Schizophrenia Spectrum and other Psychotic Disorders Flashcards
Schizophrenia
- Characterized by broad spectrum of cognitive and emotional dysfunctions
- Disruptions in almost every aspect of daily functioning
- Full recovery is rare
Dementia Praecox and Other Early Conceptualizations
- Haslam and Pinel (early 1800s): wrote about what we now call “schizophrenia”
- Morel: “demence precoce” (means early/premature loss of mind in French)
-
Kraepelin
- “Dementia praecox”
- First to combine symptoms of catatonia (alternating immobility excited agitation), hebephrenia (silly and immature emotionality) and paranoia (delusions of grandeur or persecution). They are included under then term “Dementia praecox”
- Distinguished from manic-depressive disorder
-
Bleuler: introduced the term “schizophrenia”
- “Split mind” associated with splitting of basic functions of personality
Individuals with schizophrenia have varying symptoms as well as varying causes
What are the problems associated with schizophrenia?
- Thought
- Perception
- Memory
- Affect
- Attention
- Sensory processing
- Motor behaviour
- Life functioning
Schizophrenia DSM-5 Diagnostic Criteria
- A. Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated). At least one of those must be 1, 2, or 3:
- Delusions
- Hallucinations
- Disorganized speech (e.g., frequent derailment or incoherence)
- Grossly disorganized or catatonic behaviour
- Negative symptoms (i.e., diminished emotional express or avolition)
- B. For a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or self-care, is markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, there is failure to achieve expected level of interpersonal, academic, or occupational functioning)
- C. Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or by two or more symptoms listed in Criterion A in an attenuated form (e.g., odd beliefs, unusual perceptual experiences)
- D. Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out
- E. Disturbance not attributable to the physiological effects of a substance or another medical condition
- F. If there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations, in addition to the other required symptoms of schizophrenia, are also present for at least 1 month
- Specify if: with catatonia
Psychotic behaviour:
has been used to characterise many unusual behaviours, although in its strictest sense it usually involves delusions and and/or hallucinations
Schizophrenia: The Clinical Picture
- What does someone with schizophrenia look like?
- Groups of symptoms
- Are many “clinical pictures”
- Is violence an issue? Although people with schizophrenia are more likely to commit acts of violence than the general population, they are less likely to be violent compared to people with substance abuse and personality disorders
- Groups of symptoms:
- Positive
- Negative
- Disorganized
- Cognitive
- Positive symptoms
- Negative symptoms
- Disorganized symptoms
- Cognitive Symptoms
- Positive symptoms: generally refer to symptoms around distorted reality
- Negative symptoms: involve deficits in normal behaviour in such areas such as speech, blunted affect (lack of emotional reactivity) and motivation
- Disorganized symptoms: include rambling speech, erratic behaviour and inappropriate affect (e.g. smiling when upset)
- Cognitive Symptoms: Impairments in the ability to attend to, process, and retrieve information
% of people with schizophrenia who experience hallucinations, delusions or both
Between 50% and 70%
Positive Symptoms : Delusions
- Motivational view
- Deficit view
- Delusion: disorder of thought content
- Very common
- Has been called “the basic characteristic of madness”
- Common types:
- Control
- Thought insertion
- Thought withdrawal
- Thought broadcasting
- Persecution
- Reference
- Grandeur
- Body changes
- Uncommon delusions
- Capgras syndrome (imposter)
- Cotard’s syndrome (person is dead)
- How to understand delusions?
- Motivational view of delusions would look at beliefs as attempts to deal with and relieve anxiety and distress
- Deficit view of delusion sees these beliefs resulting from brain dysfunction that creates these disordered cognitions or perceptions
Positive Symptoms: Hallucinations
- Hallucinations are the experience of sensory events without any input from the surrounding environment
- Can involve any sensory system, but auditory most common
- Running commentary, accusations
- Most often voices of people they know in real life, and/or attributed to figures such as God or the devil
- How to understand auditory hallucinations?
