Pharm: Osteoporosis Drugs Flashcards
(22 cards)
What is the MOA of calcitonin-salmon?
Inhibits the activity of osteoclasts to ↓ bone resorption
What are the 2 main clinical applications of calcitonin-salmon?
- Tx of established osteoporosis
- Used for Paget disease of bone

Bisphsphonates are structural analogs of what; what is their MOA?
- Structural analogs of pyrophosphate, normal component of bone
- Incorporated into bone, then inhibit bone resorption by ↓↓ both the number and activity of osteoclasts

Bisphosphonates are the drugs of first choice for what 5 conditions?
- Postmenopausal osteoporosis
- Osteoporosis in men
- Glucocorticoid-induced osteoporosis
- Paget disease of bone
- Hypercalcemia of malignancy

What are the AE’s associated with bisphosphonates?
- Esophagitis: minimized by taking meds with 8oz of water
- Osteonecrosis of the jaw
- Atypical femur fractures

Which bisphosphonate has been most commonly associated with osteonecrosis of the jaw and also dose-dependent kidney damage and rarely atrial fibrillation?
Zolendronic acid (IV)

Which SERM can be used to prevent and treat postmenopausal osteoporosis?
Raloxifene

Where is the SERM, Raloxifene an agonist and antagonist of estrogen effects?
- Blocks in breast and uterus
- Agonist in the bone

What is the drug of choice for prevention and treatment of postmenopausal osteoporosis in pt at risk of estrogen-dependent breast cancer?
Raloxifene

The SERM, Raloxifene increases the risk for what AE’s?
- DVT’s
- Pulmonary embolism
- Stroke

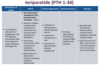
What is the only drug for osteoporosis that increases bone formation?
Teriparatide

When Teriparatide is administered in which fashion it increases bone deposition by osteoblasts?
Given as a daily pulsed therapy
What is the MOA and effect of Denosumab?
- Monoclonal antibody that is a RANKL inhibitor
- Binds to RANKL and ↓ formation and function of osteoclasts –> ↓ bone resorption

What are the clincial uses of Denosumab; what should it be taken with?
- Tx osteoporosis in postmenopausal women at high risk for fractures
- Prevention of skeletal-related events in pt’s with bone metastases from solid tumors
- Should be taken with calcium and vitamin D supplement to prevent hypocalcemia

What are some serious AE’s associated with Denosumab?
- ↑ risk of new fractures
- Osteonecrosis of the jaw

What is an important part of the therapy when treating osteoporosis in men; what are the 2 agents most commonly used?
- Testosterone replacement is important part of therapy
- Bisphosphonates (i.e., alendronate) = agent of choice
- Denosumab is an alternative
What is the MOA of cinacalet?
- Binds to CaSR on parathyroid gland —> ↑ sensitivity to extracellular Ca2+
- Leads to ↓ PTH secretion

What are the clinical uses of Cinacalet?
- Primary hyperparatyroidism (parathyroid carcinoma)
- Secondary hyperparathyroidism due to CKD

What are the 3 most common AE’s associated with Cinacalet?
Nausea + vomiting + diarrhea

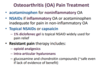
Which drugs can be used for non-inflammatory vs. inflammatory OA?
- Acetaminophen for non-inflammatory OA
- NSAIDs if inflammatory OA or acetaminophen is inadequate for pain in non-inflammtory OA
Which topical NSAID is widely used for OA pain relief?
1% Diclofenec gel
What are 4 effective oral antibiotics used for osteomyelitis; how long should tx be administered for?
- Clindamycin
- Rifampin
- TMP-SMX
- Fluoroquinolones
- Consists of 4-6 week course… time needed for bone revascularization after debridement