S8) Functional Anatomy of the Eye Flashcards
Describe the structure of the orbital cavity
The orbital cavity is pyramidal shaped with its apex pointing posteriorly and base anteriorly

Identify the different boundaries of the orbit
- Roof (superior wall)
- Floor (inferior wall)
- Medial wall
- Lateral wall
- Apex
- Base
Describe the structures forming the roof of the orbital cavity
- The roof is formed by the frontal bone and the lesser wing of the sphenoid
- The frontal bone separates the orbit from the anterior cranial fossa

Describe the structures forming the floor of the orbital cavity
- The floor is formed by the maxilla, palatine and zygomatic bones
- The maxilla separates the orbit from the underlying maxillary sinus

Describe the structures forming the medial wall of the orbital cavity
- The medial wall is formed by the ethmoid, maxilla, lacrimal and sphenoid bones
- The ethmoid bone separates the orbit from the ethmoid sinus

Describe the structures forming the lateral wall of the orbital cavity
The lateral wall is formed by the zygomatic bone and greater wing of the sphenoid

Describe the structures forming the apex and base of the orbital cavity
- The apex is located at the opening to the optic canal (optic foramen)
- The base (aka orbital rim) opens out into the face, and is bounded by the eyelids

The orbital cavity has 4 bony walls. Identify them.
- Base = Tough orbital rim
- Medial wall = Ethmoid bone
- Floor = Maxillary bone
- Roof = Orbital plates of frontal bone

Identify 3 important anatomical relations of the orbital cavity
- Paranasal air sinuses (maxillary and ethmoid)
- Nasal cavity
- Anterior cranial fossa

Identify two important implications of the anatomical relations of the orbital cavity
- Orbital surgery e.g. lobotomy
- Spread of infection (into and out from orbit)
- Orbital trauma
Identify the weakest parts of the orbital cavity and explain why they are most easily fractured
Medial wall and floor of the orbit as they are thinner and contain air cavities ( they aren’t chunky bones) .: most vulnerable to fracture when there is direct impact to the front of the eye by a ball/ fist.
What is an orbital blowout fracture?
An orbital blowout fracture is a fracture leading to the partial herniation of the orbital contents through the the orbital wall due to blunt force trauma to the eye

How does an orbital blowout fracture occur?
- Direct impact to front of eye e.g. ball/fist
- Leads to sudden increase in intra-orbital pressure from traume to the eye/ orbit
- Results in retropulsion of contents in the orbit e.g. eyeball
- This fractures floor of orbit (maxilla) → orbital blow-out fracture

How does an orbital blow out fracture present?
- Periorbital swelling (painful)
- Double vision (especially on vertical gaze)
- Impaired vision
- Anaesthesia over affected cheek (infraorbital nerve damage)

How do orbital blow out fractures occur?
Sudden increase in intra-orbital pressure from retropulsion of eye ball e.g. by fist/ball fractures floor of orbit

What is the result of an orbital blow out fracture?
- Orbital contents and blood can prolapse into maxillary and ethmoid sinuses respectively
- The fracture site can ‘trap’ structures e.g. muscles and soft tissue such as the extra orbital muscle located near floor or orbit

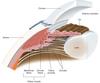
Look at the images and describe what is seen in the orbital blow out fracture?


In orbital blow out fractures, the mastoid is often fractured. Although the medial wall of the orbit made by the ethmoid bone is thinner than the floor of the orbit, what makes it stronger?
- presence of walled air cells (anterior, middle, posterior and ethmoidal air cells) act as buttresses + convey an added strength to the medial wall.

What risk is there with the presence of air ethmoidal air cells in relation to the orbit?
- air cells can be come infected (acute sinusitis) and due to their proximity to the orbit → infection can sometimes break through the thin lamina papyracea (part of ethmoid bone forming medial wall of the orbit) → .: track into the orbit → causing orbital cellulitis
Which nerve is at risk during an orbital blow out fracture?
- infra-orbital nerve (branch of Vb of trigeminal nerve)

What is the management for orbital blow-out fracture?

Three openings at its apex of the orbit transmitting nerves and blood vessels in and out.
Identify them

What structures are carried in the optic canal?

What structures are carried in the superior orbital fissure?