Session 5 - Health Promotion, Screening and Risk Communication Flashcards
What are meant by determinants of health?
- A range of factors that have a powerful and cumulative effect on the health of populations, communities and individuals:*
- Physical environment*
- Social & economic environment*
- Individual genetics, characteristics and behaviours*
- On this basis therefore, individuals are unlikely to be able to directly control many determinants of health and so blaming them for poor health or crediting them for good health is inappropriate.*
What is health promotion?
- EMPOWERING
- PARTICIPATORY
- HOLISTIC
- INTERSECTORAL
- EQUITABLE
- SUSTAINABLE
- MULTI-STRATEGY

What are the 5 approaches to health promotion?
- Medical or preventative
- Behaviour change e.g. Smoking = Ask, Advise, Act
- Educational e.g. Smoking posters
- Empowerment
- Social change e.g. banning smoking in public places
There are 3 levels of prevention.
What is meant by PRIMARY PREVENTION?
Aiming to prevent the onset of disease or injury. Often has 4 approaches:
- Immunisation
- Prevention of contact with environmental risk factors.
- Taking appropriate precautions re communicable disease.
- Reducing risk factors from health related behaviours.
There are 3 levels of prevention.
What is meant by SECONDARY PREVENTION?
Aiming to detect and treat a disease at an early stage (to prevent progression/potential future complications)
Examples include:
- Screening for cervical cancer
- Monitoring and treating blood pressure
- Screening for glaucoma.
There are 3 levels of prevention.
What is meant by TERTIARY PREVENTION?
Aims to minimise the effects of established disease. Examples include:
- Maximising the remaining capabilities and functions of an already disabled patient
- Renal transplants
- Steroids for asthma
What are 6 dilemmas around health promotion?
1. Interfering in people’s lives
2. Victim blaming (ignoring determinants of health that cannot be directly controlled)
3. Fallacy of empowerment (having the information doesn’t mean people can act on this because there may be adverse circumstances and wider socio-economic determinants of health limiting this ability).
4. Reinforcing negative stereotypes (e.g leaflets aimed at HIV prevention in drug users can reinforce idea they are only to blame for their situation).
5. Unequal distribution of responsibility (e.g. women are responsible for implementing health behaviours).
6. Prevention Paradox (interventions that make a difference at a population level might not have much effect on the individual [people may not see themselves as a ‘candidate’, and there are also elements of anomalies and randomness of a disease])
Define ‘evaluation’, and why it is carried out.
- The rigorous & systematic collection of data to assess the effectiveness of a programme in achieving predetermined objectives.*
- Needed for evidence-based interventions.*
- Accountability*
- Ethical obligation*
- Programme management & development*
There are 3 types of evaluation.
What is meant by PROCESS evaluation?
- Focuses on assessing the process of programme implementation.
- AKA formative or illuminative evaluation.
There are 3 types of evaluation.
What is meant by IMPACT evaluation?
Assessing the immediate effects of the intevention.
There are 3 types of evaluation.
What is meant by OUTCOME evaluation?
Measuring long-term consequences e.g. improvement in lives, reduction of symptoms.
NB:// The timing of evaluation can influence the outcome - Delay (take time to have effect) and Decay (wear off rapidly)
What is meant by the term ‘diagnosis’?
The definitive identification of a suspected disease or defect by application of tests, examinations or other procedures (which can be extensive) to definitely label people as either having a disease or not having a disease.
Outline 3 ways in which disease can be detected.
- Spontaneous Presentation
- Opportunistic Case Finding
- Screening
What is SCREENING?
A systematic attempt to detect an _unrecognised_ condition by the application of tests, examinations or other procedures, which can be applied _rapidly_ (and cheaply) to distinguish between _apparently well persons_ who _probably_ have a disease (or its precursor) and those who _probably do not_.
For what purpose(s) is screening carried out?
- To give a better outcome compared with finding something in the usual way (i.e. having symptoms and self-reporting).
- If treatment can wait until there are symptoms there is no point in screening.
NB:// Finding something earlier is NOT the primary objective.
Give examples of some screening programmes.
- AAA screening programme
- Bowel cancer screening programme
- Breast screening programme
- Cervical screening programme
- Fetal anomaly screening programme
Give 3 examples of diseases where there is no national screening programme (or a restricted one)…
- Prostate Cancer (PSA test)
- Breast Cancer screening for those women <50 yrs.
- Cervical Cancer screening for women <25 yrs.
There are five areas of criteria for screening:
1. Condition
2. Test
3. Intervention
4. Screening programme
5. Implementation.
Describe and explain what is meant by ‘Condition’
- It must be an important health problem (frequency/severity) with epidemiology, incidence and prevalence understood.
- All cost-effective primary prevention interventions should have been implemented as far as practicable.
There are five areas of criteria for screening:
1. Condition
2. Test
3. Intervention
4. Screening programme
5. Implementation.
Describe and explain what is meant by the ‘Test’
- Has to be simple, safe, precise and validated.
- It must be acceptable to the target population.
- The distribution of test values in the population must be known with an agreed cut-off-level.
- There must be an agreed policy on further diagnostic investigation for those who have a +ve result.
There are five areas of criteria for screening:
1. Condition
2. Test
3. Intervention
4. Screening programme
5. Implementation.
Describe and explain what is meant by the ‘Intervention’
- Evidence is required that intervention at a pre-symptomatic phase leads to better outcomes for the screened individual compared with usual care.
There are five areas of criteria for screening:
1. Condition
2. Test
3. Intervention
4. Screening programme
5. Implementation.
Describe and explain what is meant by the ‘Screening programme’
- There needs to be a proven effectiveness in reducing mortality or mobidity (high quality RCT data).
- The complete screening programme must be clinically, socially and ethically acceptable to health professionals and the public.
- The benefit gained by individuals should outweigh any harms (e.g. from overdiagnosis, overtreatment).
- The opportunity cost of the screening programme should be economically balanced in relation to expenditure on medical care as a whole.
There are five areas of criteria for screening:
1. Condition
2. Test
3. Intervention
4. Screening programme
5. Implementation.
Describe and explain what is meant by the ‘Implementation’
- That clinical management and patient outcomes should be optimised in all healthcare providers.
- All other options for managing the condition should have been considered.
- There should be adequate staffing and facilities for the programme.
- Evidence-based information should be available to potential participants (informed choice).
- Public pressure should be anticipated.
Discuss some of the difficulties (3) in evaluating screening programmes.
1. Lead time bias => early diagnosis falsely appears to prolong survival i.e patients live the same length of time, but simply know about the disease for longer.
2. Length time bias => Screening programmes are better at picking up slow growing, unthreatening cases rather than aggressive, fast-growing cases.
3. Selection bias => studies often skewed by ‘healthy volunteer effect’ i.e. those who have regular screening are likely to do other things to protect them from disease.
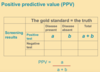
What are the 2 types of error that any screening test is going to make?
- It is going to refer well people for further investigation i.e FALSE POSITIVES.
* (stress, anxiety, direct & opportunity costs)* - It is going to fail to refer people who do actually have an early form of the disease i.e. FALSE NEGATIVES.
* (inappropriate reassurance and delay)*