Quiz 4 Flashcards
(68 cards)
What is the billing function in health care
process of quantifying health care services to insurance carriers, 3rd party payors, and patients for reimbursement.
ICD-10
diagnosis, 3-7 digit alphanumeric code
ICD-10-CM
Clinical diagnosis
ICD-10-PCS
Hospital diagnosis
CPT
procedure
HCPCS
CPT for Medicare
What does NPI stand for
National Provider Identifier
When did NPI start
HIPAA 1996
What is NPI
10 digit unique alphanumeric number that is similar to a SSN, but it is given out to other providers
Who has to have an NPI
physicians, non physician extenders, CRNA
What is credentialing
verification of health care practitioners education, training, and work
What is UPD
Universal Provider Database, uniform application that any provider can complete for credentialing.
What are some payors additional requirements for credentialing?
Every 2 years
What are the different levels of an established patient office visit?
Level 1: 99211, patient gets blood pressure checked, less documentation Level 2: 99212 Level 3: 99213 Level 4: 99214 Level 5: 99215, 15-20 minutes of face time with doctor, more documentation
How much reimbursement does Medicare allow for a 99211?
$18
How much reimbursement does Medicare allow for a 99215?
$134
Why is documentation important
it is linked directly to reimbursement, the more specific and complex
Bellcurve
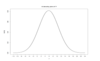
there is a normal distribution between 99211 and 99215
Skewed left

not using rescouces properly, not documenting appropriately, administration might be conservative
Skewed right

might have more severe cases, but still need good documentation, red flag for CMS, coders might not be trained properly
What does coding and reimbursement depend on?
Medical necessity= CPT+ICD-10
ABN
Advanced beneficiary notice, form that patient signs saying that they will pay out of pocket what Medicare doesn’t pay
Claim
itemized statement of services and costs from a health care provider submitted to payers for payment
UB04 (CMS 1450)
Hospital inpatient


