic factors, leading to fibrosis... may disrupt phagolysosomes and impair macrophages, increasing susceptibility to TB!!!!!!!!!!!!!!!!!!!! –> Silicosis
asymptomatic (not a pneumoconiosis) condition found in many urban dwellers exposed to sooty air.
–> Anthracosis
Carbon dust; Massive exposure leads to diffuse fibrosis (‘black lung’); –> Coal workers’ pneumoconiosis
Mycobacterium scrofulaceum (holy weird as name)
causes WHAT
(cervical lymphadenitis in children).
Adult male has Dry Tap on BM aspiration and MASSIVE splenomegaly.
Tartrate resistnace acid phosphatase +ve
what is the diagnosis
WHAT ARE THE TWO treatments and their MOA
Hairy cell leukemia
CLADRIBINE (antimetabolite)
PURINE analogue
inhibits DNA pol and causes DNA strand breaks
note: the other purine analogue (inhibits DE NOVO purine synthesis is 6MP)
what parts of the branchial arch is derived from mesoderm, what part if derived from neural crest?
Branchial arches—
derived from mesoderm (muscles, arteries)
neural crest (bones, cartilage).
hep b and c are endemic in Sub saharan africa. T or F?
TRUE
bladder exstrophy is due to what
and what two clincal associations can you make with it?
Ventral wall defects (tummy side) Developmental defects due to failure of: CAUDAL fold closure—bladder exstrophy
Exstrophy of the bladder is associated with
- Epispadias
- Adenocarcinoma of the bladder
note:
Developmental defects due to failure of:
Rostral fold closure—sternal defects
Lateral fold closure—omphalocele & gastroschisis
Up to 25% of PHEOCHROMOCYTOMA cases are associated with germline mutations, name 3 main ones
Up to 25% of cases associated with germline mutations (eg,
NF-1,
VHL,
RET [MEN 2A, 2B]).
if an HIV pt has a cd count less than 50.
he is at risk for getting MAC (mycobacat avium complex).
what can you give AS PROPHYLAXIS FOR MAC
isoniazid
or
azithromycin
dont fall for it!
ISONIAZID DOES NOT WORK AGAINST MAC!!!!!!
JUST AZITHRO OR CLARTHRO (MACROLIDES)
For acute cough, the most common cause is
name 1
For chronic cough, the most common causes are
name 3
For acute cough, the most common cause is
• Viral URI
For chronic cough, the most common causes are
- Asthma (most common)
- Gastroesophageal reflux disorder (GERD)
- Postnasal drip
AN umbilical hernia (seen at birth) which is reducible adn comes out when crying and also is asymptomatic and resolves spontaneously by around age 3 is classically associated with what disorders and what is the pathogenesis of this disorder.
- down syndrome
- hypothroidism (cretinism)
- Beckwith Wiedman syndrome
Copper is a cofactor for what 3 things
Cofactor for
- ferroxidase (binds iron to transferrin),
- lysyl oxidase (cross-linking of
collagen and elastic tissue),
- tyrosinase (melanin synthesis)
Diapedesis—WBC travels between endothelial cells and exits blood vessel
whats on wbc vs endothelium?
PECAM-1 (CD31) on both
diff btw gen anxiety disorder and adjustment disorder?
GAD last >6 mos and is NOT brought on by a specifc event, person, place or thing
adjustment disorder is <6 months (>6 months is the INCITING STRESSOR is chronic)
so here we have an actual stessor causing impairment (divorce, illness, etc)
WHAT LINES A PSEUDOCYST?
EPITHELIUM
OR
GRANULATION TISSUE + FIBROSIS?
…….YOU BEST GET THIS RIGHT.
GRANULATION AND FIBROUS TISSUE THATS WHY IS A PSEUDO AND NOT REAL CYST
if i say rhomboid crystals that are weakly birefringment under polarized light (blue when parallel to light), what disease process do you think of?
what is seen on xray in patients with this?
Calcium pyrophosphate deposition disease
[PSEUDOGOUT]
X RAY: chondrocalcinosis (cartilage calcificaitons)
*knee is most affected
what the most common COMPLICATION OF CAUSTIC INGESTION?
STRICTURE (ESOPHAGEAL)–> SQUAMOUS CELL CA
DOC for invasive mucomycosis
amphotericin B
what type of drug toxicity is being described:
can be due to any cause of decreased GFR, overdose or drug interaction
acutely presents with GI sxs
Chronically presents with Neuro sxs like ataxia, tremors/fasciculations
its MOA is to inhibit the Phophoinositol cascase
Lithium
treatment for ACROMEGALY
- Pituitary adenoma resection. If not cured, treat with
- Octreotide (somatostatin analog)
- Pegvisomant (growth hormone receptor antagonist).
chiari 1 vs 2
KNOW THIS!
due to underdevelopment of Posteror fossa
chiari 1: more mild (relatively benign) presents at adolescence, due to cerebellar tonsils that extend beyond foramen magnum into the vertral canal: present like Paroxsymal occipital HA (due to meningeal irritation) and cerebella dys (ataxia and dizziness) due to compression of cerebella tonsils
—associated with SYRINGOMYELIA!
chiari 2: more severe, presents in neonate (tonsils, vermis and medulla even through FM)
-NON COMM hydrocep always happens bc of aqueductal stenosis (compression of medulla–> dysphagia, apnea, and stridor + lumar Associated with: Myelomeningoclee! –> lower limb paralysis
what are 3 main examples of Free radical injury and examples for each category
- Oxygen toxicity: retinopathy of prematurity (abnormal vascularization) & bronchopulmonary
dysplasia (from Therapeutic supplemental O2 to a baby who has ARDS when its done too quickly!)
