Rheumatology Flashcards
Common and chronic conditions (plus some potential rogue ones) to know
List common differentials for an acutely swollen joint
- Most important to rule out –> septic arthritis
- trauma & haemarthrosis
- bursitis
- tendinopathy
- reactive arthritis
- gout
- pseudogout
- enteropathic arthritis
Define gout
What is the pathophysiology?
Gout = crystal arthropathy resulting from excess uric acid leading to precipitation in joints and tissues.
Pathophysiology –> disorder of purine metabolism, uric acid is the breakdown product of purines and is predominantly excreted via the kidneys. Imbalance between production and excretion of uric acid leading to deposits in joints and soft tissues.
3 main mechanisms - increased production with increased cell turnover e.g. psoriasis, chemoT
Increased purine intake - seafood red meat alcohol
Decreased uric acid secretion e.g. furosemide, thiazides, AKI, CKD
Risk factors for gout?
Fuck My HOT And Chronic gout
Family history
Male
High purine diet/ hyperlipidaemia
Obesity
Thiazides
CKD/ CVD/ Chemotherapy / DBM
Presentation of gout
Rapid onset of pain - typically over 1 hour
Monoarticular - often 1st MTP joint (may affect wrists/ carpometacarpal joint/ knee/ ankle)
or oligoarticular (< 4 joints)
joint stiffness, swelling, erythema & warmth
effusion
Gout tophi - often on extensor surfaces - elbow, knee, achilles, helix of ear
FHx of gout
Examination features of gout
- warm red swollen
- considerable tenderness
- limited ROM
- Hard subcutaenous Tophi on extensors - elbow/ knees / achilles/ helix of ears

Investigations for Gout
- Gout is a clinical diagnosis but joint aspiration can be used to confirm it
Bedside:
- BM - Diabetes = RF
- Urine dip - for CKD (protein blood etc)
Bloods:
- FBC
- U& E –> check renal function
- LFTs –> premedication baseline
- Blood cultures –> exclude septicaemia
- Serum Uric acid –> taken 4-6 weeks after acute attack, normal serum uric acid does not exclude gout during an acute attack as plasma urate often falls.
- Serum Calcium
Imaging:
- USS –> more sensitive in Xray in detecting erosions, tophi and gout specific double contour sign
- Xray –> typically normal in acute episodes of gout. In Chronic gout:
- lytic lesions
- punched out erosions
- erosion with sclerotic borders
- joint space maintained
Special test:
- Joint arthocentesis –> gold standard investigation, exclude septic arthritis
- MCS of joint aspirate –> crystal microscopy will show needle shaped monosodium urate crystals, negatively birefringent of polarised light. No bacterial growth

Management of gout
Conservative:
- Rest, ice, elevation
- Weight loss
- Low purine diet
- Reduced alcohol consumption
Medical:
For acute episode:
- NSAID 1st line, Colchicine 2nd line, Steroid 3rd line
- NSAID CI in significant HD or renal impairment, then use oral colchicine
- notable SE colchicine is diarrhoea which is dose dependent.
- If NSAID and colchicine is CI then short course oral steroid or intraarticular steroid
For chronic management:
- urate lowering therapy usually started once initial attack has resolved to enable the patient to make the decision to start urate lowering therapy without any pain
- First line Allopurinol = xanthine oxidase inhibitor that prevents conversion of metabolites to uric acid
- colchicine cover considered for the first 6 months
- Caution with allopurinol in renal impairment
- Second line = Febuxostat (also xanthine oxidase inhibitor) considered if allopurinol is CI.
Define pseudogout
Pseudo gout = Microcrystal synovitis caused by the deposition of calcium pyrophosphate crystals in the synovium
What is the pathophysiology of pseudogout
What are the risk factors
- Pathophysiology:
- excess CPP production leads to supersaturation and crystal formation / deposition in the synovium. There is an inflammatory response to calcium in the synovium
- Risk factors: usually pseudogout is associated with increasing age therefore patients developing it at a younger age have a secondary condition:
- haemochromatosis
- hyperparathyroidism
- hypomagnesaemia
- familial CPPD disease (calcium pyrophosphate disease)
- acromegaly
- wilsons
- gout
Presentation of pseudogout
Asymmetrical arthropathy of larger peripheral joints
key risk factors of increasing age, family history, previous inury or surgery to the joint, metabolic disorders
often affects knee 50%, can affect the shoulders, elbows, wrists, hips, ankles and feet
sudden worsening of osteoarthritis and involvement of joints not commonly involved in OA e.g wrists and shoulders may suggest CPP arthritis
joint swelling
erythema
restricted ROM
with or without fever
Investigations for pseudogout
- Bedside: BM ( diabetes), Urine dipstick (kidney function)
- Bloods:
- FBC
- U&Es (kidney function)
- LFTs baseline premedication
- Blood cultures –> rule out septicaemia
- Serum calcium / bone profile (check for hyperparathyroidism)
- Serum urate
- Imaging:
- Xray –> chondrocalcinosis is the classical XR finding (pathognomonic of gout)
- Other XR changes similar to OA (LOSS) (Loss of joint space, osteophytes, subchondral sclerosis, subchondral cysts)
- Special tests:
- Synovial fluid analysis –> rhomboid shaped crystals positively birefringent in polarised light with no bacterial growth

