Phys exam 2 Flashcards
what action is responsible for the heart sounds
the valves closing makes the sound of the heart
which valves are wider and why?
- AV valves
- semilunar valves
- AV valves are wider.
- semilunar valves are narrow because they need to shoot out with more pressure.
The heart does not contract simultaneously.
- What direction does it contract?
- What timing stays the same?
- it contracts from top to bottom
- then bottom to top
- Left & right stay the same, though
Define cardiac output
- what’s remains the same
- what may be different
How much does each portion get (%):
- renal
- GI
- muscles
- cerebral
- coronary + skin
- cardiac output = volume/minute
- pressure may change
- volume stays the same
- each portion
- renal, GI, muscles = 25%
- cerebral = 15%
- coronary + skin = 5%
who discovered that veins have one-way valves
william harvey
amongst the vessels (artery, arteriole, capillary, vein), which has the highest:
- velocity
- surface area
- volume
- control over BP
- velocity = aorta
- surface area = capillaries
- volume = veins
- control over BP = arterioles
Arterioles = greatest site of BP drop off
what determines the resistance of an arteriole?
- what medications constrict it?
- what medications dilate it?
smooth muscle
- constriction = alpha1 agonists
- dilation = beta2 agonists
- NOTE: arterioles are the only** part of the vasculature that **moves
what is the only thing that determines total peripheral resitance?
arterioles
Capillaries
- are they thin/thick
- are they fast/slow
- how many layers of endothelial cells
- are they muscular/not
Capillaries are
- thin
- slow
- 1 layer of endothelial cells
- not muscular
what function do the capillaries serve?
- what happens to lipid soluble material
- what happens to water soluble material
- capillaries are used for diffusion and picking up substances
- lipid soluble stuff goes THROUGH cells (O2, CO2)
- water soluble goes AROUND cells
what controls flow in an arteriole?
sphincters control arteriole size
- ex) pre-capillary sphincters
how many layers do arteries and veins have?
3
- endothelium
- external layer
- smooth muscle layer
what moves blood forward in veins?
name 2 differences between veins and arteries
surrounding muscles move blood forward in veins
3 differences
- they have more capacity than arteries
- they have one-way valves
name 5 arteriole dilators (NNHPP)
name 3 arteriole constrictors (AVN)
dilating substances
- NO
- nitroglycerin
- histamine
- prostaglandins
- prostacyclins
constricting substances
- angiotensin 2
- vasopressin
- nor-epi
what’s the formula for velocity of blood flow?
Q = VA
- Q=flow
- V=velocity
- A=area (diameter)
if you take the same volume through a larger area, flow will be slower (ex: capillaries)
what happens to flow if….
- resistance goes up
- resistance goes down
- pressure at beginning goes up
what’s the major way to change flow
- high resistance = low flow
- low resistance = high flow
- high pressure = high flow
changing resistance = how to change flow
what’s Ohm’s law
Q=ΔP/R
- Q = flow
- P = pressure
- R = resistance
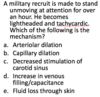
how does dobutamine work for patients with pulmonary embolism?
dobutamine increases pressure, therefore decreasing flow
- Q=ΔP/R
(…is this right?)
What is Poiseuille’s equation?
- what happens to resistance with
- higher viscosity
- longer tube
- narrower tube
Resistance = (Viscosity x Length) / r^4
- greater viscosity = more resistance
- longer tube = more resistance
- narrower tube = more resistancee
Using Pouisseulle’s equation for resistance, explain
- dobutamine vs. congestive failure
- dilating mitral stenosis
- angioplasty
- dobutamine increases pressure (force of contraction)
- this decreases TPR
- this increases the flow
- dilating mitral stenosis
- increased diameter (radius)
- -> decreased resistance
- -> increased flow
- increased diameter (radius)
- angioplasty
- use thrombolytics to increase flow
with flow, what happens if you…
- double length
- double viscosity
- double pressure
- double radius
flow when…
- double length = 1/2 flow
- double viscosity = 1/2 flow
- double pressure = 2x flow
- double radius = 16x flow
Only need 19% increase in radius to double the flow
series and parallel resistance
- what happens to total resistance with
- resistors in series
- resistors in parallel
what are all blood vessels in? (series/parallel)
- resistance in series ADDs
- resistance in parallel DIVIDEs
All blood vessels are in SERIES
- aorta to arteries to capillaries to veins
- cardiac output goes through them sequentially
- greater resistance in ONE means added resistance to the entire system
What blood vessel has the greatest variation in diameter (and thus, resistance)?
Thus, what do most BP medications target?
arterioles
- this is why most medications target arteriole diameter
- calcium blockers
- ACE inhibitors
- angiotensin receptor blockers
- beta blockers are hard to understand
- beta2 stimulation dilates
- but then why do beta blockers decrease BP?
- beta blockers decrease HR and lower renin
what will more parallel resistors do to the total resistance of a system?
more parallel resistors = lower total resistance
- adding a new ORGAN will decrease total resistance
- ex) the liver is a resistor in parallel
it’s like many toll booths
- does not mean slower flow
- does not always mean narrowing