2. Drug/chemical toxicity: carbon tetrachloride–> causes FATTY change in liver by decreasing protein synthesis (inlcuding apoliopproteins–>causes fat to be able to come into liver but cant get out) & acetaminophen overdose (hepatotoxicity)
- Metal storage diseases: hemochromatosis (iron) and Wilson disease (copper)
List all the CYP450 INHIBITORS
CRACK IM A GQ’SS
Cimetidine
Ritonavir
Amiodarone
ciprofloxacin
Ketoconazole
Isoniazid (INH)
Macrolides (except azithromycin)
Acute Alcohol Abuse
Grapefruit juice
Quinidine
SulfonamideS
SSRI’s
Be careful with
-cyclosporin (narrow therapeutic index, extenseively met in liver and intestine by CYP3A4)
spott necrosis + ballooning degeneration (hepatocyte swelling) + eosinophilic apoptotic bodies in the liver biopsy of a man who recently traveled to s america is the histo you would see in WHAT viral illness?
and how would this man classically present one week into the disease?
HEP A!!!!!!!!!
NOTE! the eosinophiic apop bodies are COUNCILMAN BODOIES!!!!!!!!!
first is a prodrome: fever, ANOREXIA, N/V, malaise
THEN
CHOLESTATIC signs: jaundice, DARK COLORED URINE, LIGHT STOOL, pruitis
no carrier state and self limited
KNOW THAT HISTO
how do bugs confer resistance to MACROLIDES?
well since macrolides work by BINDING TO THE 23S SUBUNIT OF THE 50 S ribosome and blocking translocation
if you METHYLATE that 23S rRNA binding site the DRUG CANT BIND AND VOILA!
2 causes of Protein-Energy Malnutrition (PEM? PRIMARY
and whats the MCC of secondary
- kwashikor
- marasmus
seconday
a. Secondary PEM is common in the elderly (living alone or in hospitals or nursing homes), chronic alcoholics, the homeless population, and bedridden
patients.
WHAT IS HOMAN SIGN
WHERE IS IT CHARACTERISICALLY SEEN?
Homan sign—WHEN DORSIFLEXTIONof foot calf CAUSES PAIN!
DVT!!!!!!!! (inc d-dimer)
THESE LABS ARE SEEN WHERE
- INC PTH, INC ALP, INC cAMP in urine.
- Most often asymptomatic.
- May present with weakness and constipation, abdominal/ flank pain (kidney stones, acute pancreatitis), depression
Primary hyperparathyroidism
profound bilateral sensorineural hearing loss in child who experiences syncopal episodes during periods of stress, exercise, or fright.
and long QTc, usually greater than 500 msec.
diagnosis
which disease presents the same but is AD and no deafess?
Congenital long QT syndrome
Jervell and Lange-Nielsen syndrome— autosomal recessive, sensorineural deafness. (AR)
Romano-Ward syndrome—autosomal dominant, pure cardiac phenotype (no deafness).
what effect does restrictive cardiomyopathy have on
LV End DIASTOLIC pressure?
how does it affect the PV loops?
LV EDP increases at the SAME LV EDV
moves up and to the left
HOW TO DO DIFF BTW APCKD AND MCKD (multicysitic dysplastic kidney)?
ADCDK follows a clear inheritance pattern.
mcdk is congenital and SPONTANEOUS NOT INHERITED
adckd have cysts but their renal system is developed just fine
mcdk had an issue of the ureteric bud not taking to the metanenpheric mesenchyme so the kidney (ureter, tubules, etc) DO NOT develop propersly AND THIS CAUSES BUILD UP OF URINE AND SUBSEQUENT cysts that dont communicate and fibrosis with lots of cartilage
what two opioid analgesic are given for diarrhea as well
whats the MOA
what drug is given alongside to discourage pts from taking high doses to acheive euphoria or dependence?
loperamide
diphenoxylate
they bind mu opiod receptors in the GI and SLOW MOTILITY
give atropine (causes dry mouth, blurry vision, nausea) so pts wont want to take the opiods in high doses or else they’ll get these ae’s
WBC travels through interstitium to site of injury or infection guided by chemotactic signals
what are thees chemotactic signals on the endothelium? (5)
K-C L I P
kallikrein
LTB4
IL-8
C5a
Platelet-activating factor
wickham striate (reticular white lines) in mouth mucosa associated with…
lichun planus!!
what subunits make up fetal vs adult hemoglobin
Fetal Hb (2α and 2γ subunits)
Adult is 2a, 2b
In the type of pulmonary HTN caused by Vasoconstriction, is vasoconstriction is thought to be due in part to enhanced activity of name two classic vasoconstrictors and reduced activity of name two classic vasodilators..
is there a treatment for this? name 3 if ya can and their MOA!
Vasoconstriction is thought to be due in part to
- enhanced activity of thromboxane and endothelin-1 (both vasoconstrictors)
and
- reduced activity of prostacyclin and nitric oxide (both vasodilators).
- BosENtan: Competitively antagonizes ENdothelin-1 receptors–> DEC. pulmonary vascular resistance.
- Sildenafil: Inhibits cGMP PDE-5 and prolongs vasodilatory effect of nitric oxide.
- Epoprostenol, iloprost: PGI2 (prostacyclin) with direct vasodilatory effects on pulmonary and systemic arterial vascular beds. Inhibits platelet aggregation.
