Scoring systems Flashcards
(41 cards)
What is the scoring system used to assess the liklihood of a septic joint (eg septic arthritis vs transient synovitis)?

What is the scoring system used to assess stroke risk in patients with AF?
CHA2DS2-VASc

What is the scoring system to evaluate risk of haemorrhage on anticoagulation for AF?
HASBLED Score

List the elements of the PERC Score.
Who should it be used in?
Effectively rules out PE (<2% probability) in patients with a pre-test probability of <15%.

What are the elements of the Well’s Score?
What do the scores equate to?
<2 points: low risk = (1.3% incidence PE) -> PERC or D-dimer
Score 2-6 points: moderate risk (16.2% incidence of PE): D-dimer testing or CTA.
Score >6 points: high risk (37.5% incidence of PE): consider CTA. D-dimer testing is not recommended.

What is the HEART Score?
What does it predict?
Predicts the risk of Major Adverse Coronary Events (MACE) in the next 6/52 for patients with undifferentiated chest pain.

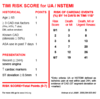
What is the TIMI Score for NSTEMI/UA?
What does it predict?
Give an estimate of the risk for various scores.
What is the GRACE Score?
What is it used for and what are its elements?

What are the inclusion criteria for stroke lysis?
- Clinical diagnosis of ischemic stroke causing measurable neurologic deficit
- Onset of symptoms <4.5 hours before beginning treatment;
- Age ≥18 years
What is the dose of tPA for stroke lysis?
0.9mg/kg alteplase IV (maximum 90mg) over 60 minutes (10% given as a bolus)
What is the NNT to obtain functional independence for thrombolysis in ischaemic stroke?
10 - 13 depending on measure of “functional independence 0-1 vs 0-2.
What is the modified Rankin Score?

What is the number needed to harm (NNTH) for patients treated with thrombolysis in ischaemic stroke?
sICH - 42
Death - 122
What are the indications for GTN infusion in STEMI?
- Ischaemic pain not responsive to opiates
- Severe hypertension
- Cardiogenic APO with HTN
What are the indications for thrombolysis in STEMI?
Indications:
- PCI not available within 90mins of first medical contact AND
- All patients (without contraindications) who present within 12 hours of symptom onset of STEMI.
- Patients who present more than 12 hours after symptom onset may be considered however in selected cases when:
- There are ongoing symptoms
- There is ongoing electrical and /or hemodynamic (cardiogenic shock) instability.
NB: The ideal treatment for all STEMIs is acute PCI or in some cases emergency CABGs
What are the absolute and relative contrindications to thrombolysis (PE and STEMI)?

List ten causes of non-MI tropinaemia (cardiac and non-cardiac).
Cardiac:
- CHF
- Cardiac contusion or electrical injury (defib/electrocution)
- Tachy/bradyarrhythmias
- Kawasaki’s disease
- Takotsubo’s disease (stress cardiomyopathy)
Non-cardiac:
- PE
- Aortic dissection
- Sepsis
- >30% BSA burns
- Hypoxia
- ICH/SAH
- Renal failure
- Extreme exertion
List the STEMI criteria.
- >20mins of typical ischaemic chest pain
- Persistent (>20mins) ECG changes in >= 2 contiguous leads of:
- >2.5mm STE in V2-V3 (males < 40y)
- >2.0mm STE in V2-V3 (males > 40y
- >1.5mm STE in V2-V3 (females)
- >1mm in all other leads
- LBBB new or which meets Sgarbossa Criteria
What are the recommended timeframes for patients with confirmed ACS (STEMI or NSTEACS)?
- STEMI
- Very high-risk NSTEACS
- High risk NSTEACS
- Intermediate risk NSTEACS
- Emergent -> activate cath lab
- PCI <2h
- PCI < 24h
- PCI <72h
What are the features of Very High Risk NSTEACS?
- Haemodynamic instability:
- Heart failure/ cardiogenic shock
- Mechanical complications of myocardial infarction
- Life-threatening arrhythmias or cardiac arrest
- Recurrent or ongoing ischaemia (e.g. chest pain refractory to medical treatment) or
- recurrent dynamic ST segment and/or T wave changes, particularly with:
- de Winter T wave changes
- Wellens syndrome (or LMCA syndrome)
- posterior MI
What targets should be aimed for when utilising an MTP?
- Temp >35
- Calcium >1.1
- pH > 7.2
- Lactate < 4
- Platelets >50
- INR < 1.5
- APTT/PT <1.5 normal
- Fibrinogen > 1
- BE < -6
What are PESI and Simplified PESI?
What do they predict?
What are the features that suggest poorer outcomes in patients w/ PE?
PE Severity Index (11 clinical criteria)
Simplified PE Severity Index (6 clinical criteria)
They predict the risk of death at 30days. In sPESI, any one criteria increases the risk from 1.1% to 8.9%.
sPESI:
- Age > 80
- History of cancer
- History of cardiopulmonary disease
- HR > 110
- SBP < 100
- SaO2 < 90%
PESI is a weighted system and also includes:
- Gender
- RR > 30
- T < 36
- ALOC
What electrolyte imbalances are most common in re-feeding syndrome?
Give three effects of each of these imbalances.

List ten clinical indications (hx, exam or lab) for medical admission in patients with Eating Disorders.
- BMI < 12
- Weight loss 1kg/wk over multiple weeks
- Grossly inadequate nutritional intake <1000cal/day
- High risk of re-feeding syndrome, eg:
- SBP < 80mmHg
- Postural SBP drop > 10mmHg
- HR < 40 or > 120
- Postural HR inc > 20bpm
- T < 35degs
- Any arrhythmia (QTc prolongation, non-specific ST or T-wave changes)
- BSL < 2.5
- Na < 125
- K < 3.0
- Mg < 0.7
- PO4 < 0.8
- eGFR < 60
- Alb < 30
- Neutrophils < 1.0
- Markedly elevated ALT/AST > 500
*


