Systems 2 - Integrated Physiology Flashcards
Equivalents
= moles x valence
So 1 mol Na⁺ = 1 eq/L
1 mol Ca²⁺ = 2 eq/L
Moles are unit of quantity, 6 x 10²³
PaCO₂
PaCO₂ (arterial) = Rate of CO₂ production / alveolar ventilation rate
Quantity of moles
1 mole =
10³ mmol
10⁶ μmol
10⁹ nmol
pH equations
pH = -log[H⁺]
So minor changes in pH -> major changes in [H⁺]
pH = pk + log[A⁻]/[HA]
Importance of pH in body
- enzyme activity/protein strucure affected
- Ca²⁺ ions - 50% are free in blood, ionised, to stabilise nerve and muscle membranes. 50% are bound to albumin, which competes with H⁺ for binding. -> when decreased H⁺, less free Ca²⁺, so less of a membrane stabilising effect
- –> so in hyperventilation, increased pH, hyperexcitable nerves
Trousseau sign, Chvostek’s sign
Trousseau - hand cramped forward, claw
Chvostek - muscle twitch when tap facial nerve
-> indicate disturbance of plasma calcium, or acid/base balance disruption
Buffers
Resist a change in pH by absorbing or releasing H⁺ when an acid or base is added
pH will still change slightly - buffer pair is weak acid and its conjugate base
pk
= the pH where an acid is 50% dissociated, [A⁻]/[HA] = 1
Lower pk -> stronger acid
Extracellular buffers
Bicarbonate
Haemoglobin
Phosphate
Plasma proteins
-> work together to resist change, isohydric principle
Bicarbonate buffer system
pk = 6.1 CO₂ + H₂O = H₂CO₃ = H⁺ + HCO₃⁻
BUT rarely know [H₂CO₃], so use solubility coefficient of 0.03 - [H₂CO₃] = 0.03 x PCO₂
- > pH ∝ [HCO₃⁻]/PaCO₂
- > pH depends on the ratio of bicarbonate to carbon dioxide
IMPORTANT
- high conc of buffer pair in plasma
- PaCO₂ regulated by respiratory system
- [HCO₃⁻] regulated by kidney
Acid production in body
Body is net producer of acid
Kreb’s cycle makes CO₂
Metabolism makes H⁺
Gut below pylorus -> HCO₃⁻ to lumen in alkaline tide, H⁺ into blood
Renal handling of bicarbonate
Reabsorption - of bicarbonate ions by glomerular filtration. If too high, exceeds tubular threshold and spills into urine
Regeneration - of bicarbonate lost in buffering, by secreting protons into nephron to be trapped and excreted by non-bicarbonate buffers, and by secreting ammonium
-aemia
Acidaemia - acidic blood, pH less than 7.35
Alkalaemia - alkaline blood, pH more than 7.45
-osis
Acidosis/alkalosis - processes that cause a change in pH of blood
Usually -> -aemia
‘osis-without-aemia’ when pH in normal range
Compensation
Attempts to return pH to normal
Pathological chronic change in PCO₂ or HCO₃⁻ is compensated by homeostatic change in the other
Renal compensation (adjusting HCO₃⁻) is more effective than respiratory compensation (adjusting CO₂) but takes longer to get effect, days
-> if renal and lung disease, big problem
Change in same direction, if increase in HCO₃⁻, body will increase CO₂ to compensate
Normal range of pH, PCO₂, HCO₃⁻
pH - 7.35-7.45
PCO₂ - 35-45
HCO₃⁻ - 21-29
Alkalaemia
pH > 7.45
HCO₃⁻ raised, metabolic alkalosis
PCO₂ decreased, respiratory alkalosis
Acidaemia
pH < 7.45
HCO₃⁻ decreased, metabolic acidosis
PCO₂ raised, respiratory acidosis
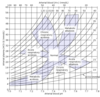
Acid base map
Electroneutrality
Total [cations] = total [anions] in body fluids, can’t have net charge
Anion gap in -ve ions, unsure where from
Normally 8-16mEq/L
Other anions are Cl⁻ and HCO₃⁻
Hyperchloraemic metabolic acidosis with normal anion gap
As cations have increased, to fill in gap, Cl⁻ increases
Anion gap remains unchanged
Caused by too much bicarb out
Increased anion gap metabolic acidosis
As bicarbonate has decreased, to fill in gap, anion gap increasases
Cl⁻ remains unchanged
Caused by too much acid in
Causes of increased anion gap metabolic acidosis
- more fixed acid production, eg lactic acidosis/ketoacidosis
- ingestion of fixed acids, eg aspirin
- inability to excrete fixed acids, eg in renal failure
Causes of hyperchloraemic metabolic acidosis with normal anion gap
- loss of bicarb from gut, eg diarrhoea, ileostomy
- loss of bicarb via kidney, eg renal tubular acidosis