Management of pseudogout
- Flares usually self resolve within a few weeks
- Conservative:
- ice packs, immobilisation, rest for first 48 hours
- Medical management:
- NSAID - naproxen first line
- colchicine - if NSAID CI
- Steroids PO or joint injection if no response to above
- Recurrent episodes may need prolonged colchicine
- Surgical:
- Joint washout in severe cases
Define reactive arthritis
Reactive arthritis - one of the group of seronegative spondyloarthropathies, arthritis occurring after an infection with “Sterile inflammation”.
Occurs several weeks following an infection with organisms that infect the urogenital or GI tract
Common organisms causing reactive arthritis?
- Urogenital infections –> chlaymidia, gonorrhoea, Ureaplasma urealyticum
- GI –> campylobacter jejuni, shigella, salmonella, yersinia, C diff
- Rare – >TB
Presentation of Reactive arthritis
Key: cant see, pee, or climb a tree
- Conjunctivitis
- urethritis
- acute monoarthritis
- Patients with clear history of preceding infection either diarrhoea or urethritis
- often 1- 4 weeks before onset of joint pain
- Peripheral asymmetrical oligoarthritis most common
- can cause monoarticular or polyarticular arthritis
- acutely hot swollen red painful joint
- worse in the morning
- axial arthritis –> inflammatory back pain, buttock pain, stiffness at rest, relieved by exercise
- enthesitis - often achilles
- dactylitis
Extraarticular manifestations:
- fever
- fatigue
- ocular –> bilateral conjunctivitis
- oral ulcers
- Skin –> circinate balanitis (inflammation of head of penis) and keratoderma blenorrhagica, erythema nodosum
- GI –> diarrhoea
- Urogenital –> urethritis & dysuria

Investigations : reactive arthritis
- Bedside:
- urine dipstick & urinalysis for source of infection
- Stool culture (often negative at onset of arthritis)
- urethral / cervical swab for STI screen
- Bloods:
- FBC
- U&E
- LFT
- CRP/ESR
- blood cultures - rule out septic arthritis
- STI screen - HIV/ hep/ syphilis
- ANA (should be -ve)
- RF (should be -ve)
- Imaging/ special test:
- Xray of pelvis –> asymmetric sacroilities or enthesitis of achilles tendon
- Joint aspiration to exclude septic arthritis, gout and pseudogout
Management : reactive arthritis
- Conservative: RICE
- Medical –> 1) indentify and eradicate underying infection, 2) NSAID& paracetamol, 3) Steroid PO or joint injection
- Medical if chronic ReA –> use DMARDs methotrexate or sulfasalazine
Often self limiting but up to 20% develop chronic arthritis
Key risk factors reactive arthritis
DDX reactive arthritis
Key risk factors: Male, HLA B27 +VE, preceding chlaymidia or GI infection
DDX:
Septic arthritis (key)
disseminated gonococcal infection
Gout
pseudogout
RA
SLE
Traumatic arthritis / haemarthrosis
Differential diagnosis for chronic joint pain
- Monoarthritis:
- OA
- Chronic tophaceous gout
- Polyarthritis:
- RA
- Ankylosing spondylitis
- psoriatic arthritis
- Systemic sclerosis
- SLE
- Sjogrens
- PMR
- Fibromyalgia
Define osteoarthritis
- Osteoarthritis is a chronic degenerative joint disorder caused by degeneration of the cartilage within a joint, leading to exposure of the underlying bone and bone - bone interaction. Leads to pain, stiffness and reduced function of the joint involved.
Risk factors for OA
- Age
- Female
- Fhx
- Physically demanding occupation or sport
- anything leading to altered joint loading –> hypermobility, osteoporosis, trauma within the joint e.g. fracture, meniscal or ligament tears
Presentation of OA (symptoms)
- Pain and stiffness within joints
- worsened by activity and weight bearing
- background ache at rest
- lasts less than 30 mins in the morning
- pain better with rest
- pain not present at night unless advanced
- often affects larger weight bearing joints : Hips, knees, SI joints, cervical spine
- Hands –> DIPs and 1st CMC joint (base of the thumb) & wrist
- often > 50 years
- slow onset over months - years
- functional difficulty
Signs of OA on examination?
- Check weight, height, calculate BMI
- Watch for gait abnormality and malalignment of the joints
- Look:
- joint swelling
- erythema
- bony swellings –> osteophytes
- effusion
- fixed flexion deformity at the knee or hip (+ve thomas test)
- Feel:
- crepitus
- limited ROM
- Effusion
- Joint line tenderness
- Move:
- assess ROM, both active and passive (will be reduced)
- crepitus felt
- assess for ligament laxity (may be a cause)
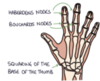
- Hand signs:
- Heberdens DIP
- Bouchards PIP
- Squaring of 1st CMC joint
- Weakened grip
- reduced ROM
Diagnosis of OA?
Diagnosis of OA is often a clinical diagnosis based of age, symptoms and examination findings. Clinical diagnosis is considered in a patient with a typical OA presentation:
Activity related joint pain
morning stiffness no longer than 30 mins
> 45 yrs