The increased pulmonary vascular pressure that results from vascular obstruction further injures the endothelium. Injury activates coagulation at the intimal surface, which may worsen the hypertension.
what valve is most commonly affected in Rheumatic Heart Disease (Rheumatic Fever)
Mitral
Mitral>Aortic>>>>tricuspid (high-pressure valves affected most).
which Pneumoconioses is the only one that affects LOWER lobes
Asbestosis
whats the only bug to have protein A as its virulence factor?
staph aureus!
prevents opson and phago
binds the fc part of IgG
WHAT ARE THE BORDERS OF THE FEMORAL TRIANGLE?
when the femoral vein runs superior and passes the inguinal ligament, what vein does it officially become?
Inguinal lig (superior)
Adductor longus (medially)
Sartorius muscle (laterally)
EXTERNAL ILIAC VEIN

Diagnosis is primarily of Guillain-Barré syndrome. clinical.
Similar acute weakness can result from
myasthenia gravis, botulism, poliomyelitis (mainly outside the US), tick paralysis, West Nile virus infection, and metabolic neuropathies
HOW can these usually be distinguished?
- Myasthenia gravis is intermittent and worsened by exertion.
- Botulism may cause fixed dilated pupils (in 50%) and prominent cranial nerve dysfunction with normal sensation.
- Poliomyelitis usually occurs in epidemics.
- Tick paralysis causes ascending paralysis but spares sensation.
- West Nile virus causes headache, fever, and asymmetric flaccid paralysis but spares sensation.
- Metabolic neuropathies occur with a chronic metabolic disorder.
whats the substrate that inhibits CPT-1 in carnitine shuttel during FA degrad and what is the use of this type of reg?
Malonyl CoA inhibits CPT-I, thus preventing the entry of long-chain acyl groups into the mitochondrial matrix.
Therefore, when fatty acid synthesis is occurring in the cytosol (as indicated by the presence of malonyl CoA), the newly made palmitate cannot be transferred into the mitochondria and degraded.
so that FA synthesis and degrad are not happening at the same time?
does Sirolimus (Rapamycin) work by
- Preventing IL-2 transcription (production) or
- Preventing response to IL-2.
whats its main MOA
in contrast to cyclosporine and tacrolimus how does siroliums differ?
what its main AE?
its an: mTOR inhibitor; binds FKBP.
Blocks T-cell activation and B-cell differentiation by preventing response to IL-2.
calcineurin: Calcineurin inhibitor; binds cyclophilin. –Blocks T-cell activation by preventing IL-2 transcription.
tacrolimus: Calcineurin inhibitor; binds FK506 binding protein (FKBP).
Blocks T-cell activation by preventing IL-2 transcription.
both tacrolimus and calcineurin are NEPHROtox but SIROLIMUS is NOT NEPHROTOXIC! its causes pancytopenia, insulin resistance & hyperlipidemia;
******Kidney “sir-vives.” Synergistic with
cyclosporine.
which one of the following require a SEGMENTED GENOME (as they relate to Viruses). Give an example fo a virus that would take place in this.
recombination
reassortment
phenotypic mixing
complementation
REASSORTMENT
requires a VIRUS WITH A SEGMENTED GENOME
S for S
eg: influenza
a LOW maternal AFP is characterisically seen in
DOWN SYNDROME
linelozind,
whats a bad AE
serotoninc syndrome!!!
Adenomas (Conn) caused by an adenoma, usually unilateral, of the glomerulosa cells of the adrenal cortex or, more rarely,
by adrenal hyperplasia.
In adrenal hyperplasia, which is more common among older men, both adrenals are overactive, and no adenoma is present.
Hypernatremia, hypervolemia, and a hypokalemic alkalosis may occur, causing episodic weakness, paresthesias, transient paralysis, and tetany. Diastolic hypertension and hypokalemic nephropathy with polyuria and polydipsia are common
note: Low levels of both PRA (Plasma renin activity () and aldosterone suggest nonaldosterone mineralocorticoid excess (eg, due to licorice ingestion, Cushing’s syndrome, or Liddle syndrome).
HVA and VMA (catecholamine metabolites) in urine!
Bombesin and NSE ⊕.
Associated with overexpression of N-myc oncogene.
Classidfied as an APUD tumor (amine precursor uptake decarboxylase (APUD)
associated with a characteristic Pareneoplastic syndrome that is seen also seen in adults (when adults have Smal cell CA)
diagnosis?
Neuroblastoma
- Most common tumor of the adrenal medulla in children, usually < 4 years old.
- Originates from neural crest cells. Occurs anywhere along the sympathetic chain
Can also present with opsoclonus-myoclonus syndrome (“dancing eyes-dancing feet”).
