SM 189a/190a - Functional Renal Anatomy and Glomerular Filtration, Regulation Flashcards
Which of the following would tend to decrease GFR?
- An increase in hydrostatic pressure in the glomerular capillary
- A decrease in oncotic pressure in the glomerular capillary
- A decrease in total glomerular capillary surface area
c. A decrease in total glomerular capillary surface area
If solute delivery to the juxtaglomerular apparatus is too high, which cells respond?
What is the response?
- Macula densa senses increase in solute (Na+) delivery
- Macula densa releases adenosine
- Adenosine causes extraglomerular mesangial cells to contract and cause vasocaonstriction of the afferent arteriole
What is the equation for clearance (kidney)?

Which of the following is NOT a component of the glomerular permeability barrier?
a. Visceral epithelial cells (a.k.a. podocytes)
b. Glomerular basement membrane
c. Parietal epithelial cells (a.k.a. Bowman’s capsule)
d. Negatively charged glycosaminoglycans
e. Glomerular capillary endothelial cells
c. Parietal epithelial cells (a.k.a. Bowman’s capsule)
What fraction of cardiac output goes through the kidney?
20%
If solute delivery to the juxtaglomerular apparatus is too low, which cells respond?
What is the response?
- Macula densa senses decrease in solute (Cl-) delivery and/or flow
- Signals to the granular cells in the wall of the afferent arteriole
- Granular cells release renin
- Renin secretion -> Increased Angiotensin II production
-
Angiotensin II ->
- Increased Na/H exchange
- Constriction of the efferent arteriole
- Aldosterone secretion -> Na+ reabsorption
What are the requirements for the use of creatinine clearance for GFR?
- Renal function must be in steady-state
- No vigorous activity or muscle breakdown
- No protein loading
What is the function of the macula densa?
The macula densa…
- Senses changes in solute concentration and tubular flow
- Communicates to granular cells in wall of afferent arteriole if solute (Cl-) delivery and flow are low
- -> Granular cells release renin
- Communicates to extraglomerular mesangial cells of solute (Na+) delivery and flow are high
- -> Mesangial cells contract, causing constriction of the afferent arteriole (tubuloglomerular feedback)
Which macromolecules will filter through the glomerular permeability barrier more easily:
Positively charged, negatively charged, or neutral?
Why?
Positively charged
The glomerular basement membrane contains anionic glycosaminoglycans that repell negatively charged molecules
[smaller molecules filter more easily than large]
How do the Starling forces change from the affertent to efferent arterioles of the glomerulus?
- PGC remains constant, may drop slightly
- PBS remains constant
- πGC increases
- Fluid is leaving, protein concentration in the glomerular capillary increases
- πBS remains zero

Filtration stops when πGC increases to oppose PGC
What are mesangial cells?
Supporting cells of the glomerulus that help to maintain capillary structure
They can contract (contain actin and myosin)
Where in the kidney does filtration occur?
Glomerulus
(Located in the cortex)
Filtration = fluid going from capillaries to Bowman’s space; this is the ultrafiltrate that will eventually become urine
Does albumin filter into the urine?
Why or why not?
Albumin does not filter into the urine
It is large and negatively charged - it cannot get through the glomerular permeability barrier
(Fenestrated endothelium, GBM, Foot processes of podocytes)
What mechanisms affect LpS?

Mesangial cell contraction can decrease capillary surface area
Decreased surface area (S) = decreaed GFR
Lp remains constant
Which of the following statements about creatinine is FALSE?
- Creatinine is freely filtered by the glomerulus
- Creatinine is neither reabsorbed nor secreted by the tubules
- Creatinine is a clinically useful marker of GFR
- Cimetidine may increase the plasma creatinine concentration
b. Creatinine is neither reabsorbed nor secreted by the tubules
(I think this is right, but let me know if not!)
Where in the kidney does filtration take place?
Glomerulus
Filtration = movement from glomerular capillaries -> Bowman’s capsule
What is angiotensin II?
What are the effects?
Angiotensin II is a potent vasoconstrictor
- Kidney
- Vasoconstriction of the efferent arteriole
- -> Raises PGC and increases GFR in response to low Cl- delivery to the macula densa or beta-1 adrenergic stimulation
- Systemic
- Rise in blood pressure
What is the basis for the structural difference between the thin and thick ascending loop of Henle?
What does this tell us about their functions?
The thick ascending limb is thick because the walls are full of mitochondria
The mitochondria in the thick ascending limb generate ATP that fuels active transport of NaCl into the medulla to increase osmolality in the medullay, which drives the countercurrent multiplier
Describe the sequence of events that happens if renal blood flow increases
- PGC (Hydrostatic pressure in the glomerular capillary) increases
- GFR increases
- Macula densa senses increased NaCl in the ultrafiltrate
- Macula densa releases ATP into extracellular space
- ATP is converted to adenosine
- Adenosine activates mesangial cells to contract, causing vasoconstriction of the afferent arteriole
- PGC decreases
- GFR returns to normal
- Macula densa senses return to normal, stops releasing ATP into the extracellular space
Which of the following statements is most consistent with tubuloglomerular feedback?
- increased NaCl delivery to the thick ascending limb causes increased proximal fluid reabsorption.
- decreased NaCl delivery to the thick ascending limb causes increased proximal fluid reabsorption.
- increased NaCl delivery to the thick ascending limb causes no change in proximal fluid reabsorption.
- increased NaCl delivery to the thick ascending limb causes decreased glomerular filtration rate
- increased NaCl delivery to the thick ascending limb causes increased glomerular filtration rate
D. increased NaCl delivery to the thick ascending limb causes decreased glomerular filtration rate
What is the equation for glomerular filtration rate (GFR)?
- Δπ = π inside of the glomerular capillary
- Oncotic pressure inside of Bowman’s space is zero
- Hydrostatic pressure in the glomular is the driver of glomerular filtration

What are the major differences between cortical and juxtamedullary nephrons
-
Location
- Cortical: mid-outer cortex
- Juxtamedullary: boundary of cortex and outer medulla
-
Loop of Henle
- Cortical: short
- Juxtamedullary: long
-
Function
- Cortical: recieve 95% of filtrate
- Juxtamedullary: establish high osmolarity in the inner medulla -> countercurrent multiplier
-
Abundance
- Cortical: more abunant
- Juxtamedullary: less abundant
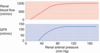
Why doesn’t renal artery pressure have a large effect on GFR?
The afferent arteriole that leads into the glomerulus “protects” the glomerular capillary bed from changes in renal artery pressure
The affernet arteriole is under control of the intrinsic myogenic reflex, vasoconstrictors, and vasodilators
What is the role of renin secretion in autoregulation of GFR?
Renin secretion -> Angiotensin II production (via RAAs)
Active when renal arterial pressure is low
Responsible for raising glomerular capillary pressure to maintian GFR