Pulmonology Flashcards
Most common CAP Pediatric patients
Pediatric patients
• Age 4 mo to 4 yrs
– Most common pathogen
• RSV
– Peak incidence • 2-7 mo of age
• Age 5-18 yrs
– Most common pathogen • Mycoplasma pneumoniae – Treat with a macrolide
Score for Pneumonia Severity
Estimates mortality of community-acquired pneumonia to help determine inpatient vs. outpatient treatment.

CAP Treatment for Outpatient, previously healthy, no risk for DRSP infection
Outpatient, previously healthy, no risk for DRSP infection
– Macrolides (SOR A) • Azithromycin • Clarithromycin • Erythromycin
OR
– Doxycycline (SOR B)
CAP treatment for Outpatient with comorbidities or recent abx

CAP treatment for Inpatient (Non-ICU)
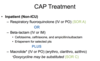
CAP treatment for Inpatient (ICU)

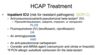
HCAP Treatment - Outpatient or inpatient

HCAP Treatment - ICU
Pneumococcal Vaccines
PPSV23—Pneumococcal Polysaccharide vaccine (Pneumovax)
– 23 serotypes that cause 80% of invasive pneumococcal disease in US – B-cell response – 96% drop in pneumonia caused by susceptible strains
PCV-13—Pneumococcal Conjugate vaccine (Prevnar 13)
– T-cell response
Conjugate Vaccine (PCV13)
- Primary series 2, 4, 6 months, booster 12-15 months
- All adults > 65
- Adults > 19 with CSF leaks, cochlear implants, functional asplenia or immunosuppression
Polysaccharide Vaccine (PPSV) 23

How to Give Both PCV13 and PPSV23
CDC now recommends 2 pneumococcal vaccines for adults >65 years
- Age 2-18– Give 1 dose of PPSV23 at least 8 weeks after the final dose of PCV13. (If immune compromise or asplenia, should receive a 2nd dose of PPSV23 5 years after the first PPSV23)
- Age 19-64 at high risk – give PCV13 first followed by PPSV23 at least 8 weeks later
- Age > 65 give PCV13 first, followed by PPSV23 6 to 12 months later (min 8 weeks if immunocompromised)
- If your patient has received any doses of PPSV23, the dose of PCV13 should be given at least 1 year later

TB Skin Testing > 5 mm is considered positive if:
- HIV sero-positive
- Recent TB direct contact
- CXR shows prior inactive TB
- Immunosuppressed patients – Prednisone > 15 mg/day – TNF-a antagonists – Organ transplant recipients
TB Skin Testing
> 10 mm is considered positive if:
Long-term care facility – Resident or employee • Inmate • IV drug user • Children < 4 yrs of age • Mycobacteriology lab personnel • Diabetic • Renal failure • Cancer • Recent immigrant (< 5 yrs) from high-risk country • High-prevalence area
TB Skin Testing > 15 mm is considered positive if:
• Any person with no known risk factors – Even if prior BCG vaccination
Booster Phenomenon
- Some people infected with M. tuberculosis may have a negative reaction to the TST if many years have passed since they became infected.
- They may have a (+) reaction to a subsequent TST because the initial test “stimulates” their ability to react to the test. – This may incorrectly be interpreted as a skin test conversion
- The two-step test is indicated for serial testing situations, to avoid thinking that this latent “wake up” is a new infection or conversion
Two-Step Skin Testing

Workup of Positive TST or IGRA
- Check CXR for active disease – If CXR Negative (latent tuberculosis)
- Isoniazid (INH) for 6-9 months (9 mo is preferred) – Daily or intermittently (twice weekly) – Use directly observed therapy (DOT) for intermittent regimen
- Rifampin daily for 4 months, consider adding Pyridoxine
- Monthly exams for signs of hepatitis and medication adherence, check liver transaminases if indicated
Workup of Positive TST or IGRA
- If CXR positive (Active tuberculosis)
- Aggressive Combination therapy indicated to decrease mortality, transmission, and resistance • Four-drug treatment initially: – Isoniazid (INH) – Rifampin (RIF) – Ethambutol (EMB) – Pyrazinamide (PZA)
- Treatment regimen modified once culture results received
Post-Treatment Follow-Up
Regardless of whether Rx for LTBI was completed, serial or repeat CXRs are not indicated unless signs or symptoms of TB develop
Fungal Lung Infections
Opportunistic (more likely in immunocompromised)
• Aspergillosis • Candidiasis
Endemic (farm workers, etc)
- Mississippi/Ohio Valley: Histoplasmosis and Blastomycosis
- Southwest: Coccidiodomycosis
What percentage of airway reversibility and change in FEV1 do you need in order to confirm the diagnosis of asthma?
12% and 200 mL
Spirometry in Asthma
- FEV1 is decreased to < 80% predicted
- TLC is normal to elevated • FRC is usually elevated • Significant reversibility after inhaling a SABA – Increase by ≥ 12% and – 200 mL in FEV1

