Thyroid Path Flashcards
(47 cards)
Describe the development of the thyroid gland…
- derived from median endodermal thickening near the foramen cecum. It later descends into the neck and forms gland - parafollicular C cells are derived from the ultimobranchial body
Congential abnormalities of Thyroid gland
- agenesis - lingual thyroid (problems with descent during development) - heterotopic thyroid tissue (pockets in neck) - thyroglossal duct cyst (neck cysts with thyroid tissue inside)
T/F thyroid pathology is more common in females than males
True!

Normal thyroid
Nontoxic Goiter
Causes…
Tx?
- -enlargement that is not associated with functional, inflammatory, or neoplastic alterations
- neither hyperthyroid nor hypothyroid (T4, T3, TSH usually normal)
- Usually asymptomatic except for presence of neck mass or local pressure on adjacent structures
- Thyroid growth may be related to an exaggerated response to normal TSH levels
- Treatment includes thyroid hormone–decreases TSH (feedback inhibition on pituitary)
- Radioactive iodine or surgery for local compressive symptoms
subtypes of non-toxic goiter
- Diffuse-more common in adolescence and during pregnancy
- Multinodular form more common > 50 years
- Both nontoxic and toxic multinodular goiter are much more common in females
- Many patients will progress to toxic multinodular goiter

nodular thyroid

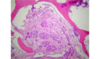
nodular goiter histo
compressed normal gland
Causes of Hypothyroidism
- defective synthesis of thyroid hormone with compensatory goiter (endemic)
- inadequate function due to decreased gland mass (surgery, inflammation, radiation therapy)
- inadequate TSH (pituitary), TRH (hypothalamus)
Systemic effects of hypothyroidism
- *Skin** – myxedema (puffy appearance), capillary fragility, i.e. easy bruising
- *Nervous System** - lethargy, somnolence, confusion, paranoia, severe agitation (myxedema madness), sensory deficits, cerebellar ataxia. Mucinous accumulations in cerebellum and nerve fibers.
- *Cardiovascular** - cardiac output decrease, myxedema heart (dilated cardiomyopathy), peripheral vascular resistance increased
Gastrointestinal - decreased peristalsis with constipation, myxedema megacolon
Reproductive
females- anovulatory failure, menstrual cycle disturbances
males - erectile dysfunction and oligospermia
Sx: 3 week old baby with apathy, lethargy, enlarged abdomen, decreased body temperature, refractory anemia, dilated heart, mental retardation (irreversible) and stunted growth
Dx?
Tx?
Causes?
Prognosis?
Dx? congenital hypothyroidism (cretinism)
Tx? prompt thyroid hormone replacement therapy
Causes? endemic (insufficient iodide in diet), sporadic, familial, secondary to thyroid dysgenesis
Prognosis? if not treated promptly, irreversible brain damage and dwarfism
Causes of goitrous hypothyroidism…
- Enlargement of thyroid due to inadequate thyroid hormone production
- Dietary iodine deficiency (Antithyroid agents–lithium, phenylbutazone, p-aminosalicylic acid or Foods with goitrogens–Rutabagas, turnips, cassava)
- Iodide induced goiter–Excessive dietary iodide (seaweed, supplements)
- High dose iodine in pregnancy can produce goitrous infants
- Hereditary defects in thyroid hormone synthesis
Causes of hyperthyroidism…
- may occur secondary to increased TSH production (rare)
- abnormal stimulation of thyroid (Graves)
- extrinsic production from ectopic thyroid tissue, i.e. struma ovarii (rare)
- Thyroiditis (early stages, thyroid follicles destroyed and excessive TH released into blood)
- -may or may not cause goiter
Features of toxic multinodular goiter
- development of functional autonomy of a nodule(s) from a nontoxic goiter
- unresponsive to thyroid hormone administration
- Uptake of iodine may be diffuse or only within hyperfunctioning nodules. Other more normal follicles are suppressed.
- The clinical presentation may be similar to a toxic (functioning) adenoma (but adenoma is generally solitary)
- Hyperthyroidism not as severe as in Grave’s (no exophthalmos)
- T4, T3, only minimally elevated or normal
- Treatment: radioactive iodine after anti-thyroid therapy.
Sx: nervousness, tremor, weakness, wt loss, heat intolerance, palpitations
PE: hyperthyroidism, diffuse goiter with bruits, exopthalmos, dermopathy
Tests: increased radioactive iodine uptake and elevated T3 and T4
Dx?
Causes?
Tx?
Dx: Grave’s disease
Cause: autoimmune–anti-TSH receptor stimulating antibodies
Tx:
- antithyroid medications
- radioactive iodine, along with corticosteroids and adrenergic
antagonists - exophthalmos does not resolve with treatment and may worsen
- thyroid failure may ensue

Grave’s disease
-Diffusely hyperplastic thyroid

Grave’s disease histo
- Papillary projections of epithelium into follicles with scalloped borders
- lymphoplasmacytic infiltrate (not shown)

- treated graves disease
- Diffusely hyperplastic with numerous papillary projections and little colloid
Toxic adenoma
- cause of hyperthyroidism
- hyperfunctioning, autonomous “hot” nodule
- infrequent cause of hyperthyroidism
- treated with radioactive iodine and/or surgery
Hypersecretion of TSH
- cause of hyperthyroidism
- thyrotropin adenoma
- TSH-like substances secreted by trophoblastic tumors
Dx?
Histo?
clinical features?
Tx?

Dx: hashimotos thyroiditis histo
histo: lymphoplasmacytic infiltrate, destruction and atrophy of follicles, Hurthle (Askanazy) cell metaplasia
Clinical features: gradual development goiter, hypothyroidism, elevated TSH, circulating antibodies
Tx: hormone replacement
subacute thyroiditis

-painful
- DeQuervain, Granulomatous, or giant cell thyroiditis
- follows URI, caused by viral infection (influenza, adenovirus, echo, coxsackie, possibly mumps)
- granulomatous inflammation (not lymphoplasmocytic)
- transient hyperthyroidism with destruction of follicles
- euthyroid state restored upon recovery
histo: DeQuervain’s thyroiditis with giant cells
silent thyroiditis
- painless subacute thyroiditis
- Lack of anti-thyroid antibodies or autoimmune thyroiditis
- affects mostly post-partum females
- typically resolves over several months
What type of thyroiditis?
Features?
Histo?

- *Riedel Thyroiditis**
- dense fibrosis of thyroid
- associated with extrathyroidal fibrosis including:
- retroperitoneum
- mediastinum
- not related to other thyroiditides
- *Histology**
- dense hyalinized tissue with chronic inflammatory infiltrate