Respiratory disorders - respiratory infections Flashcards
Respiratory infections
Pathogens
- Viruses cause 80–90% of childhood respiratory infections. The most important are the respiratory
- most important are the respiratory syncytial virus (RSV), rhinoviruses, parainfluenza, influenza, metapneumovirus and adenoviruses
- individual virus can cause several different patterns of illness, e.g. RSV can cause bronchiolitis, croup, pneumonia or a common cold
- important bacterial pathogens of the respiratory tract are Streptococcus pneumoniae (pneumococcus) and other streptococci, Haemophilus influenzae, Moraxella catarrhalis, Bordetella pertussis, which causes whooping cough, and Mycoplasma pneumoniae
Respiratory infections
Classification of respiratory infections

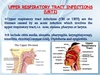
Respiratory infections are classified according to the level of the respiratory tract most involved:
- Upper respiratory tract infection
- Laryngeal/tracheal infection
- Bronchitis
- Bronchiolitis
- Pneumonia.

Respiratory infections
Upper respiratory tract infection (URTI)
Approximately 80% of all respiratory infections involve only the nose, throat, ears or sinuses. The term URTI embraces a number of different conditions:
- Common cold (coryza)
- Sore throat (pharyngitis, including tonsillitis)
- Acute otitis media
- Sinusitis (relatively uncommon).
URTIs may cause:
- Difficulty in feeding in infants as their noses are blocked and this obstructs breathing
- Febrile convulsions
- Acute exacerbations of asthma.

Respiratory infections
The common cold (coryza)
- commonest infection of childhood. Classical features include a clear or mucopurulent nasal discharge and nasal blockage
- commonest pathogens are viruses – rhinoviruses (of which there are over 100 different serotypes), coronaviruses and RSV
- Fever and pain are best treated with paracetamol or ibuprofen. Antibiotics are of no benefit as the common cold is viral in origin and secondary bacterial infection is very uncommon
Respiratory infections
Sore throat (pharyngitis)
- The pharynx and soft palate are inflamed and local lymph nodes are enlarged and tender.
- Sore throats are usually due to viral infection with respiratory viruses (mostly adenoviruses, enteroviruses and rhinoviruses).
- In the older child, group A β-haemolytic streptococcus is a common pathogen.
Respiratory infections
Tonsillitis
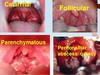
- Tonsillitis is a form of pharyngitis where there is intense inflammation of the tonsils
- Common pathogens are group A β-haemolytic streptococci and the Epstein–Barr virus (infectious mononucleosis). Group A β-haemolytic streptococcus can be cultured from many tonsils
- Marked constitutional disturbance, such as headache, apathy and abdominal pain, white tonsillar exudate and cervical lymphadenopathy, is more common with bacterial infection
- Antibiotics (often penicillin, or erythromycin if there is penicillin allergy) are often prescribed for severe pharyngitis and tonsillitis even though only a third are caused by bacteria
- Amoxicillin is best avoided as it may cause a widespread maculopapular rash if the tonsillitis is due to infectious mononucleosis

Respiratory infections
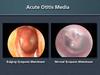
Acute infection of the middle ear (acute otitis media)
Acute otitis media
Can only be diagnosed by examining the tympanic membrane
Antibiotics marginally shorten the duration of pain but do not reduce hearing loss
If recurrent, may result in otitis media with effusion, which may cause speech and learning difficulties from hearing loss.

- most common at 6–12 months of age. Up to 20% will have three or more episodes. Infants and young children are prone to acute otitis media because their Eustachian tubes are short, horizontal and function poorly
- In acute otitis media, the tympanic membrane is seen to be bright red and bulging with loss of the normal light reflection
- Pathogens include viruses, especially RSV and rhinovirus, and bacteria including pneumococcus, non-typeable H. influenzae and Moraxella catarrhalis
- Most cases of acute otitis media resolve spontaneously. Antibiotics marginally shorten the duration of pain but have not been shown to reduce the risk of hearing loss
- Amoxicillin is widely used. Neither decongestants nor antihistamines are beneficial.
Respiratory infections
Sinusitis
- Infection of the paranasal sinuses may occur with viral URTIs. Occasionally there is secondary bacterial infection, with pain, swelling and tenderness over the cheek from infection of the maxillary sinus
- Antibiotics and analgesia are used for acute sinusitis in addition to topical decongestants.
*
Respiratory infections
Tonsillectomy and adenoidectomy

The indications for tonsillectomy are controversial, and must be balanced against the risks of surgery, but include:
- Recurrent severe tonsillitis (as opposed to recurrent URTIs) – tonsillectomy reduces the number of episodes of tonsillitis by a third, e.g. from three to two per year, but is unlikely to benefit mild symptoms.
- A peritonsillar abscess (quinsy)
- Obstructive sleep apnoea (the adenoids will also normally be removed).

Respiratory infections
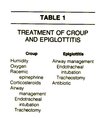
Laryngeal and tracheal infections
The mucosal inflammation and swelling produced by laryngeal and tracheal infections can rapidly cause life-threatening obstruction of the airway in young children. Several conditions can cause acute upper airways obstruction (Box 16.1). They are characterised by:
- Stridor, a rasping sound heard predominantly on inspiration
- Hoarseness due to inflammation of the vocal cords
- A barking cough like a sea lion
- A variable degree of dyspnoea.
Respiratory infections
Croup

- mucosal inflammation and increased secretions affecting the airway, but it is the oedema of the subglottic area that is potentially dangerous in young children because it may result in critical narrowing of the trachea.
- Viral croup accounts for over 95% of laryngotracheal infections
- Parainfluenza viruses are the commonest cause, but other viruses, such as human metapneumovirus, RSV and influenza, can produce a similar clinical picture
- Croup occurs from 6 months to 6 years of age but the peak incidence is in the second year of life. It is commonest in the autumn.
- typical features are a barking cough, harsh stridor and hoarseness, usually preceded by fever and coryza. The symptoms often start, and are worse, at night
Respiratory infections
Bronchitis

- While some inflammation of the bronchi producing a mixture of wheeze and coarse crackles is often a feature of respiratory infections, bronchitis in children is very different from the chronic bronchitis of adults
- In acute bronchitis in children, cough and fever are the main symptoms. The cough may persist for about 2 weeks, or longer with pertussis or Mycoplasma infections. There is no evidence that antibiotics, cough suppressants or expectorants speed recovery.

Respiratory infections
Whooping cough (pertussis)
Pertussis
Caused by Bordetella pertussis
Paroxysmal cough followed by inspiratory whoop and vomiting; in infants, apnoea rather than whoop, which is potentially dangerous
Diagnosis: culture of organism on per-nasal swab, marked lymphocytosis on blood film.
- highly contagious respiratory infection caused by Bordetella pertussis. It is endemic, with epidemics every 3–4 years
- After a week of coryza (catarrhal phase), the child develops a characteristic paroxysmal or spasmodic cough followed by a characteristic inspiratory whoop (paroxysmal phase)
- The spasms of cough are often worse at night and may culminate in vomiting. During a paroxysm, the child goes red or blue in the face, and mucus flows from the nose and mouth.
- Epistaxis and subconjunctival haemorrhages can occur after vigorous coughing. The paroxysmal phase lasts 3–6 weeks
- Complications of pertussis, such as pneumonia, convulsions and bronchiectasis, are uncommon, but there is still a significant mortality, particularly in infants
- organism can be identified early in the disease from culture of a per-nasal swab, although PCR is more sensitive. Characteristically, there is a marked lymphocytosis (>15 × 109/L) on a blood count