Asthma Classification – NHLBI

Asthma During Pregnancy
- Albuterol is the preferred SABA
- ICSs are preferred controller medication – Budesonide has the most reliable safety profile
- Comorbid allergic rhinitis can be managed with intranasal steroids
Stepwise Treatment Approach for asthma

What is true regarding COPD and mortality in the U.S?
It is the 3rd leading cause of death
COPD Common Symptoms
Cough (85%)
Dyspnea, exertional (70%)
Wheezing (40%)
What proportion of active smokers are likely to develop COPD?
25%
COPD Diagnosis
- Single best variable for identifying adults is a history of > 40 pack yrs of smoking
- Combination of all 3 of the following almost ensures the presence of obstruction
– > 55 pack yr hx
– Wheezing on auscultation
– Patient self-reporting of wheezing
- Absence of all 3 essentially rules it out
- Spirometry is the key test – Recommended for all symptomatic adults • USPSTF recommends against screening asymptomatic adults for COPD using spirometry (Grade D)
– Not recommended to track disease progression or modify Rx after it has been initiated
COPD Workup
- If abnormal spirometry:
- CXR to evaluate for – Lung nodules – Masses – Fibrotic changes
- Alpha-1 Antitrypsin Deficiency Screening: Perform when COPD develops in patients of Caucasian descent under 45 years, or with a strong family history of COPD
COPD staging

What is true concerning nicotine replacement therapy (NRT) for smoking cessation?
NRT will double the chance of quitting
What are the only interventions proven to prolong survival of patients with COPD?
Tobacco cessation and O2 therapy
Tobacco Cessation
- Proven interventions (may double chance of quitting!) • Counselling*
- Nicotine replacement therapy (NRT)
- Patch, gum, lozenge, inhaler, nasal spray all equally effective
- Nicotine vapor (“vaping”) not proven to help
- Varenicline (Chantix) – nicotine blockade
- Bupropion SR (Zyban)
*Counselling and meds more effective together than either one alone
COPD Management immunization
Immunization status monitoring:
– Pneumococcal – Influenza (yearly) – others
COPD Management

Inhaled corticosteroid therapy is associated with an increased risk of
Inhaled corticosteroid therapy is associated with an increased risk of pneumonia
Classification of COPD Exacerbations
Mild Can be controlled with an increase in dosage of regular medications
Moderate Requires treatment with systemic corticosteroids or antibiotics
Severe Requires hospitalization or evaluation in the emergency department
Antibiotics should be given in exacerbation of COPD with all three symptoms:
Antibiotics should be given in exacerbation of COPD with all three symptoms: (SOR B)
– Increased dyspnea
– Increased sputum volume
– Increased purulence or
– If hospitalized for COPD and mechanical ventilation (invasive or non-invasive) is required
Acute COPD Exacerbations: Treatment Options
Oxygen: titrate to target O2 saturation of 88-92%.
Bronchodilators: Short-acting inhaled beta2-agonists with or without short-acting anticholinergics are preferred.
Systemic Corticosteroids: 40 mg prednisone per day for 5 days is recommended.
Nebulized magnesium – No (Ann Thoracic Med 2014).
1 cancer in men and women
Lung Cancer
Lung Cancer Screening
• USPSTF recommendation
The USPSTF recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 55 to 80 years who have a 30 pack-year smoking history and currently smoke or have quit within the past 15 years.
Screening should be discontinued once a person has not smoked for 15 years
Sarcoidosis Symptoms
- Shortness of breath, cough
- Reddish bumps or patches on the skin
- Enlarged lymph nodes in the chest, neck, axillae
- Fever, weight loss, fatigue, night sweats, general feeling of ill health
- Lofgren’s syndrome – acute form of sarcoid – erythema nodosum, fever, arthritis, self-limited
Lofgren’s syndrome
acute form of sarcoid
– erythema nodosum, fever, arthritis, self-limited
Sarcoidosis Diagnosis
- Granulomas in lung tissue biopsy
- Typical signs and symptoms of sarcoidosis like picture
- Abnormal CXR or lung CT
Extra Pulmonary Manifestations of Sacaridosis
- 90% confined to lung, but may involve:
- Eye – acute anterior uveitis
- Skin – cutaneous involvement, erythema nodosum
- Neurosarcoidosis – may have intracranial lesions or peripheral neuropathy
- Cardiac granulomas – cardiomyopathy
- Symptoms may resolve in 2-3 years, or may persist indefinitely
Sarcoidosis Treatment
- No specific treatment or cure; Focus is on management of symptoms, anti-inflammatory meds, reduced lung exposure to toxins, and nutrition
- Follow angiotensin-converting enzyme (ACE) levels in the blood to follow disease activity
- Corticosteroids are mainstay of treatment (start 20-40 mg a day, 5-10 mg a day maintenance)
- Also used: methotrexate, azathioprine, chloroquine, etanercept (Enbrel), infliximab (Remicaide) – consult Pulmonary
Wegener’s Granulomatosis