- Possible that auditory hallucinations are a person’s own thoughts about thinking (or metacognitions) that they mistake for hearing someone else’s voice which leads to worrying about having these thoughts and worrying about worrying (meta-worry)
- This theory is supported by research that used single photon emission computed tomography (SPECT) in men with schizophrenia and found that when these individuals had auditory verbal hallucinations, the area that is most active in the brain is Broca’s area (involved in speech production, rather than language comprehension, which is Wernicke’s area)
Negative Symptoms
- Aprox 25% of people with schizophrenia display these symptoms
- “Pathological deficits”
- Avolition (apathy) little interest in performing day-to-day functions
- Alogia (relative absence of speech)
- Anhedonia (lack of pleasure)
- Affective flattening (do not show expected emotions, but may be responding to emotions on the inside)
- Studies suggest that emotional expression may be one way to identify potential schizophrenia in children
Disorganized Symptoms: Disorganized Speech
- Examples of disorganized speech: Loose associations or derailment
- Letter to Queen Beatrix
- Tangentiality (going off on a tangent instead of answering a specific question) and circumstantiality
- Neologisms (made up words)
- Clanging (rhyming speech)
Disorganized Symptoms: Inappropriate Affect and Disorganized Behaviour
- Diagnostic criteria for catatonia associated with another mental disorder (catatonia specifier)
- Inappropriate affect
Diagnostic criteria for catatonia associated with another mental disorder (catatonia specifier)
- A. The clinical picture is dominated by three or more of the following symptoms:
- Stupor (no psychomotor activity, not actively related to environment)
- Catalepsy (passive induction of a posture held against gravity)
- Waxy flexibility (slight, even resistance to positioning by examiner)
- Mutism (no or very little verbal response)
- Negativism (opposition or no response to instructions or external stimuli)
- Posturing (spontaneous and active maintenance of a posture against gravity)
- Mannerism (odd, circumstantial caricature of normal actions)
- Stereotypy (repetitive, abnormally frequent non-goal-directed movements)
- Agitation, not influenced by external stimuli
- Grimacing
- Echolalia (mimicking another’s speech)
- Echopraxia (mimicking another’s movements)
Cognitive Symptoms
- Impairments in the ability to attend to, process, and retrieve information
- Include deficits in:
- Early stages of information processing (e.g., attention, concentration)
- Encoding and storage (e.g., speed of information processing and memory)
- Complex, higher order skills (e.g., executive functions such as abstraction, planning, and problem solving)
Schizophrenia: Characteristics
- Lifetime prevalence: 0.3% - 0.7%
- No sex differences in prevalence, but are differences in age of onset and prognosis
- Relationship to SES:
- Found at all levels of SES but most commonly in lower SES
- Is it the stress of poverty that causes the disorder, or the disorder that causes individuals to fall from higher SES (“downward drift” theory)?
- Marital status:
- 3% divorced/separated, 2% single, 1% married
- Age of onset (associated with prognosis):
- Males: 18 – 25
- Females: 29 – 35
- Causes significant disability, high financial costs
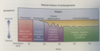
Schizophrenia: Development and Course
- Onset: late adolescence, early adulthood
- Some features seen in children
- Phases:
- Premorbid (before the psychotic episode)
- Prodromal (a 1-2 year period before the serious symptoms occur but when less severe yet unusual behaviour start to show themselves)
- Active
- Residual
- Treatment can aid improvement, but typical pattern is relapse and recovery
- Prognosis is poor
Research areas to find the cause of schizophrenia
- The possible genes involved in schizophrenia
- The chemical action of the drugs that help many people with the disorder
- Abnormalities in the working of brains of people with schizophrenia
- Environmental risk factors that may precipitate the onset of the symptoms
Other
- Women with schizophrenia seem to have more favourable outcomes than men
- Up to 85% of people who develop schizophrenia go through a prodromal stage, a 1-2 year period before the serious symptoms occur but when less severe yet unusual behaviour start to show themselves (some people have sudden onset of schizophrenia), the same as schizotypal personality disorder
- May be evidence of the development of schizophrenia in early childhood with symptoms of mild physical abnormalities, poor motor coordination and mild cognitive and social problems (called premorbid)
Natural history of schizophrenia
Culture
Schizophrenia is a universal cultural phenomenon although the course and outcome vary from culture to culture
Biological Aetiology
Genetics and family studies
- Genes are responsible for making some individuals vulnerable to schizophrenia
- Research has shown that families that have a member with schizophrenia are at risk not just for schizophrenia alone but for a spectrum of psychotic disorders related to schizophrenia
- There is a 48% chance of developing schizophrenia if an identical twin has the disorder, 17% for fraternal twins
- There is a 17% chance you will develop schizophrenia if your parent has the disorder
- Good home environments reduce the risk of schizophrenia
- Eye-tracking deficit and cognitive deficits in families may be endophenotypes for schizophrenia
Biological Aetiology
Neurobiological influences
- Dopamine hypothesis
- When drugs are administered that are known to increase dopamine (agonists), there is an increase in schizophrenic behaviour; when drugs that are known to decrease dopamine, (antagonists) such as neuroleptics or antipsychotics are used, schizophrenic symptoms tend to diminish.