NOTE: you can say the “adult” version of this is tumor is Pheochromocytoma which is MORE likely to present with HTN than this neuroblastoma

how heat stable are ENDOtoxins
stable at 100 deg for 1 hour
match the histo description with the type of Hep virus (choose from HEP A, B or C
- Granular eosinophilic “ground glass” appearance; [cytotoxic T cells mediate damage]
- Lymphoid aggregates with focal areas of macrovesicular steatosis
- Hepatocyte swelling, monocyte infiltration, Councilman bodies (refer to attached image for description of a councilman body)
- Granular eosinophilic “ground glass” appearance; [cytotoxic T cells mediate damage] = HEP B
- Lymphoid aggregates with focal areas of macrovesicular steatosis = HEP C
- Hepatocyte swelling, monocyte infiltration, Councilman bodies = HEP A

which of the following cytokines are critical for the formation and maintenance of granulomas (eg: in TB). Pick alll that apply
a. IL-4
b. IL-2
c. IL-12
d. IFN gamma
e. IL-6
f. TNF-a
qID: 301
c. IL-12 (induces t helper cells differentialtion into the Th1 subtype)
d. IFN gamma (produced by mature Th1 cells which then activate macs, improving their abiity to kill ingested mycobacteria.
f. TNF-a (produced by activated macs to recruit additonal monocytes and macs to the area)
macrophage mediated immunity to Mycobacterium Tb is led by Th1 helper cells (you go down this pathway when IFN-gamma > IL-4)
which is the childhood tumor that is Derived from remnants of Rathke pouch?
where in the brain is it located? supra or infratentorial?
how does it present
whats commonly seen of it on imaging
-Most common childhood supratentorial tumor.
- Derived from remnants of Rathke pouch.
- *-Calcification** is common on imaging
-May be confused with pituitary adenoma (both can cause bitemporal hemianopia)
increased wall stress on right--> HEMATOCHEZIA=associated with what GI pathology?
increased wall stress on left–> HEMATOCHEZIA=associated with what GI pathology?
increased wall stress on right--> HEMATOCHEZIA=associated with ANGIODYSPLASIA (Most often found in cecum, terminal ileum, ascending colon)
increased wall stress on left–> PAINLESS HEMATOCHEZIA=DIVERTICULOSIS
[Many false diverticula of the colon, commonly sigmoid. Caused by intraluminal pressure and focal weakness in colonic wall. Associated with low- FIber diets.
POMC is enzymatically cleaved to produce what 3 things?
b-endorphins (delta receptor)
ACTH
MSH
[HERITABLE] Pulmonary arterial hypertension is caused by:
an inactivating mutation in BMPR2 gene (normally inhibits vascular smooth muscle proliferation); poor prognosis.
note:
Other causes include drugs (eg, amphetamines, cocaine), connective tissue disease, HIV infection,
portal hypertension, congenital heart disease, schistosomiasis.
why is OSMOTIC DIARRHEA + A DECREASED STOOL pH seen in LACTOSE INTOLERANCE?
OSMOTIC DIARRHEA bc lactose attracts water into the small bowel
A DECREASED STOOL pH bc BACTERIA in the gut FERMENT THE LACTOSE INTO LACTIC ACID!
NOTE: Lactose hydrogen breath test: ⊕ for lactose malabsorption if postlactose breath hydrogen value rises > 20 ppm compared with baseline.
Aortic narrowing near insertion of ductus arteriosus (“juxtaductal”).
Associated with bicuspid aortic valve, other heart defects, and Turner syndrome.
Hypertension in upper extremities and weak, delayed pulse in lower extremities (brachial-femoral delay).
name that congenital heart defect
Coarctation of the aorta
whats the difference btw WET and DRY beri beri (for fun, deficiency in what vitamin causes this)?
Dry beriberi—polyneuritis, symmetrical muscle wasting.
Wet beriberi—high-output cardiac failure (dilated cardiomyopathy), edema.
what type of behavior is HTLV associatd with?
(associated with IV drug abuse)
Adults present with cutaneous lesions;
especially affects populations in Japan, West Africa, and the Caribbean.
Lytic bone lesions, hypercalcemia.
i got this wrong
note the
broad based budders (which i didnt initially see and note NEUTROPENIA)
thing fungal

answer is AMPHOTERICIN
general funal treatment:
Treatment:
Fluuconazole or itraconazole for local infection;
amphotericin B for systemic infection.
H-B-C-P are the SYSTEMIC MYCOSIS
side note: Systemic mycoses can form granulomas (like TB) but cannot be transmitted person-to-person (unlike TB).

the upper part of the vagina developes from the _________
while the lower part develops from the _________
- Paramesonephric (MULLERIAN) duct
- urogenital sinus
what is the GHRH analog used to treat HIV associated lipodystrophy?
tesamorelin!
cyst brain lesion + immunoCOMPETENT patient + native to Central/South america + seizures/ intracranial HTN you should be suspicious of what and treat how?
neurocysticercosis
treat with albendazole
“periventricular calcifications” are seen in a baby with
unique
a CONGENITAL CMV infection!
(transmitted to mom via sexual contact or TRANSPLANT)
Hearing loss, seizures, petechial rash, “blueberry muffin” rash, periventricular calci cations
not periventricular plaques assoc with MS
what is the most common predisposing condition for native valive IE (infective endocarditis) IN DEVELOPED NATIONS? how about in DEVELOPING nations?
MITRAL VALVE PROLAPSE WITH REGURGITATION (deposits on valves can become colonized by microorganism (eg: strep viridans) during episodes or bacteremia (eg: following a dental extraction).
NOTE: IE–> embolic stoke (middle cerebral artery)— (common complication)
RHEUMATIC HEART DISEASE (under developed nations)
72-year-old woman comes to the physician because of a 6-month history of increased bruising on her forearms. She appears alert and well nourished. Physical examination shows extensive wrinkling, scaly erythematous patches on the face, and irregularly shaped brown macules on the face and forearms. There are ecchymoses in various stages of healing on both forearms; the ecchymoses are more numerous on the right side. Laboratory studies, including a complete blood count and coagulation studies, are within the reference ranges. She has noticed no bleeding from her gums after brushing her teeth. Which of the following is the most likely cause of the ecchymoses in this patient?
