Symposium - Alcohol Misuse Flashcards
Through what mechanisms does alcohol contribute to mortality in the following age groups:
- 16 to 34
- 34 to 64
- 64+
- 16-34 years
- Accidents/traumas
- Self-harm and suicide
- Alcohol intoxication (poisoning)
- 34-64 years
- Alcohol related liver disease
- 64+
- Alcohol related cancers
What are the principles of the WHO global alcohol strategy?
- Availability
- Regulation of marketing
- Price controls (cheapest alcohol)
- Leadership and mentoring
- Early identification and advice
What are the effects of alcohol at low and high doses?
- Low doses
- Euphoria, reduced anxiety, relaxation, sociability
- High doses
- Intoxication (the pathological state produced by a drug, serum, alcohol or any toxic substance), basically poisoning
- Impaired attention and judgement, unsteadiness, flushing, nystagmus, mood instability, disinhibition, slurring, stupor, unconsciousness
What is intoxication?
- Intoxication (the pathological state produced by a drug, serum, alcohol or any toxic substance), basically poisoning
What is used to grade alcoholism?
ICU-10
What are the different grades of alcoholism?
-
Harmful use
- Pattern of use causing damage to physical or mental health
- Use > 1 month or repeatedly over 12 months
-
Dependence
- 3 or more of the following for >1month or repeatedly over 12 months
- Cravings/compulsions to take
- Difficulty controlling use
- Primacy
- Increased tolerance
- Physiological withdrawal on reduction/cessation
- Persistence despite harmful consequences
- 3 or more of the following for >1month or repeatedly over 12 months
-
Withdrawal state
- Group of symptoms of variable clustering and severity on complete/relative withdrawal of a psychoactive substance, after persistent use of that substance
- Tremor, weakness, nausea, vomiting, anxiety, seizures, confusion, agitation, death
- Delirium tremens
- Profound confusion, tremor, agitation, hallucinations, delusions, sleeplessness, autonomic over-activity
- Death – cardiovascular collapse, infection, hyperthermia, seizures of self-injury
- Usually 48-72 hours after alcohol stopped
What is the criteria for the following grades:
- harmful use
- dependence
- withdrawal state
- Harmful use
- Pattern of use causing damage to physical or mental health
- Use > 1 month or repeatedly over 12 months
- Dependence
- 3 or more of the following for >1month or repeatedly over 12 months
- Cravings/compulsions to take
- Difficulty controlling use
- Primacy
- Increased tolerance
- Physiological withdrawal on reduction/cessation
- Persistence despite harmful consequences
- 3 or more of the following for >1month or repeatedly over 12 months
- Withdrawal state
- Group of symptoms of variable clustering and severity on complete/relative withdrawal of a psychoactive substance, after persistent use of that substance
- Tremor, weakness, nausea, vomiting, anxiety, seizures, confusion, agitation, death
- Delirium tremens
- Profound confusion, tremor, agitation, hallucinations, delusions, sleeplessness, autonomic over-activity
- Death – cardiovascular collapse, infection, hyperthermia, seizures of self-injury
- Usually 48-72 hours after alcohol stopped
What is seen in delirium tremens?
- Profound confusion, tremor, agitation, hallucinations, delusions, sleeplessness, autonomic over-activity
- Death – cardiovascular collapse, infection, hyperthermia, seizures of self-injury
- Usually 48-72 hours after alcohol stopped
When does delirium tremens usually begin?
- Usually 48-72 hours after alcohol stopped
What are some examples of problems that alcohol can cause?
- Physical health
- Affects every part of your body, every organ system
- Find examples below
- Mental health
- Depression
- Sleep disruption
- Morbid jealousy
- Alcohol hallucinosis
- Deliberate self-injury
- Suicidal thoughts/acts
- Relationships
- Aggression
- Marital difficulties
- Poor parenting
- Loss of friendships and social supports
- Employment, financial
- Legal
What are some health conditions directly related to alcohol?
- Wernicke’s encephalopathy
- Confusion, ataxia, opthalmoplegia, nystagmus
- Koraskoff’s psychosis
- Prominent impairment of recent and remote memory, preservation of immediate recall, impaired learning and disorientation
- May exhibit nystagmus and ataxia
- Due to thiamine deficiency
Wernicke’s encephalopathy - clinical featrures
- Confusion, ataxia, opthalmoplegia, nystagmus
Koraskoff’s psychosis - clinical features
- Prominent impairment of recent and remote memory, preservation of immediate recall, impaired learning and disorientation
- May exhibit nystagmus and ataxia
Karoskoff’s psychosis - aetiology
- Due to thiamine deficiency
What are some screening tools for alcoholism?
- CAGE (2 or more indicates alcohol problem)
- Have you tried to Cut down
- Have you felt Annoyed by people critisising your drinking
- Have you felt Guilty about drinking
- Have you felt the need to have an Eye opener
- AUDIT (alcohol use disorders identification test)
- FAST (4 questions)
- PAT (Paddington Alcohol Test) – used in A and E
What are the 4 questions of CAGE?
- CAGE (2 or more indicates alcohol problem)
- Have you tried to Cut down
- Have you felt Annoyed by people critisising your drinking
- Have you felt Guilty about drinking
- Have you felt the need to have an Eye opener
What screening tool is used in A&E?
- PAT (Paddington Alcohol Test) – used in A and E
Describe the management of alcoholism?
- Practical advice, education, harm reduction
- Holistic/bio-psycho-social approach
- Support for patient and family
- Psychological help such as CBT, group therapy
- Social work input (benefits, housing, child protection)
- Skills training
- Community support such as AA
- Inpatient or residential treatment
- Medication
- Thiamine to prevent Wernicke-Korsakoff syndrome
- Management of alcohol withdrawal – benzodiazepines
- Aversion/deterrent medication – disulfiram
- Anti-craving medication – acamprosate, naltrexone, nalmefene
What medications can be used in alcoholism?
- Thiamine to prevent Wernicke-Korsakoff syndrome
- Management of alcohol withdrawal – benzodiazepines
- Aversion/deterrent medication – disulfiram
- Anti-craving medication – acamprosate, naltrexone, nalmefene
What organ systems are affected by alcohol?
Each organ system is affected, particular the liver

