Respiratory Tract Histology and Defence Mechanisms Flashcards
- Describe the respiratory epithelium as found in the trachea and bronchus. - Describe the change in epithelial pattern in the alveoli and relate this to gas exchange. - Describe the micro-anatomy of the wall of the respiratory tract and relate this to function. - Outline the nature of the secretions of the lung.
Describe the epithelial lining of the trachea.
Girthy ;)

What purpose and features of the nose and oropharnyx make it a useful component of the respiratory system?
- Filters large particles
- Warms & Humidifies air, prevents epithelium from drying out.
- Mucosal layer lined with different types of epithelial cells.
- Respiratory epithelium-based in aqueous viscous & sticky mucus to trap particles.
- Ciliated epithelium have a coordinated beat-mucocilary escalatory push material towards naso & oropharynx.
- Irritant particles stimulate irritant receptors and provoke sneezing & couging to remove material.
Describe the histological features of the conducting airways, from the nasal passages to the small bronchi.
Pseudostratified with 3 cell types:
- Ciliated epithelial cells - mucosillary escalatory.
- Goblet cells (secretory, non-ciliated).
- Basal cells (act as stem cells, may contribute to structure).
Describe the epithelial histology of the bronchioles.
- Epithelium changes to simple ciliated cuboidal
- Club (Clara) cells replacing goblet cells.
Briefly describe the componenents of the mucocillary escalator.

Which parasympathetic nerve can increase mucus secretion?
The vagus nerve (CN X)
What is CN II?
The Optic Nerve
Describe the features of the tract wall in different respiratory conducting zones.
Trachea & Primary Bronchi: Held open by C-shaped cartilage anterolaterally, smooth muscle (Trachealis) posteriorly.
Trachea: (generally 16-20) rings of cartilage.
Bronchi: cartilage plates, smooth muscle, blood vessels of systemic circulation (bronchial arteries).
Bronchioles: smooth muscle helical bands
Describe the epithelial lining of the trachea

Describe the histology of the olfactory epithelium.

Describe the histology of the bronchus.

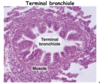
Describe the histology of the terminal bronchioles.
- They have no cartilage, glands.
Epithelial in initial portion is ciliated columnar, but then becomes cuboid with cilia.
- Final portion un-ciliated.
- Smooth muscle.
Outline the histological nature of the respiratory bronchioles.
- They have a low simple cuboidal epithelium and a thin coat of interlaced smooth muscle and elastic fibres.
- It has thin evaginations in its wall: 1st respiratory alveoli, where gaseous exchange can take place.
- Primary alveoli, thin-walled spaces with minimal diffusion distance to pulmonary capillaries.
- This is where gas exchange occurs.

Give some factual information about Type I pneumocytes.
- 95% of alveolar surface.
- Highly flattened.
Simple squamous epithelium.
Form occluding junctions with one another.
(Barrier to extracellular fluid into alveolus).
- Type I cells forms thin diffusion barrier - fused with pulmonary capillary endothelium - the blood-gas interface.
- Neighbouring alveoli interconnected by Pores of Kohn.
Give some factual information about Type II pneumocytes.
- less numerous; only about 5% of alveolar surface
- Cuboidal
- Capable of rapid cell division
- Dispersed among type I pneumocytes and form occluding junctions with them
- Produce surfactant - reduces surface tension, prevents alveoli from collapse.
Histologically distinguish between Type I and Type II pneumocytes.

Describe the spatial arrangements of Type I and Type II pneumocytes in the alveolar membrane.

Give some properties of the Type II pneumocyte alveolar cells.
- Type II cells are thicker & produce a fluid layer that lines alveoli.
- Fluid contains pulmonary surfactant in lamellar bodies.
- Reduces the surface tension within alveoli
- Interstitium contains reticular and elastic fibres, allowing for elasticity.
- Lymphoid cells.
Lamellar Bodies: Secretory organelles found in type II alveolar cells and kertainocytes in the skin.