A. Exocytosis of lymphocytes
B. Extensive solar elastosis
C. Impaired platelet function
D. UV destruction by Langerhans in epidermis
B. Extensive solar elastosis
Histo feature seen in Actinic keratosis!
Premalignant lesions caused by sun exposure. Small, rough, erythematous or brownish papules or plaques . Risk of squamous cell carcinoma is proportional to degree of epithelial dysplasia.
Richter transformation is—(when the type of cancer whose name you are trying to guess) undergoes transformation into an aggressive lymphoma, most commonly diffuse large B-cell lymphoma (DLBCL).
Chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL)
what factors cause a shift of the Oxygen-hemoglobin dissociation curve of the curve to the right?
does a right shift mean that unloading o2 is favored or not?
“Right shift—When curve shifts to the right, DECREASED affinity of Hb for O2 (facilitates unloading of O2 to tissue).
ACE BATs right handed”
Acid
CO2
Exercise
2,3-BPG
Altitude
Temperature
82-year-old woman comes to the physician because of constant severe lower abdominal pain and fever for 24 hours. Laproscopic examination shows severe diverticulosis and perforated diverticulitis. In spite of appropriate therapy she dies 2 days later. Liver autopsy shown. Which of the following is the primary component of the material shown on the hepatic surface?

FIBRIN!!!!!
what vitamin deficiency is being described
Hemolytic anemia
acanthocytosis
muscle weakness
posterior column and spinocerebellar tract demyelination.
Vitamin E DEFICIENCY
DONT BE FOOLED.
THIS IS SIMILAR TO VIA B12 DEFICIENCY BUT IS DIFFERENT BC HERE WE ARE LACKING:
megaloblastic anemia
hypersegmented neutrophils
INC serum methylmalonic acid levels.
DRUGS THAT CAUSE:
[DILE] Drug induced lupus Erythematosus (SLE-like syndrome)
“SHIPP-E”
Sulfa drugs,
**Hydralazine,
**Isoniazid,
**Procainamide (class 1A antiarrythmic) (note: Procainamide is metabolize by hepatic ACETYLATION: therefore, SLOW acetylators are at higher risk of DILE
Phenytoin,
Etanercept
SHIPP-E
what are the lab presentations in primary (psychogenic) polydipsia
Psychogenic polydipsia is found in patients with mental illnesses, most commonly schizophrenia
The most common presenting symptom is tonic-clonic seizure, found in 80% of patients.
HYPOnatremia bc they be drinking so much water (UNLIKE central or nephro DI where they have HYPERnatremia!!!)
INITIAL low urine OSMOlarity (but then quickly responds to water depriv and urine inc in osmolarity).
also, urine will not change in osm after ADH is given bc max endogenous ADH has already been used
The most common presenting symptom is tonic-clonic seizure, found in 80% of patients.[21] Psychogenic polydipsia should be considered a life-threatening condition, since it has been known to cause severe hyponatraemia, leading to cardiac arrest, coma and cerebral oedema.
Euvolemic hyponatremia: In euvolemic (dilutional) hyponatremia, total body Na and thus ECF volume are normal or near-normal; however, TBW is increased.
Primary polydipsia can cause hyponatremia only when water intake overwhelms the kidneys’ ability to excrete water. Because normal kidneys can excrete up to 25 L urine/day, hyponatremia due solely to polydipsia results only from the ingestion of large amounts of water or from defects in renal capacity to excrete free water. Patients affected include those with psychosis or more modest degrees of polydipsia plus renal insufficiency.
Patients with acute psychogenic water drinking are able to concentrate their urine during water deprivation. However, because chronic water intake diminishes medullary tonicity in the kidney, patients with longstanding polydipsia are not able to concentrate their urine to maximal levels during water deprivation, a response similar to that of patients with partial CDI. However, unlike CDI, patients with psychogenic polydipsia show no response to exogenous ADH after water deprivation. This response resembles NDI, except that basal ADH levels are low compared with the elevated levels present in NDI. After prolonged restriction of fluid intake to ≤ 2 L/day, normal concentrating ability returns within several weeks.
EUVOLEMIC (normal volume, normal BP) HYPONATREMIA is classically seen in….
SIADH!!!!
Characterized by:
- Excessive free water retention
- Euvolemic hyponatremia with continued urinary Na+ excretion which is protective to keep BP and vLs in check via the following mechanisms:
***Body responds to water retention with aldosterone and ANP and BNP—> INC urinary Na+ secretion–> normalization of extracellular uid volume—> euvolemic hyponatremia.
what disease is this
HONEYCOMB LUNG
CYCLICAL LUNG INJURY: repeated cyles of lung injury and wound healing (diffuse fibrosis) increased collagen deposition
-digital clubbing
IDIOPATHIC PULMONARY FIBROSIS (IPF)
aka: Cryptogenic fibrosing alveolitis
a type of restrictive lung disease affecting the interstitium
what two ethnicitis are at inc risk for pancreatic adenomcarcinoma?
jews
african americas
VACTERL association specifically refers to the abnormalities in structures derived from what embryonic entity?
what does vacterl stand for?
MESODERM!
- *V**ertebral defects
- *A**nal atresia
- *C**ardiac defects
Tracheo-Esophageal stula
Renal defects
Limb defects (bone and muscle)
RECURRENT C DIFF INFECTIONS
whats the DOC
whats its MOA?
is it safe in pts allergic to penicillin?