Alcoholic fatty liver - prognosis
- 20% progress to cirrhosis
- Alcohol abstinence returns fatty liver to normal
Alcohlic fatty liver - epidemiology
- Most heavy drinkers have fatty liver
Acute alcoholic hepatitis - diagnosis critera
- Alcohol intake >6u(units) per day
- Jaundice with bilirubin > 80mg/dl
- No other aetiology for liver inflammation
Alcoholic hepatitis - prognosis
- Very high mortality, no specific treatment yet
What scoring system is used to grade acute alcoholic hepatitis?
GAHS score
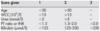
What does the GAHS score consider?

Mortality is high for what GAHS score?
If score is 9 or more mortality is high, but steroids help
How can alcoholism cause malnutrition?
- 60% of chronic abusers have malnutrition
- Most of the calories is from alcohol
- Total energy intake reduced
- Nausea and vomiting
- Abdominal pain
- Diarrhoea
How do different peopole with alcoholic cirrhosis die?
Mortality in alcoholic cirrhosis is high:
- 75% die of liver compensation
- 25% die from hepatocellular cancer sequelae
- Most need transplant
- ARLD most common indication for transplant
What is commonly seen in teenangers who drink a lot?
Alcohol and teenagers:
- Cirrhosis rare
- Deranged LFT common, especially in obese
Describe the pathophysiology of alcoholic ketoacidosis?
- Lipolysis tends to increase because of increased levels of cortisol and catecholamines, causes by extra stress placed on body by alcohol
- Lipolysis contributes to abundance of FFA, which in turn sees diverted ketone production
- Usually the ketone beta-hydroxybutyrate
- Excess alcohol metabolised drives NADH+ production, which drives production of ketone beta-hydroxybutyrate
- Chronic alcohol misusers have depleted reserve, ethanol will provide calorie intake though glycogen stores depleted
- Metabolism of ethanol raises NADH/NAD which impairs hepatic gluconeogenesis and the metabolism of lactate
- So patient has impaired ability to make glucose, or metabolise lactate driving the hypoglycaemia and acidosis
What ketone is usually seen in alcoholic ketoacidosis?
- Usually the ketone beta-hydroxybutyrate
What is done to stailise a patient with alcoholic ketoacidosis?
To stabilise patient:
- IV fluids
- IV vitamin B1 (thiamine)
What is vitamin B1?
Thiamine
Why is thiamine so important for metabolism?
Thiamine is used at multiple points as co-factor

What act describes the alcohol laws?
Licensing (Scotland) Act 2005
What are some of the principles of the Licensing (Scotland) Act 2005?
- Provides regulation of the sale of alcohol
- Illegal to
- Sale to under 18 or to allow consumption of
- Attempt to enter pub whilst drunk
- Sell to drunk person
- Whilst drunk behave in disorderly manner
- Refuse to leave
- Allow drunkenness or disorderly conduct
In relation to the law, what does alcohol increase the risk of?
- Committing crime
- Becoming victim of crime or misadventure
- Adverse incidents