Give an overview of the defence mechanisms in the respiratory tract.
- Warming & humidification of air.
- Muco-ciliary escalator
Secreted factors for non-specific defence:
- A number of factors produced by epithelial cells & other cells or derived from plasma.
- Anti-proteases e.g. a1-antirypsin - inhibits proteases released from bacteria/neutrophils.
- Lysozyme - has antifungal and bacteriocidal properties.
- Antimicrobial proteins: Lactoferrin, Peroxidases & Neutrophil-derived Defensins & Cathelicidins.
What principal immunglobulin exists within respiratory tract?
IgA.
Give an example of immune defence mechanisms:
- Leucocytes: neutrophils & lymphocytes present in alveoli.
- Neutrophils kill bacteria
- Alveolar macrophages migrate throughout the respiratory tract - phagocytose any particles that get this far.
- Macrophages act as antigen presenting cells & products presented to T & B lymphocytes.
- Macrophages secrete Interleukens (ILs), Tumour Necrosis Factor (TNF) & chemokines.
- ILs & TNF activate immune system.
- Chemokines attract white cells to site of inflammation.
- Mast cells secrete heparin, histamine, 5-HT & hydrolytic enzymes involved in allergy & anaphylaxis (IgE).
How do Natural Killer (NK) cells confer immunity?
- Present in lungs & lymphoid organs.
- Contains granules with hydrolytic enzymes.
- 1st line of defence against viruses.
- Secrete interferons & TNFs.
- T & B lymphocytes migrate to lymph nodes, tonsils & adenoids.
- Diffuse batches of bronchus-associated lymphoid tissue (BALT) in lamina propria.
- Antigens presented to T-lymphocytes by antigen-presenting cells-cascade of cytokines released & a variety of antibodies produced (Immunoglobulins).
- Most important are dendritic cells.
- Specialised mononuclear phagocytes.
- Act as antigen presenting cells.
Give some background info about the cough reflex
- Caused by irritation of respiratory tract by gases, smoke & dust.
- Receptors throughout the airways between epithelial cells.
- Rapidly adapting afferent myelinated fibres in vagus.
- In trachea, leads to cough. Lower airway leads to hyperpnoea.
- Also causes reflex bronchia & laryngeal constrictions.
- Characterised by deep inspiration followed by forced expiration with closed glottis.
- Results in expulsion of irritants from respiratory tract.
Explain some stuff about the sneezing reflex.
- Caused by irritation of nasal mucous membrane due to dust particles, debris and excess fluid accumulation.
- Characterised by deep inspiration followed by forced expiration with open glottis.
- Results in expulsion of irritant from airways.
- Irritation of nasal mucous membrane, olfactory receptors and trigeminal nerve endings in nasal mucosa.
- Afferents from trigeminal and olfactory nerves pass to sneezing centre in medulla.
- Efferent fibres pass from medulla via trigeminal, facial, glossopharyngeal, vagus and intercostal nerves.
- Results in activation of pharyngeal, tracheal & respiratory muscles.
Briefly describe the process and benefits of the swallowing reflex.
- Initiated by stimuli to dorsum of tongue, soft palate & epiglottis.
- During swallowing, respiration is inhibited - deglutition.
- Prevents inhalation of food.
Give some facts about the stretch receptors and why they are relevant for respiration.
- Located in the smooth muscle of bronchial walls
- Slowly adapting
- Afferents ascend via vagus
- Stimulation results in inspiration being shorter and shallower
- These receptors responsible for Hering-Breuer inspiratory reflex.
- Lung inflation inhibits inspiratory muscle activity.
- Deflation reflex-augments inspiratory muscle activity.
- Normal breathing weak reflex, more active during excersise when tidal volume > 1L.
- In neonates, protects against over-inflation.
Explain the significance of the Juxtapulmonary (J) receptors:
- Located on alveolar & bronchial walls close to capillaries.
- Afferent unmyelinated C-fibers or myelinated nerves in vagus.
Activation causes:
- Apnoea (cessation of breathing) or rapid shallow breathing
- HR & BP fall
- Laryngeal constriction & relaxation of the skeletal muscles.
J receptors activated by:
- Increased alveolar wall fluid
- Pulmonary congestion and oedema
- Microembolisms
- Inflammatory mediators such as histamine
(Above associated with lung disease).