what is “laminar flow”?
- is it faster or slower flow
- where within a vessel would you see the fastest flow of blood
- by the walls
- center of the vessel
- laminar flow = faster flow
- smooth layers flow quickly
- quickest flow is in the center, without the turbulence from the walls

R______’s number measures turbulence
what happens to turbulence as you increase…
- density
- diameter
- velocity
- viscosity
Reynold’s number = turbulence
HIGH turbulence
- more dense
- more diameter
- more velocity
LOW turbulence
- more viscosity
think NASCAR (wider/faster road, dense traffic = racing)
quicksand = not racing
what are “shearing forces”
- Means “breaking flow into layers”
- More shear = greater difference in velocity
- If everyone’s the same speed, shear is low
- Shear is huge along the walls of a vessel
- Flow is slowest along the walls of a vessel
what is compliance?
compliance = volume / pressure
- “how easy going you are without feeling pressure”
- high compliance = a gallon of liquid goes in and pressure doesn’t change
- low compliance = a gallon of liquid goes in and pressure shoots up
which are high compliance (fill quickly with no pressure change)?
which are low compliance (fill slowly with pressure change)?
- lungs
- veins
- skull
- old arteries
- lymphatics
- stomach
HIGH compliance
- lungs
- veins
- lymphatics
- stomach
LOW compliance
- old arteries
- skull
What are the dangers of LOW compliance?
- blood pressure
- vessels
- which body part is this dangerous for
LOW compliance
- causes hypertension
- causes rupturing of blood vessels
- SKULL = dangerous
- emptying a little bit causes a BIG pressure change
- decompressing skull is dangerous
What is good regarding compliance of:
- skull
- arteries
- lung
- compliant skull = BAD
- compliant arteries = GOOD
- don’t want small volume changes to make HTN
-
lungs
- too compliant = bad (emphysema)
- too non-compliant = bad (fibrosis)
Compliance of blood vessels
- what’s more compliant?
- arteries
- veins
- why?
what happens to compliance artery>capilllaries>veins
- veins are more compliant
- arteries = non-compliant because they need to be able to push
- compliance goes UP, pressure goes DOWN as you go from artery > capillary > vein

what happens if compliance decreases in blood vessels?
- high blood pressure
- strokes
- myocardial infarction
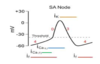
Interpret the attachment
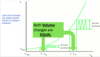
N/A
What kind of vessel is the site of pressure and compliance change?
- aka what kind of vessel controls TPR
- Site of pressure change
- Site of compliance change
- Controls vascular resistance aka TPR
BP = 90-100 mmHg going INTO arterioles
BP = 30 mmHg LEAVING arterioles (60-70% drop)
Why is there a big pressure change with blood entering/leaving capillaries?
Pressure
- 30 mmhg entering
- 5 mmhg leaving
BIG percentage change
Because capillaries need to push nutrients out
More elasticity = ___________ compliance
- More elasticity
- LESS compliance
- ex) arteries
LESS springy would mean better compliance
With blood pressure
- greater pressure = _______ stroke volume
Which phase lasts longer (systolic/diastolic)?
- therefore, the mean BP is closer to which?
What is “pulse pressure”?
- With high compliance, would you see a large or small pulse pressure?
- What’s the formula for mean arterial pressure?
- greater pressure = greater stroke volume
- diastolic phase lasts longer
- you spend 2x as much time in diastole!
- mean BP is closer to diastolic value
- pulse pressure = difference between sys/dias
- high compliance = small pulse pressure
- MAP = diastole + 1/3 pulse pressure
what causes the “dicrotic notch” in a heartbeat?

