Pulmonary Embolism Flashcards
(11 cards)
Define pulomonary embolism
Occlusion of pulmonary vessels, most commonly by a thrombus that has travelled to the pulmonary vascular system from another site
Explain the aetiology/ risk factors of pulmonary embolism
Causes:
-
Thrombus:
- 95% arise from DVT in proximal leg or iliac veins
- rarely from atrium in AF
- post-MI from right ventricle
- Septic emboli
-
Other:
- Fat
- Air
- Tumour
- Amniotic fluid
- Mycotic
Risk factors SPASMODICAL:
- Sex Female
- Pregnancy
- Age up
- Surgery (10 days post-op)
- Malignancy
- OCP/HRT
- DVT/PE hx
- Immobility
- Colossal size
- Antiphospholipid syndrome
- Lupus anticoagulants
Summarise the epidemiology of PE
Relatively COMMON esp in hospitalised px
Occur in 10-20% of px with confirmed proximal DVT
Recognise the presenting symptoms of pulmonary embolism
Depend on size and site
Small - may be asymptomatic
Moderate -
- Sudden onset SOB
- Cough
- Haemoptysis
- Pleuritic chest pain
Large or proximal -
- As above +
- Severe central pleuritic chest pain
- Shock
- Collapse
- Acute right heart failure
- Sudden death
Multiple small recurrent -
- Symptoms of pulm HTN: SOBOE and SOB, syncope and swelling
Recognise the signs of pulmonary embolism
Severity of PE can be assessed based on signs:
Small - often no clinical signs ±tachy and tachypn
Moderate - tachy, tachypn, pleural rub, low O2 despite supplementation
Massive PE - shock, collapse, cyanosis, signs of right heat strain (Raised JVP< left parasternal heave, accentuated S2)
Multiple recurrent PE - signs of pulm HTN, or right heart failure
Identify appropriate investigations for pulmonary embolism
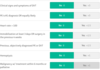
Use Well’s score
- if low probability («4) - use D-dimer
- Negative D-dimer - exclude
- Positive D-dimer - CTPA
- if high probability (>4) - CTPA
Bloods: ABG, thombophilia, FBC, U&Es, D-dimer
ECG:
- may be normal
- T inversion in II,III, aVF and V1-V4
- RBBB
- right ventricular strain: Inverted T waves in V1-4
- tachycardia ±AF or atrial flutter
- S1Q3T3 - rare
CTPA: first line investigation, poor for small good otherwise
VQ Scan: mismatch between ventilation and perfusion, infarcted lung - rarely used
CXR: usually normal, might see linear atelectasis
Pulmonary angiography: invasive, rarely used
Doppler US of LL: enquire for DVT
Echocardiography: right heart strain
Well’s Score for PE
Generate a management plan for pulmonary embolism
Primary prevention:
- RF (mobilisation, hydration, WT, stop OCP…)
- compression stockings
- heparin prophylaxis for those at risk
If haemo stable:
- Oxygen
- AC with heparin or LMWH
- Switch to warfarin for 3 months - maintain INR 2-3
- Analgesia
If haemo unstable:
- Resus: fluids and Oxygen
- Thrombolysis with tPA
Surgical or radiological:
- Embolectomy
- IVC filters for rec PE despite AC or if cant have AC
PE management flow chart

Identify the possible complications of pulmonary embolism
Death
Pulmonary infarction
Pulmonary HTN
Right heart failure
AF
Summarise the prognosis for patients with pulmonary embolism
30% mortality if untreated
8% mortality with treatment
increased risk of future VTE disease