- Taking these observations together, researchers theorised that schizophrenia in some people was attributable to excessive dopamine activity
- Evidence that contradicts the dopamine hypothesis
- A significant number of people with schizophrenia are not helped by dopamine antagonists
- Although neuroleptics block the reception of dopamine quite quickly, the relevant symptoms subside only after several days or weeks, more slowly than we would expect
- These drugs are only partly helpful in reducing negatives symptoms (for example, flat affect or anhedonia) of schizophrenia
- Evidence now points to at least three specific neurochemical abnormalities that simultaneously effect the brains of people with schizophrenia
Biological Aetiology
Abnormal brain function
- Adults with schizophrenia show deficits in their ability to perform certain tasks and to attend during reaction time exercises
- Evidence in ventricle enlargement in some people with schizophrenia (more common in men and ventricles seem to enlarge in proportion to age and duration of schizophrenia).
- Ventricle size itself may not be a problem, but the dilation of the ventricles indicates that adjacent parts of the brain either have not developed fully or have atrophied, thus allowing the ventricles to become larger.
- Enlargement of ventricles may be related to susceptibility of schizophrenia.
- People with schizophrenia often have hypofrontality, which is when the frontal lobes are less active. Follow up studies show hyperfrontality (too much activity), indicating the dysfunction is reliable, but hyperfrontality displays itself differently in different people
Biological Aetiology
Prenatal and perinatal influences
- Fetal exposure to viral infection (influenza in the second trimester), pregnancy complications and delivery complications are among the environmental influences that seem to affect whether or not someone develops schizophrenia
Marijuana and Schizophrenia
Possible correlation between early and chronic use of marijuana and development of schizophrenia
Psychological and Social Influences
- Stress
- Schizophrenogenic mother
- Double bind communication
- Expressed emotion
-
Stress
- The symptoms of schizophrenia seem to become worse as a result of stressful life experiences
- Schizophrenogenic mother was a term used to describe a mother whose cold, dominant and rejecting nature was thought to cause schizophrenia in her children (no longer supported)
- Double bind communication was used to portray a communication style in parents that produced conflicting messages (no longer supported)
-
Expressed emotion
- If high levels of criticism, hostility, and emotional over-involvement in families of people with schizophrenia were high, patients tended to relapse
- Schizophrenia patients who live in a family with high expressed emotion are 3.7X more likely to relapse than those in a family with low expressed emotion
- Although, there seem to be cultural variations (what appears to be over-involvement in one culture may be viewed as supportive in other cultures)
Is What We Call “Schizophrenia” Actually Multiple Disorders?