- Dip down in BP after systole
- The springy aortic valve “rebounds” after closing and pushes up, pushing pressure up.
- Like jumping down and up on a trampoline
Image:
- Closure of aortic valve (A2) makes pressure go down
- Rebounding back UP of aortic valve pushes pressure UP

What is the MOST “physiologically accurate” measure of organ perfusion
Mean arterial pressure (MAP)
What happens to compliance with atherosclerosis?
- what happens to BP/MAP
- Does stroke volume change?
The harder the arteries, the less compliant
Greater pressure from the same original stroke volume
Raises Systolic BP, MAP
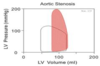
What’s aortic stenosis?
What chamber experiences higher pressure as a result?
- Crunchy, clogged aorta
- Blocks exit of blood from Heart
- Normal = NO gradient (no difference) between LV and aorta pressure. Both 120
- Stenosis = LV pressure > aorta pressure

Which valve(s) lesions give you
- SOB
- CHF
All valves can
What happens to the pulse as a result of aortic stenosis?
- What happens to timing of aortic valve closure
- What is the timing in relation to the pulmonary valve closure
- How will this sound on exam?
- Delays the pulse
- Decreases perfusion of the brain
- Can result in syncope
- Results in delayed closure of the aortic valve
- Was supposed to be before the pulmonary valve
- Systolic crescendo-decrescendo = murmur (delayed)

A long term smoker comes with increasing swelling of his legs. There is ascites and enlargement of the liver and spleen. Which is most likely to be present?
A.Right ventricular hypertrophy
B.Patent foramen ovale
C.Left ventricular atrophy
D.Pulmonary hypotension
E.Increased cardiac output
A.Right ventricular hypertrophy (fyi, the disease is COPD)
What happens to the blood in the heart with aortic regurgitation?
- What happens to pulse pressure
- Which chamber is affected?
- Regurgitation = insufficency
- Blood spills backward
- Heart creates an extra high EF to compensate for spillage
- Greater pulse pressure
- LV gets enlarged (bad)

What is compliance of the lungs (high/low)
How about the pulmonary artery?
- Pulmonary Artery = very compliant
- to allow for it to be filled with air volume
- Low pressure
- Lungs are “Soft and Squishy”
1Which part of vascular system has the greatest CHANGE in pressure?
a. Aorta
b. Arteries
c. Arterioles
d. Capillaries
e. Veins
c.Arterioles
What is the main reason Mean arterial pressure is closer to diastolic pressure?
a. Arteries are less compliant than veins
b. Elasticity of Arterioles
c. Loss of fluids by hydrostatic forces in capillaries
d. Two-thirds of cardiac cycle is in diastole
d.Two-thirds of cardiac cycle is in diastole
- Which is more elastic?
a. Arteries of older persons
b. Capillaries of young people
c. Veins of older persons
d. Lymph channels at any age
a.Arteries of older persons
- Elasticity opposes compliance
- Thick elastic walls = arteries
- What is the site of action of treatment of Aortic regurgitation?
a. Aorta
b. Pulmonary artery
c. Arterioles
d. Capillaries
e. Veins
c.Arterioles
- All of our drugs target arterioles
- Aorta = on LEFT
- Pulmonary artery = on RIGHT
What is the most accurate test of aortic stenosis?
a. Electrocardiogram (EKG)
b. Chest Xray
c. Left heart catheterization
d. Right heart catheterization
e. Echocardiogram
c.Left heart catheterization
It’s the only way to get the most specific pressure measurements
Why do aortic stenosis and regurgitation cause dyspnea?
a. Increased hydrostatic pressure in peripheral capillaries
b. Loss of oncotic pressure
c. Pulmonary hypertension
d. Increased pulmonary capillary hydrostatic pressure
e. Increased venous return to right heart
d.Increased pulmonary capillary hydrostatic pressure
- Peripheral capillaries are your hands, and you don’t breathe from there
- Oncotic pressure = plasma proteins and that doesn’t deal with this
- D is correct because blood & fluid gets backed up into the lungs, then pushing fluid back into the alveoli, making you SOB
A man with shortness of breath that has been happening for months with a systolic murmur going to his neck. What test will you do first to show the diagnosis?
a. Xray
b. Cardiac Catheterization
c. EKG
d. Echocardiogram
d.Echocardiogram
Injection drug user with fever and a murmur. Blood cultures grow Staphylococcus. He develops sudden shortness of breath, lung congestion and rales. Murmur worsens. What structure broke?
a. Chordae/Papillary muscle
b. Atrial septum
c. Aorta
d. Pulmonary artery
a. Chordae/Papillary muscle
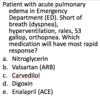
A woman is in intensive care with overwhelming infection and septic shock. Her blood pressure is 70/40 and pulse 120/minute
Which of these will help her?
a. Nitric Oxide
b. Nitroglycerin
c. Histamine
d. Prostaglandins
e. Norepinephrine
e.Norepinephrine