Staining and Ocular Response to CL Flashcards
(67 cards)
Why do you want to conduct an after care appt?
Ensure optimum comfort and optical performance
- Minimise drop-outs
- Answer patient queries/questions
- Address any compliance issues – Safety: reduce risk of infection
- Assess the ocular reaction to a lens
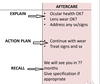
How do you conduct an appt for a new fit of contact lenses?

How do you conduct an aftercare appt?

How does a history and symptoms check for contact lenses differ to that of a routine check up?
CL history and syptoms focuses on the motivation for contact lenses and whether CL are appropriate for how the px wants to wear them
What are some common reasons for why patients chose to wear CLs?
For Cosmetic purposes i.e. they have a high Rx or anisometropia.
Sports where glasses are impractical
Special Occasions
Therapeutic Reasons i.e. for some ocular conditions
What should be recorded in a history and symptoms of a CL aftercare appt?
What type of visit is it? • Routine? • Unscheduled visit?
A Determination of whether there are any problems
A Follow up of advice that was given at the previous visit
e.g. • Use of eye drops • Advice regarding wear time
How the px feels about vision in their contact lenses.
Ocular Health
Medications
Lifestyle/Hobbies
What vision related questions are we asking our px in history and symptoms for a CL aftercare appt?
We are asking how their vision is in the CLs and how that compares to their glasses.
We ask whether the patient is experiencing any fluctuations in vision - if so when?
Whether blinking has any effect on their vision.
What vision related questions are we asking our patient in history and symptoms for a new fit CL appt (and why)?
What is the VA like compared to their glasses?
In order to determine the presence of any issues that may affect the VA through CLs e.g. amblyopia or presbyopia
What questions do we ask in regards to ocular health in the history and symptoms portion of a CL aftercare appt?
Any new problems?
COMFORT:
• Issues when wearing CLs? e.g. about Lenses drying out, ocular discomfort, redness, pain?
QUS ABOUT LENSES:
• Age of lens/case? • Cleaning of lenses/case? • Solution?
WEAR TIMES:
Days (/7), hours (/24), max, average, and today, as well as comfortability
What do we check in regards to ocular health in the history and symptoms portion of a CL new fit appt?
Check for symptoms
- Are there any contraindications to lens wear? (such as a red or pink eye, or discharge etc)
- Does patient require treatment prior to fitting?
What are very important symptoms to look out for?
Light sensitvity (photophobia)
Discharge
Pain
Sudden blurry Vision/Vision loss
If a patient complains of any symptom how do we investigate this further- i.e. what questions to we ask?

What does CLPC stand for?
Contact Lens Pupillary Conjunctivitis
If a patient experiences a sudden onset of discomfort or discomfort upon insertion of the contact lens what are some possible causes for this?
A foreign body
A damaged lens
Conjunctival irritation
Corneal Abbrasion
Excessive movement of the lens
If a patient experiences discomfort after during a period of wearing CLs what could be the cause of this?
Lens Deposits
Ocular surface Dehydration as a result of wetting properties of the lens
Issues with the environment in which the lens is worn i.e. dry environment - lots of air conditioning
Trapped Debris
CLPC
If a patient experiences discomfort after a period of wearing contact lenses - what are possible causes of this?
Corneal Abraison
SEAL - Superior Epithelial Arcuate lesion
Inflammation/Infectin
[Here the CL acts as a bandaid and whenremoved the px experiences symptoms]
If a patient is experiencing constant blurred vision with their CLs on, what may be the possible cause of this?
They’ve accidentally switched their lenses i.e. Left CL in right eye and Right CL in the Left eye.
The Rx is incorrect
They are experiencing residual astigmatism
The lens is distorted
If a patient is experiencing blurred vision that fluctuates with blinking whilst wearing their CLs , what may be the cause of this?
Any one of the following could be a possible cause:
- Lens deposits (if vision is better post blinking)
- Excessive lens movement (if vision is worse post blinking)
- The lens has been inserted inside out (i.e. not the boat shape)
If a patient experiences blurred vision with their CLs throughout the course of the day whilst wearing them, what may be a possible cause of this?
Lens Deposits
The lens surface drying out
What are a list of possible triggers for any symptom a px experiences with CLs?
The lenses themselves
The lens case
The lens solution
The environment in which they are worn
The px themsleves by being irresponsible i.e. showering or swimming in lenses, creams , makeup etc.
(A combination of all these factors)
Why is it helpful to ask a patient about the severity of a symptom?
Despite it being subjective it can be a good way of monitoring progression/ changes to symptoms.
Also allows us to record if any treatments were particularly effective at removing symptoms such as discomfort.
When recording previous Ocular history as part of history and symptoms, for a new fit CL appt what types of questions do we want to be asking and why?
We want to be asking whether they have suffered from any eye conditions as that may affect the type of lens we prescribe.
If they have worn contacts before we want to ask why they stopped wearing contacts so that we can resolve any previously experienced problems - in this case, we also want to be recording which lenses those were.
What questions are we asking and focusing on when recording ocular history in a CL aftercare appt?
Checking previous records and confirming them
Asking about whether the px is experiencing any new symptoms or any conditions which may affect the eyes and subsequently lens wear.
What allergies/conditions should we be asking our patient about, due to their systemic association with the eyes and as a result CL wear?
General Allergies
Presence of Ezcema
Diabetes
Rheumatoid Arthritis