- Question that has been debated for many years -> wide variety of symptom presentation
- Recent genetic research now suggesting that schizophrenia is actually multiple genetically distinct disorders
- Groups of interacting gene clusters create extremely high risk (70-100%)
Treatment of Schizophrenia: Biological Interventions
- Treatment usually begins with one of the neuroleptic drugs available which are typically combined with a variety of psychosocial treatments to reduce relapse, compensate for skills deficits and improve cooperation for taking the medications
- Early historical treatments: psychosurgery, insulin coma therapy, ECT
- Antipsychotic medications
-
Neuroleptics (conventional or first-generation psychotics),
- Haldol
- Thorazine
-
Atypical/second-generation antipsychotics, these drugs hold promise for helping those who were previously unresponsive to medications
- Risperidone
- Olanzapine
-
Neuroleptics (conventional or first-generation psychotics),
- Noncompliance a constant issue
- Some factors include negative doctor-patient relationships, cost of medication and poor social support and unpleasant side effects
- Unpleasant side effects
- Extrapyramidal symptoms (e.g., akinesia, tardive dyskinesia which can be irreversible)
- Transcranial magnetic stimulation
- Can be effective in reducing auditory hallucinations, but its effects last less than a month
Psychosocial Interventions for Schizophrenia
- Symptom and medication management
- Institutionalization and deinstitutionalization
- Revolving door syndrome
- Social skills interventions
- Identify symptoms of relapse
- Family interventions
- Vocational rehabilitation
- Assertive community treatment
- Prevention!
Classifying Psychotic Disorders
- Schizotypal (Personality) Disorder
- Delusional disorder
- Brief psychotic disorder
- Schizophreniform disorder
- Schizophrenia
- Schizoaffective disorder
- Substance/Medication-induced psychotic disorder
- Psychotic disorder due to another medical condition
- Catatonia associated with another mental disorder
- Catatonic disorder due to another medical condition
- Unspecified catatonia
- Other specified schizophrenia spectrum and other psychotic disorder
- Unspecified schizophrenia spectrum and other psychotic disorder
Schizophreniform Disorder Diagnostic Criteria
(experiencing schizophrenia for a few months only and then resuming normal lives)
- A. Same as Criterion A for schizophrenia
- B. Episode of the disorder lasts at least 1 month but less than 6 months
- When diagnosis must be made without waiting for recovery, should be qualified as “provisional”
- C. Schizoaffective disorder and depressive or bipolar disorder have been ruled out
- D. Disturbance not attributable to physiological effects of a substance or another medical condition
- Specify if:
- With good prognostic features (e.g., at least two of the following: onset of prominent psychotic symptoms within 4 weeks of the first noticeable change in usual behaviour or functioning; confusion or perplexity; good premorbid social and occupational functioning; absence of blunted or flat affect)
- Without good prognostic features (absence of two or more of above features)
- With catatonia
Schizophreniform Disorder Characteristics
- Incidence is low, perhaps five-fold less than that of schizophrenia
- Development of disorder similar to that of schizophrenia
- 1/3 will fully recover, 2/3 will eventually receive a diagnosis of schizophrenia or schizoaffective disorder
Schizoaffective Disorder Diagnostic Criteria
- A. An uninterrupted period of illness during which there is a major mood episode concurrent with Criterion A of schizophrenia
- B. Delusions or hallucinations for 2 or more weeks in the absence of a major mood episode during the lifetime duration of the illness
- C. Symptoms that meet criteria for a major mood episode are present for the majority of the total duration of the active and residual portions of the illness
- D. Disturbance not attributable to effects of substance or another medical condition
- Specify type:
- Bipolar type: If manic episode is part of the presentation
- Depressive type: If only major depressive episodes are part of the presentation
- Specify if with catatonia
Features of Schizoaffective Disorder
- Lifetime prevalence: 0.3% (1/3 as common as schizophrenia)
- Onset is typically in early adulthood
- Prognosis is better than for schizophrenia, worse than that for mood disorders
- Expression of psychotic symptoms across the lifespan is variable
- Depressive or manic symptoms can occur before the onset of psychosis, during acute psychotic episodes, during residual periods, and after cessation of psychosis
Delusional Disorder Diagnostic Criteria
- A. Presence of one or more delusions with a duration of 1 month or longer
- B. Criterion A for schizophrenia has never been met
- C. Apart from the impact of the delusion(s) or its ramifications, functioning is not markedly impaired, and behaviour is not obviously bizarre or odd
- D. If manic or major depressive episodes have occurred, these have been brief relative to the duration of the delusional periods
- E. Disturbance is not attributable to the physiological effects of a substance or another medical condition, not better explained by another mental disorder
Characteristics of Delusional Disorder
- Lifetime prevalence: 0.2%
- No major gender differences (seems to affect 55% females and 45% males)
- Like many with schizophrenia, people with delusional disorder experience delusions
- Other than this, however, they behave very normally
- Behaviour does not show gross disorganization and performance deficiencies characteristic of schizophrenia
- General behavioral deterioration rarely occurs with this disorder
Delusional Disorder: Types
Delusional disorder delusions are different from schizophrenic delusions in that the imagined events could be happening (are plausible) but aren’t. In schizophrenia the imagined events aren’t possible (e.g. believing your brainwaves broadcast to other people around the world).
