Schizophrenia 1.5.1 Flashcards
What are some negative symptoms of schizophrenia?
- Emotional withdrawal
- Social withdrawal
- Lack of pleasure/ motivation
- Poor grooming/ hygiene- unkempt, BO
- No goal- directed behaviour- amotivation
- Alogia- talks little, uses few words
- Apathy
What are some positive symptoms of schizophrenia?
- Delusions- neighbour poisoning him
- Hallucinations- insect sensation
- Disorganised speech- “hard to comprehend”
- Disorganised behavior
- Agitation
- Insomnia
How do we diagnosis schizophrenia?
- There is no clear test to diagnose schizophrenia
- Mental state examination (interview patient)
- History from patient/family/friends
- MRI, CT scan and blood tests are generally used to rule out physical illness
- Drug testing - to exclude drug induced psychosis
- DSM 5 Criterion: TWO or more symptoms present for a significant portion of time during a 1 month period including delusions, hallucinations, disorganised speech (incoherence), grossly disorganised, negative symptoms (avolition, diminished emotional expression)
- Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms
How do you get the positive symptoms?
- an excess of dopamine in the mesolimbic pathway
- dopamine travels from the midbrain tegmental area to the nucleus accumbens
- increased activity in this pathway
How do you get negative symptoms?
- due to insufficient dopamine activity in mesocorticol pathway
- decreased activity in the pathway that goes from the midbrain to the prefrontal lobe cortex* can cause
- apathy
- withdrawal
- lack of motivation & pleasure
What causes extrapyrimidal SE of antipsychotic drugs?
- the pathway from the substantia nigra to the striatum is involved in the coordination of body movements
- inhibition of this pathway causes EPSE
How do you get elevated serum prolactin levels?
- the pathway from the hypothalamus to the pituitary
- D2 stimulation –> inhibits the release of prolactin
- inhibition of this pathway leads to elevated serum prolactin levels
What is the dopamine theory of schizophrenia?
- most antipsychotic drugs block dopamine receptors
- psychotic symptoms can be induced by drugs that increase dopaminergic activity anti-parkinsonian agents
- single positive electron tomography ligand scans show an increase in D2 receptors in nucleus accumbens of schizophrenia patients
Which drugs mimic positive, negative & cognitive symptoms of schizophrenia?
- phencyclidine
- ketamine
- they are glutamate NMDA receptor antagonists
Which drugs mimic positive symptoms of schizophrenia? How?
- amphetamine, methamphetimine
- psilocybin, LSD
- phencyclidine, ketamine
- they release dopamine & inhibit its reuptake
Which drugs are good in treating negative symptoms?
- 5HT2A receptor antagonists produced by SGAs
Which drugs are good in treating positive symptoms of schizophrenia?
Positive symptoms respond well to D2 receptor antagonism produced by FGAs & SGAs
Why does it take 1-3 weeks for antipsychotic agents to have therapeutic effect?
- there are 3 time-dependent changes in dopamine neurotransmission
- immediate effects: an increase in dopamine synthesis, release and metabolism but NO therapeutic effect
- prolonged effects (1-3wks): depolarization blockade–> reduced dopamine release from mesolimbic and nigrostriatal neurons –> alleviate the positive symptoms of schizophrenia while causing EPSs
- extended prolonged effects: dopamine receptor up-regulation and supersensitivity to dopamine agonists
- —>>may contribute to the development of a delayed type of EPS called tardive dyskinesia
What are the FGAs used to treat antipsychotics?
- chlorpromazine
- haloperidol
- droperidol
- flupentixol
- periciazine
- zuclopenthixol
What are the SGAs used to treat schizophrenia?
- clozapine
- olanzapine
- quetiapine
- risperidone
- paliperidone
- amisulpride
- aripiprazole
- asenapine
- ziprasidone
- lurasidone
- brexipiprazole
What is the difference between FGAs & SGAs?
- incidence of EPSE
- efficacy in treatment- resistant groups of patients
- efficacy against negative symptoms
- FGAs not effective
- receptor selectivity
- pharmacological properties
- FGAs- positive sxs
- SGAs- postive & negative sxs
What is the MOA of antipsychotics?
- D2 receptor antagonism is essential
- 5HT2A receptor antagonism enhances/ complements D2 receptor antagonism
- 5HT2A receptor antagonism by SGAs
What happens in the mesocortical pathway?
