Pregnancy and labour Flashcards
What are the trimesters of pregnancy defined by?
Defined by experience, not science.
1st = 0-13 weeks (if you make it past the 1st trimester than the pregnancy is 90-95% likely to successfully continue to term)
2nd = 13-26 weeks
3rd = 26-39
26 weeks represents the earliest absolute limit of viability, although modern medicine can push this limit to 22-23 weeks.
How common are miscarriages?
- Most common in the 1st trimester, its estimated 30-60% of pregnancies never survive to the 2nd trimester
- In total its estimated nearly half of all pregnancies miscarraige
What does ‘term’ mean?
- Normally refers to 280 day duration of pregnancy (40 weeks)
- Term = 37-41 weeks of pregnancy
- Before this is pre-term
- After this is post-term
What is the defined time course of pregnancy?
Pregnancy = the first day of the last menstrual period to the day of delivery
What maternal changes in pregnancy are directional?
- Increased weight
- Increased blood clotting tendency
- Increased basal body temperature
- Increased breast size
- Increased vaginal mucus production
- Increased nausea and vomiting (‘morning sickness’)
- Decreased blood pressure
What maternal changes in pregnancy are non-directional?
- Altered brain function
- Altered hormones
- Altered appetite (quantity and quality)
- Altered fluid balance
- Altered emotional state
- Altered joints
- Altered immune system
Why do mothers crave certain foods?
- If the baby is lacking something it will override the mothers need for it and take up all the mothers nutrient stores
- The mother than craves foods high in those nutrients to provide for the baby and restore her own levels
- E.g. iron levels when the baby is producing RBCs
Why do the mothers joints change in pregnancy?
They become more flexible in preparation for having to expand the pelvic girdle when giving birth.
When does the mother increase weight in pregnancy and why does this happen?
- In the 2nd and (mainly) 3rd trimesters
- Usually 10-15 kg.
- This will include the weight of the fetus, amniotic fluid and placenta; increased fluid retention; increased nutritional stores (to feed the baby after delivery).
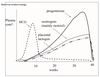
How do maternal hormone levels change in pregnancy?
- HCG peaks in the 1st trimester at aprox 8 weeks then declines
- Progesterone, oestrogens and placental lactogen increase throughout pregnancy and only decline once the placenta has been delivered
What is the significance of the high levels of progesterone and oestrogens in pregnancy?
- Progesterone is the key hormone in allowing the pregnancy to continue.
* Low progesterone levels, or administration of a progesterone antagonist, will lead to loss of the pregnancy at all gestational ages. - High levels of steroid hormones (progesterone and oestrogens) suppress the HPG axis
* Results in very low levels of LH and FSH throughout pregnancy, and hence no cyclic ovarian or uterine functions.
Define:
conceptus
embryo
fetus
infant
- Conceptus – everything resulting from the fertilised egg (baby, placenta, fetal membranes, umbilical cord)
- Embryo – the baby before it is clearly human
- Fetus – the baby for the rest of pregnancy
- Infant – less precise, normally applied after delivery
Where does the progesterone in pregnancy come from?
- From Fertilisation to 8 weeks gestation, the corpus luteum is the main source of progesterone
- This production is sustained by hCG
- From about 6 weeks of gestational age, the corpus luteum gradually produces less progesterone despite the very high hCG levels
- by about 9 weeks it has ceased to make steroids.
- The placenta also produced progesterone relative to its size as it grows during pregnancy
* by 10 weeks of gestation, the placenta is the source of all progesterone. - This change in the source of progesterone to sustain pregnancy is the ‘luteo-placental shift’.
When does the mother increase blood clotting tendency in pregnancy and why does this happen?
- starts early in pregnancy, and is greatest at term
- protective against losing too much blood at delivery,
- May also be important for interactions between the placenta and maternal blood throughout pregnancy
What is the severe form of ‘morning sickness’ called?
hyperemesis gravidarum
What is thought to cause morning sickness and why?
- hCG
- Morning sickness worse in 1st trimester at aprox 8 weeks and declines in the 2nd trimester
- This is the same pattern of hCG levels
Why is eating pattern changed during the latter stages of pregnancy?
- As the size of the uterus increases during the later stages of pregnancy, it imposes steadily increasing pressures on the gastro-intestinal system, including the stomach.
- This can decrease the distensibility of the stomach, and in late pregnancy the mother may need to have up to 6 smaller meals per day, rather than 3 bigger meals.
Why does urinary function change in pregnancy?
- Urinary frequency increases during the first trimester of pregnancy, generally normalises during the second trimester, and increases again in the third trimester.
- The changes in the first trimester are generally thought to be due to changes in the maternal hormones, regulating altered kidney function.
- By the third trimester, the greatly enlarged uterus will be exerting pressure on the bladder, decreasing the maximum size and volume of urine it can contain, so the mother will pass smaller volumes of urine more frequently.
Why does kidney function change during pregnancy?
- To increase fluid retention for a higher plasma volume.
- By the end of pregnancy, maternal blood volume is ~50% higher than before pregnancy.
What is thought to be the cause of altered brain function and mood in pregnancy?
Increased levels of steroid hormones
What systems prevent the fetus from being rejected by the immune system?
- a number of factors that can suppress the maternal immune system are produced at the utero-placental interface.
- decreasing the Th1 responses
- increasing the Th2 system.
- HLA-G is expressed on the maternal side of the placenta
- HLA-G has five known sequence variants so is almost invariant compared to most HLAs
- It is very simplistic - shows the tissue as being human but not whether it is self or non-self, therefore the immune system doesn’t attack it as its not non-self
- can suppress the activity of some leukocytes
- and can down-regulate the maternal immune system within the uterus.
How are oestogens produced during pregnancy?
- Before the luteo-placental shift they’re produced in the corpus luteum
- After this there is a complex interaction between fetal and maternal adrenals, fetal liver and the placenta
- The placenta doesn’t express the CYP 17A1 enzyme that converts pregnenolone to androgens, so this part of biosynthesis takes place in the fetal adrenals
- The weak androgen produced (dehydroepiandrosterone, DHEA) is sulphated as well to give DHEA-S, which is inactive.
- Hence a female fetus is not exposed to any androgens during development.
- The DHEA-S circulates to the placenta, where it is converted to 17beta-oestradiol.

What are the last 4 organ systems to develop?
- the lungs,
- the digestive system,
- the immune system
- the brain.
When is the fetus at greatest risk in pregnancy?
- 1st trimester is most vulnerable e.g to teratogens
- 2nd trimester has little risks
- 3rd trimester risks are the delivery itself