- Specify Type:
- Erotomanic Type (irrational belief that one is loved by another person, usually of higher status)
- Grandiose Type (believing in one’s own inflated worth, power, knowledge, identity or special relationship to a deity or famous person)
- Jealous Type (believes a sexual partner is unfaithful)
- Persecutory Type (believing oneself or someone close is being malevolently treated in some way)
- Somatic Type (person feels afflicted by a physical defect or general medical condition)
- Mixed Type
- Unspecified Type
- Specify if with bizarre content
- If delusions are clearly implausible, not understandable, and not derived from ordinary life experiences
Brief Psychotic Disorder Diagnostic Criteria
- A. Same as schizophrenia Criterion A
- B. Duration of an episode of the disturbance is at least 1 day but less than 1 month, with eventual full return of premorbid level of functioning
- C. Disturbance not better accounted for by a major depressive or bipolar disorder with psychotic features or another psychotic disorder or catatonia, not attributable to physiological effects of a substance or another medical condition
- Specify with:
- With marked stressor(s) (brief reactive psychosis)
- Without marked stressor(s)
- With postpartum onset
Brief Psychotic Disorder Characteristics
- May account for 9% of cases of first-onset psychosis
- Average age of onset: mid-30’s
- Prognosis is excellent despite high rates of relapse
- Increased risk of suicide, particularly during acute episode
Other
Attenuated psychosis syndrome is a proposed new psychotic disorder that includes people who may have some symptoms of schizophrenia but are aware of the troubling and bizarre nature of these symptoms (good insight). They can be at high risk for developing schizophrenia so may be good candidates for early intervention in an effort to stop the symptoms from worsening
Shared psychotic disorder was included in previous version of DSM , which was a condition in which an individual develops delusions simply as a result of a close relationship with a delusional individual. In DSM 5 this type of delusion is included under delusional disorder with a specifier to indicate the delusion is shared.
Other
- The greatest risk of having schizophrenia is in those who have an identical or fraternal twin with schizophrenia. Any relative with schizophrenia will make your chances of developing the disorder higher than those of the general population.*
- Raised in a home other than that of their biological parents, adopted children of parents with schizophrenia have a higher chance of having the disorder themselves. Children of people with schizophrenia adopted into families without schizophrenia have a higher than average chance of having schizophrenia*
- The likelihood of a child having schizophrenia is influenced by the severity of the parents disorder. One may inherit a predisposition for general schizophrenia that is the same or different from that of the parent.*
- Setting up an elaborate token economy in which patients are fined for disruptive or inappropriate behaviour and rewarded for appropriate behaviour is beneficial in hospitals*
- In social skills training clinicians attempt to reteach such behaviours such as basic conversation, assertiveness and relationship building to people with schizophrenia*
- Aside from social skills training, two psychosocial treatments for schizophrenia family intervention (teaching family members to be supportive) and vocational rehabilitation (teaching meaningful jobs), may be helpful*
- Recent studies indicate that the relationship of the neurotransmitters dopamine and serotonin may explain some positive symptoms of schizophrenia*
- Because antipsychotic mediations may cause serious side effects, some patients stop taking them. One serious side effect is called extrapyramidal symptoms, which may include parkinsonian symptoms*
- Difficult cases of schizophrenia seem to improve with a serotonin and dopamine antagonist called olanzapine*