FIDAXOMICIN!!!!!!!!!!!!
its inhibits the sigma subunit of RNA POL!!!!!
its a macrocylic antibiotic
SAFE!!!!
what are the two complications of Vit EXCESS?
- in pts at high risk for iron overload, VIT C can cause IRON OVERLOAD (bc its job is to convert fe 3+ to fe 2+ (which can then be absorped in intestine)
- can cause ca2+ oxalate stones bc (vit C–> metabolized into Oxalate!
in this disease, Aplastic anemia, which is Caused by failure or destruction of myeloid stem cells, is due to:
(DNA repair defect causing bone marrow failure); also short stature, incidence of tumors/leukemia, café-au-lait spots, thumb/radial defects.
what disease is this? that is causing this aplastic anemia?
whats the other main disease caused by defective DNA repair
cannot repair dna via Nonhomologous end joining which rings together 2 ends of DNA fragments to repair double-stranded breaks. No requirement for homology. Some DNA may be lost
Nonhemolytic, normocytic anemia
Fanconi anemia
ataxia telangiectasia is the other one!
during Tight-binding—whats on wbc vs endothelium?
is there a deficiency associated here?
ICAM-1 (CD54)- on endothelium
CD11/18 integrins (LFA-1, Mac-1) on WBC
(defective in leukocyte adhesion deficiency type 1 (CD18 integrin subunit)
CD5+ve
associated with Coombs +ve hemolytic
indolent
Chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL)
SMUDGE CELLS!!!!!!
- “brown tumor” consisting of osteoclasts and deposited hemosiderin from hemorrhages; causes bone pain)
where is this seen?
DUE TO PRIMARY HYPERPARATHYROIDISM
Osteitis brosa cystica—cystic bone spaces lled with brown brous tissue (“brown tumor” consisting of osteoclasts and deposited hemosiderin from hemorrhages; causes bone pain).
the most common acquired inflammatory neuropathy.
autoimmune attack of peripheral myelin (“PRIMARY AFFERENTS”) due to molecular mimicry, inoculations, and stress, but no definitive link to pathogens.
Flaccid weakness predominates in most patients; it is always more prominent than sensory abnormalities
WHATS THE DIAGNOSIS? WHAT WOULD BE TYPICALLLLY SEEN ON LABS?
HERES THE NBME Q ON THIS
24-year-old man with 3-day progressive numbness of both feet ascended to thighs. Last 24 hours, numbness and tingling of hands. PE ataxic gait. Deep tendon reflexes diminished in upper extremities and absent in knees and ankles. Vibration and joint position absent in fingertips and feet bilaterally. Mild weakness distal upper extremities ad moderate weakness of lower extremities. Structure involved?=MYELINATED PRIMARY AFFERENTS
Guillain-Barré syndrome. [an Acute in ammatory demyelinating polyradiculopathy)
Associated with infections (eg, Campylobacter jejuni, viral)—> autoimmune attack of peripheral myelin
Findings: CSF protein with normal cell count (albuminocytologic dissociation).
Complication of the labs findings: protein may cause papilledema.
- 5-HT3 antagonist; DECREASES vagal stimulation. Powerful central-acting antiemetic.
- whats this drug? and what KIND of nausea does it treat?
- main SERIOUS AE?
VERSUS:
- D2 receptor antagonist. resting tone, contractility, LES tone, motility.
- WHATS THE NAME OF THIS DRUG
- WHAT ARE ITS USES?
- WHEN IS IT CONTRAINDICATED?
Ondansetron!!!
- Control vomiting postoperatively and in patients undergoing cancer chemotherapy.
- AE: Long QT interval WHICH predisposes to torsades de pointes.
Metoclopramide!!!
- Diabetic and postsurgery gastroparesis,
- Antiemetic
- AEL Parkinsonian effects, tardive dyskinesia. Restlessness, drowsiness, fatigue, depression, diarrhea.
- Drug interaction with digoxin and diabetic agents.
- Contraindicated in patients with small bowel obstruction or Parkinson disease (due to D2-receptor blockade).
whats the pathogenesis behind the levels of CK as they relate to the “MYOPATHY” seen in Hyper and Hypothyroidism?
when are CK levels inc and when are they normal and why?
- Hypothyroid myopathy (proximal muscle weakness, INCREASED CK)
- *this is bc DEC THYROID HORMONE INC THE PERMEABILITY OF SKELETAL MUSCLE MEMBRANES SO CK LEAKS INTO BLOOD AND IS MEASURED AS INC IN SERUM.
VS.
- Thyrotoxic (hyperthyroidism) myopathy (proximal muscle weakness, normal CK)
- you get the myopathy bc of INC PROTEIN CATABOLISM (but no inc in CK bc the membranes of the skeletal muscle are ok).
Results in inappropriate laughter (“happy puppet”), seizures, ataxia, and severe intellectual disability.
Diagnosis?
Paternal or maternal imprinting?
gene from dad or mom is normally silent?
Paternal or Maternal gene is deleted/mutated?
AngelMan syndrome
Paternal Imprinting
gene from dad is normally silent and
Maternal gene is deleted/mutated.
FINDINGS in this diseaes:
- HF
- S3
- systolic regurgitant murmur
dilated heart on echocardiogram,
balloon appearance of heart on CXR.
what am i describing?
what are the 9 main etiologies? ABCCCD-PSH
Dilated cardiomyopathy
Alcohol abuse, wet Beriberi, Coxsackie B viral myocarditis, chronic Cocaine use, Chagas disease, Doxorubicin toxicity, peripartum cardiomyopathy. sarcoidosis, hemochromatosis,
*Systolic dysfunction ensues.
