Physiology Flashcards
(77 cards)
Boyle’s Law
At any constant temperature the pressure exerted by a gas varies inversely with the volume of the gas
(As the volume of a gas INCREASES the pressure of the gas DECREASES)
Forces holding the Thoracic Wall and Lung
INTRAPLEURAL FLUID COHESIVENESS - the water molecules in the intrapleural fluid are attracted to each other. This means that the pleural membranes stick to each other
NEGATIVE INTRAPLEURAL PRESSURE- the subatmospheric intrapleural pressure creates a transmural pressure gradient across the lung and chest wall.
Pressures important in Ventilation
- Atmospheric Pressure
- Intra-alveolar Pressure
- Intrapleural Pressure

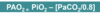
External Respiration
- Exchange between the Atmosphere and Alveoli
- Exchange of O2 and CO2 between the air in alveoli and the blood
- Transport of O2 and CO2 from the lungs to the tissues
- Exchange of O2 and CO2 between the blood and tissues
Inspiration
- Active
- The thorax is increased vertically by the contraction of the diaphragm which flattens
- The external intercostal muscle contraction lifts the ribs and moves out the sternum which increases the thorax anteriorly
- Increase in lung size = intra alveolar pressure falls so air moves into the lungs down the pressure gradient
Expiration
- The inspiratory muscle relaxes
- The chest wall and lungs recoil as elastic properties: this increases intra-alveolar pressure
- Air leaves the lungs down a different pressure gradient
Transpulmonary Pressure
- Transmural pressure gradient in the lungs
- The difference between alveolar and intrapleural pressure in the lungs
- Pneumothroax (air in pleural space) removes transmural gradient

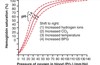
Alveolar Surface Tension
- Allows the lugns to recoil
- Attraction between the water molecules which act on the surface of lung tissue
- Prevents stretching of the lungs, if too strong then alveoli will collapse
Surfactant
- Reduces the alveolar surface tension
- A mixture of lipids and proteins: secreted by Type II alveoli
LaPlace’s Law
- Smaller alveoli have a higher tendency to collapse as the have a smaller radius
- The surfactant lowers the surface tension of smaller alveoli more
Respiratory Distress Syndrome
- Developin foetal lungs = unable to produce surfactant until late in development
- Premature babies may not have enough surfactant
- Baby makes very strenuous inspiratory efforts to overcome high surface tension
Alveolar Interdependence
- Keeps the alveoli open
- If an alvelolus starts to collapse then the surrounding alveoli are stretched and recoil
- This exerts expanding force
Forces keeeping the Alveoli OPEN
- Transmural Pressure Gradient
- Pulmonary Surfactant
- Alveolar Interdependence
Forces keeping the Alveoli CLOSED
- Elasticity of stretched connective tissue
- Alveolar Surface Tension
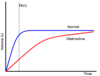
Obstructive Pulmonary Disease
Results from an obstruction or blockage in the airways
Restrictive Pulmonary Disease
Results from the lungs being affected
Tidal Volume (TV)
Volume of air entering/leaving the lungs during a single breath
Average: 500ml
Inspiratory Reserve Volume (IRV)
Extra volume of air that can be maximally inspired over and above the typical resting tidal volume
Average: 3000ml
Inspiratory Capacity (IC)
Maximum volume of air that can be inspired at the end of a normal quiet expiration
IC = Tidal Volume + Inspiratory Reserve Volume
Average: 3500ml
Expiratory Reserve Volume (ERV)
Extra volume of air that can be actively expired by maximal contraction beyond the normal volume of air after resting tidal volume
Average: 1000ml
Residual Volume (RV)
Minimum volume of air remaining in the lungs even after a maximal expiration
Average: 1200ml
Functional Residual Capacity (FRC)
Volume of air in the lungs at the end of a normal passive expiration
FRC = Expiratory Reserve Volume + Residual Volume
Average: 2200ml
Vital Capacity (VC)
Maximum volume of air that can be moved out during a single breath following a maximal inspiration
VC = Inspiratory Reserve Volume + Tidal Volume + Expiratory Reserve Volume
Average: 4500ml
Total Lung Capacity
The maximum volume of air that the lungs can hold
Vital Capacity + Residual Volume
Average: ~5700ml