- SGAs
- 5-HT2 receptors inhibit presynaptic dopamine release
- by blocking these receptors this may increase dopamine release in this pathways – this may alleviate the –ve Sx
- 5HT2A antagonist enhance / complements action of D2 antagonist to reduce positive symptoms
- may protect against EPS by preserving nigrostriatal DA activity
- also alleviate anxiety and insomnia in schizophrenia
What happens in the mesolimbic pathway?
- FGAs
- dopamine D2 receptor blockers inhibit effect of dopamine in mesolimbic pathways thereby reducing the positive Sx
- Affinity for D2 receptors cause of EPS (extrapyramidal side- effects)
- Affinity for D2 receptors is strongly correlated with alleviation of positive symptoms and cause of EPS (extrapyramidal side-effects)
- FGAs alleviate positive symptoms of schizophrenia (delusions, hallucinations & disturbed thinking)
- FGAs are quite ineffective in treating negative & cognitive symptoms and EPS may become intolerable
What are therapeutic effects of SGAs?
- alleviation of negative & cognitive symptoms as well as positive symptoms
- lower incidence of EPS and generally better tolerated
- SGAs are superior to FGAs interact with 5-HT2A and D2 receptors
- Antagonism of D3, D4 and other receptors may also contribute to the favourable clinical profile of SGAs
What are some ADV of antipsychotics?
- blockade of a1 receptors
- hypotension, reflex tachycardia
- blockade of histamine H1-receptor
- sedation & weight gain
- blockade of 5HT2C & H1 receptors
- weight gain
- anticholinergic effects
- blurred vision, dry mouth, constipation, urinary
retention
- ADV due to immune reaction
- hypersensitivity, dermatitis, rashes, photosensitivity, urticaria
- ADV due to individual drug
- clozapine cause agranulocytosis -neutropenia, bone marrow depression
- idiosyncratic rxn
- neuroleptic malignant syndrome
What are some EPSE?
- acute dystonia
- involuntary muscle spasms
- hyperextension of trunk, neck
- arching of back
- lock jaw
- akathesia
- muscle quivering, restlessness, inability to sit still
- parkinsonism
- neuroleptic malignant syndrome
- fever, encephalopathy, vtals unstable, elevated enzymes, rigidity of muscles
- dantrolene tx
Chlorpromazine as a FGA…
- low potency antipsychotic
- EPS can become troublesome
- prominent sedation, hypotension & antimuscarinic effects
- can cause obstructive jaundice and photosensitivity leading to sunburn
- useful when sedation is desired
- administered orally, IV or IM
Flupenthixol decanoate as a FGA
- depot preparation that can be administered IM every 2-4 weeks
- Minimal sedation & hypotension, but prominent EPS
Haloperidol as a FGA…
- high potency antipsychotic
- EPS is a main problem
- Favoured when sedation, hypotension, and antimuscarinic effects are undesirable (elderly patients)
- Administered orally or IM
What are long acting depot injections used for?
- for patients who don’t reliably take oral antipsychotic medication
What are clinical uses of SGAs?
- Treatment of acute and chronic psychoses (e.g. schizophrenia)
- Acute mania (olanzapine, quetiapine, risperidone)
- Organic psychoses (e.g. dementia- associated agitation)
- Severe behavioural disorders in children
Olanzapine as a SGA…
- Does not cause agranulocytosis
- Convulsions can occur
- Side-effects include: sedation, weight gain, impaired glucose regulation, hypotension and antimuscarinic effects
- widely prescribed
Risperidone as a SGA…
- positive, negative, cognitive symptoms of schizchoprenia
- above therapeutic doses (>4-6mg/day), can produce EPS
- Does not cause agranulocytosis
- Antimuscarinic effects are minimal
- Side-effects include: mild sedation, mild weight gain & impaired glucose regulation, hypotension, hyperprolactinaemia
- widely prescribed
Aripiprazole as a SGA…
- Improve positive symptoms and reduce relapse rates after an acute episode
- Does not cause agranulocytosis
- Side-effects include: sedation, weight gain, impaired glucose regulation, hypotension and antimuscarinic effects
- Precautions:
- Recent history of MI, unstable heart
- Treatment with CYP3A4
- Poor metaboliser - CYP2D6
- indicated for schizophrenia & BPAD as monotherapy
Quetiapine as a SGA…
- can treat positive, negative & cognitive symptoms without producing EPS
- Does not cause agranulocytosis
- Side-effects include sedation, dry mouth, constipation, hypotension, mild weight gain & impaired glucose regulation
- good for schizophrenia
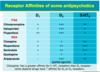
Receptor affinities for antipsychotics, 5HT2, D1, D2