*Eccentric hypertrophy
old lady comes in bc of muscle weakness and tenderness on her shins.
she has LOW ca2+ and HIGH PTH
what does she have?
osteoporosis
osteomalacia
metastatic breast cancer
primary hyperparathyroidsm
NOT OSTEOPOROSIS,
labs are NORMAL in osteoporosis
OSTEOMALACIA!!!!!!!!!
which hematologic cancer shows
REAL REAL LOW LAP
and commonly accelerates and transforms to “blast crisis”
and can be treated with imatinib
Chronic myelogenous leukemia!!!!!!!
NOTE: Very low LAP as a result of low activity in malignant neutrophils (vs benign neutrophilia [leukemoid reaction], in which LAP is INC ).
Responds to bcr-abl tyrosine kinase inhibitors (eg, imatinib).
why would loss of Ca2+ in the ECM lead to loss of cell-cell adhesion?
bc Cadherins which bind to cadherins on neighboring epithelial cells are CALCIUM dependent.
which TCA is DOC for OCD
clomipramine
diff btw dry and wet beri beri
seen in malnourished areas
dri: muscle and neuro + NO EDEMA
wet: tachy and high output cardiac failure (dilated CM) + WITH EDEMA
whats the #1 RF for transitional cell CA?
but then what are the other RFs?
SMOKING!!!! #1
Pee SAC:
Phenacetin,
Smoking,
Aniline dyes
Cyclophosphamide.
“germ tubes”
what are they and what bug are they associated with and at what temperature?
Germ tubes: short outgrowth, non-septate germinating TRUE hyphae. They are ½ the width and 3 – 4 times the length of the cell from which they arise. When cells of Candida are incubated in serum at 37C for 2-4 hours Candida albicans produce short, slender, tube like structures called germ tubes
Note: A germ tube test is a diagnostic test in which a sample of fungal spores are suspended in animal serum and examined by microscopy for the detection of any germ tubes.[2] It is particularly indicated for colonies of white or cream color on fungal culture, where a positive germ tube test is strongly indicative of Candida albicans.[2]

whats the most abundant aa in collagen?
lysince
proline
glycine
GLYCINE!!
dont you dare say proline
what two cancers are pts with ataxia telangiectasia at risk for?
whats the pathogenesis of this disease?
what is CHARACTERISTICALLY ELEVATED IN THE SERUM AND WHAT IS CHARACTERISTICALLY DECREASED?
primary cns lymphoma
leucemia
ATM gene is mutated and leads to INACTIVATION OF tp53–> which leads to failure to repeair DNA double stranded breaks—>CELL CYCLE ARREST
INCREASED AFP!
DECREASED IgA, G & E!
you see lyphopenia and cerebellar atrophy!
cutaneous erythmatous marks in a fern-leaf pattern are known as______and are an indication of________
LICHTENBURG FIGURES
LIGHTNING INJURY (can have 2nd degree burns too)
(ESPECIALLY IF THE PT IS FOUND ON WET GROUND OR UNDER A TREE AND UNCONSCIOUS )
whats the hallmark cell in a wilms tumor?
blastema!!!!!!!!!! = (immature kidney mesenchyme),
primitive glomeruli and tubules, and stromal cells
DOC for OCD (3)
(note: if there is a specific drug in one of the 3 classes for OCD, name it)
SSRIs
venlafaxine (SNRI)
clomipramine (TCA)******* know this association!
which immunosuppresant drug is a RF for Invasive CMV?
Mycophenolate mofetil
moa: Reversibly inhibits IMP dehydrogenase, preventing purine synthesis of B and T cells.
if you fuck up your LGN (lateral geniculate nucleus) WILL YOUR PUPIILARY LIGHT REFLEX be affected? like will you not constrict?
NOOOOOO!!!!!!!
LGN is involved in your VISION pathway with CN II
NOT CNIII in the PNS pathway for pupillary constriciton
if you messed up the LGN you woudlnt be able to too on one side of the eye on both eyes, like Left LGN injury–>vision in BOTH EYES on one side being affected/lost)
cholera and what e coli exotoxin have the same MOA
cholera
and
ETEC (one of its enterotoxins is the Heath Labile (LT) that also inc camp—> diahrrhea
SOMEONE HAS A HEMISECTION AT T8 (BROWN SEQUARD), WHAT LEVELS WILL HAVE LOSS OF PAIN (PINPRICK!) AND TEMP?
CONTRALAT LOSS OF PAIN AND TEMP
2 LEVELS BELOW AND EVERYTHING UNDER!
EG: INJURY AT T8
LOST OF PAIN AND TEMP ONE OR TWO SEGMENTS BELOW!!!! LIKE AT T9/T10!!
what vitamin does the following:
Antioxidant (protects RBCs and membranes from free radical damage).
Vitamin E (tocopherol/tocotrienol)
the following disease course: in a young and otherwise healthy pt
severe respiratory distress (fatigue, progressive dyspnea), atypical chest pain –> cyanosis and RVH/and or dilation of the RV (after long standing disease)–> death from decompensated cor pulmonale.
what disease process should be suspected
Pulmonary hypertension
[if the pulmonary HTN is due to Primary processes affecting the lung] its called “PAH (Pulmonary arterial hypertension )
whats the MOA for Iron poisoning and how it causes damage?
Cell death due to peroxidation of membrane lipids.
aspergillus Causes invasive aspergillosis, especially in immunocompromised and those with chronic granulomatous disease
what are specific RF’s to getting this?
what does aspergillus look like that makes it unique (aside from its ACUTE 45 angle branching)…
Major risk factors include
• Neutropenia!!!!!!!!!!!!!!!!
• Long-term high-dose corticosteroid therapy
• Organ transplantation (especially bone marrow transplantation)
• Hereditary disorders of neutrophil function (eg, chronic granulomatous disease)
• AIDS
Aspergillus sp tends to infect open spaces, such as pulmonary cavities caused by previous lung disorders (eg, bronchiectasis, tumor, TB), the sinuses, or ear canals (otomycosis).
UNIQUE:
Produces conidia in radiating chains at end of conidiophore E .

there is a patient with subacute endocarditis in a previously damaged heart valve who gets subacute endocarditis, what is the unique feature about this bug that allows for adherance to human surfaces and subsequent infection? whats the bug and some of its basic properties?
dextrans (insoluble extracell polysaccarhide), which bind to brin-platelet aggregates on damaged heart valves and tooth enamel.
STREP VIRIDANS {(Streptococcus mutans and S mitis) and subacute bacterial endocarditis at damaged heart valves (S sanguinis) )
Gram ⊕, α-hemolytic cocci.
Resistant to optochin, [differentiating them from S pneumoniae, which is α-hemolytic but is optochin sensitive]
what renal disease can Wilsons diseae lead to?
Fanconi Syndrome due to deposition of Cu in the PCT
YOU BETTER NOT FREAKIN GET CONFUSED BETWEEN ASPIRIN AND ACETMINOPHEN ANYMORE!!!!!!!!
HOW WOULD LAB VALUES IN both be DIFFERENT?
ASPIRIN = INC BLEEEEEDING TIME!!!
ACETMINOPHEN = INC PT!!!!!!!
WHICH EMBRYONIC WEEKS ARE extremely susceptible to teratogens
EMBRYONIC PERIOD
weeks 3-8
Neural tube formed by neuroectoderm and closes by week 4.
Organogenesis.
- unresponsiveness of kidney to PTH hypocalcemia despite PTH levels.
- Characterized by shortened 4th/5th digits,
- Short stature.
- Autosomal dominant.
- Due to defective Gs protein α-subunit causing end-organ resistance to PTH.
what is this disease? is it inherited from mom or dad? describe the disease the disease thats like this but thats inherited from the OTHER parent.
- Pseudohypoparathyroidism type 1A
(Albright hereditary osteodystrophy)
- Defect must be inherited from mother due to imprinting.
- Pseudopseudohypoparathyroidism—physical exam features of Albright hereditary osteodystrophy but without end-organ PTH resistance.
- Occurs when defective Gs protein α-subunit is inherited from father.
what nerve roots and nerver innervate the doral interosse which abdunt and adduct fingers
abduction and adduction of fingers (interossei),
Ulnar (C8-T1) !!!!
shifting sinusoidal waveforms on ECG is how it presents and is caused by: drugs, DEC K+ & DEC Mg2+
Torsades de pointes
WHAT ARE THE LEVELS OF EPO like in Polycythemia vera (JAK2 mutation)?
out of all the type of poycythemia, its is the only one that has DECREASED EPO due to negative feedback suppressing renal EPO production
which eye condition has painless porgressive vison loss beginning with NIGHT blindness bc its affects rods first?
retinitis pigmentosa
seen spicules arond macula
diaphragm innervates which two parts of the parietal pleura
diagphragmatic and mediastinal parts
what GI disorder is AKA: “pancreatic CHOLERA”
what else does this disease cause
VIPoma!
its also called WDHA (“whaddha” like “water”
stands for Watery Diarrhea HypoKalemia and Achlorhydria
bc it causes secretory diarrhea (3L/day)
not osmotic like lactose bc that would repsond to diet mod and not inflamm diarr bc that has pus or blood its SECRETORY (do to inc relase of na, cl and water into bowel)
TTP. talk about it.
whats the deficiency,
does it have Coombs’-negative hemolytic anemia. or Coombs’-positive hemolytic anemia?
involves nvolve nonimmunologic platelet destruction
Coombs’-negative hemolytic anemia!!!!!!!!
Inhibition or deficiency of ADAMTS 13 (vWF metalloprotease)—> degradation of vWF multimers.
Pathogenesis: INC large vWF multimers–> platelet adhesion–> platelet aggregation and thrombosis.
Labs:
- Schistocytes
- LDH
Symptoms: pentad of:
- neurologic
- renal symptoms
- fever
- thrombocytopenia,
- microangiopathic hemolytic anemia.
Treatment: plasmapheresis, steroids.
Triad of
polyarthralgias
tenosynovitis (eg, hand)
dermatitis (eg, pustules).
seen in ?
what is the other presentation of this condition? it has 2
Gonococcal arthritis
—STI that presents as either
1. purulent arthritis (eg, knee)
2. triad of polyarthralgias, tenosynovitis (eg, hand), dermatitis (eg, pustules).
what genetic principle is displayed by alpha 1 antitrypsin?
hint Blood groups A, B, AB also share this.
co dominance
when both alleles contribute to the phenotype of the heterozygote
which antimicrobial should be avoided by bc displaces BR from albumin and can lead to kernictuerus?
SUlfonamides
what two arteries mainly come off the external iliac artery? which one courses more medially?
the superficial epigastric artery and the inferior epigastric artery (more medial)