Pharm: Cardiac Arrhythmia Flashcards
1
Q
- What are the three class IA drugs?
A
- Quinidine
- Procainamide
- Disopyramide
2
Q
- What are two class IB drugs?
A
- Lidocaine
- Mexiletine
- (Phenytoin in sketchy)
3
Q
- What are 2 class IC drugs?
A
- Flecainide
- Propafenone
4
Q
- What are 2 class II drugs?
A
- Esmolol
- Propanolol
5
Q
- What are four class III drugs?
A
- Amiodarone
- Ibutilide
- Dofetilide
- Sotalol
“AIDS”
6
Q
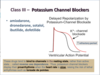
- What are 2 class IV drugs?
A
- Verapamil
- Diltiazem
7
Q
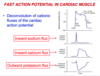
- What is happening during the phases of the fast action potential in cardiac muscle?
A
- Phase 0: voltage-dependent fast Na+ channels open as a result of depolarization; Na+ enters the cells
down its electrochemical gradient - Phase 1: K+ exits cells down its gradient, while fast
Na+ channels close, resulting in some repolarization - Phase 2: plateau phase results from K+ exiting cells
offset by and Ca2+ entering through slow voltage-
dependent Ca2+ channels - Phase 3: Ca2+ channels close and K+ begins to exit
more rapidly resulting in repolarization - Phase 4: Resting membrane potential is gradually
restored by Na+/K+ ATPase and the Na+/Ca2+
exchanger
8
Q
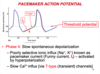
- What is happening during phase 4 of the pacemaker action potential?
A
- phase 4 is a slow spontaneous depolarization
- poorly selective ionic influx of Na, K occurs via If and T-Ca2+ channels, respectively.
9
Q
- What is happening during phase 0 and 3 of the pacemaker action potential?
A
- Phase 0 is the upstroke of nodal action potential
- Ca+2 influx via the relatively slow (L-type**) (long-acting) Ca2+ channels
- Phase 3 is the repolarization of the nodal action potential
- inactivation of calcium channels with ^K+ efflux

10
Q
- How does the rate of spontatneous depolarization in phase 4 effect firing rate of nodes?
A
- decreased slope–> decreased rate of node because it takes more time to reach threshold potential
11
Q
- How does resting potential effect nodal action potential firing rate?
A
- if potential is less negative, less time needed to reach threshold so the firing rate increases
12
Q
- Where is ERP on the action potential?
- Where is AP on the action potential?
A

13
Q
- What are the three states of sodium channels in the heart?
- in which state do the m-gates open?
- in which state do h-gates close?
A
-
Resting state – the channel is closed but ready
to generate action potential -
Activated state – depolarization to the threshold
opens m-gates greatly increasing sodium
permeability -
Inactivated state – h-gates are closed, inward
sodium flux is inhibited, the channel is not
available for reactivation – this state is
responsible for the refractory period

14
Q
- Class I drugs bind most readily to which states of sodium channels?
A
- Activated or inactivated
- very little affinity towards channels in a resting state
15
Q
- What is the order of sodium channel binding affinity in class I drugs?
A
- CAB
- C has highest affinity (**slowest to dissociate**)
- B has lowest affinity (**quickest to dissociate**)
16
Q
- Which class I drugs has intermediate dissociation kinetics?
A
IA
17
Q
- What does K+ channel blockade do?
A

18
Q
- How is the fast action potential effected by 1A drugs?
- AP length?
- Effective refractory period (ERP)?
- QT interval? Why?
- QRS?
A
- AP duration is increased
- ERP is increased
- QT interval is increased (Class IA also block potassium channels)***
- QRS is prolonged (widened)

19
Q
- What type of cells are preferentially targeted by class IA drugs?
A
- Ectopic pacemaker cells with faster rhythms
20
Q
- Which class IA drug has antimuscarinic and ganglionic blocking effects?
- what can this cause?
A
- Procainamide
- can cause hypotension

21
Q
- What are the indications for procainamide?
- acute therapy vs quinidine?
- long term tx?
A
- PSVT
- prevent recurrence of VT
- treat arrhythmias of MI
- tolerated better than quinidine when given IV as acute therapy
- long-term treatment poorly tolerated

22
Q
- What is the active metabolite of procainamide that has class III activity?
- what patient population can this be worrisome?
A
- active metabolite N-acetylprocainamide has class III activity, has longer half-life, accumulates in renal dysfunction patients
- measurements of both parent drug and metabolite are necessary in pharmacokinetic studies
23
Q
- What are the adverse cardiac effects of procainamide?
A
- Prolongs QT (K channel blockage) which can lead to TdP, although not as likely to cause torsades as quinidine
- excessive conduction block

24
Q
- What are some extracardiac adverse effects of procainamide?
- prolonged use can lead to?
A
- N/V/D, rash, fever, hypotension
- prolonged use can lead to a positive ANA test drug-induced lupus syndrome, especially in slow acetylators
- can cause agranulocytosis

25
Q
- What is the MOA of quinidine?
A
- open-state blocker of Na+ channels
- also blocks multiple cardiac K+ channels

26
Q
- Which class IA drug is a natural alkaloid from cinchona bark that has anticholinergic and alpha-adrenergic blocking effects?
A
- Quinidine
27
Q
- What are the effects of quinidine on
- QRS duration?
- QT interval?
- Inotropy?
A
- 10-20% increase in QRS duration
- 25% increase in QT interval
- negative inotrope

28
Q
- What are the indications for use of quinidine?
A
- afib, aflutter (pharmacological conversion) (because Class I are rhythm control drugs)
- maintenance of sinus rhythm in patients with paroxysmal afib/flutter, or life-threatening ventricular arrhythmias
29
Q
- Which drug is associated with decreased hearing, tinnitus, blurred vision, and delirium? What is this called?
A
- Quinidine
- Cinchonism
30
Q
- Which drug with hypersensitivity reactions, thrombocytopenia, and rarely severe hepatotoxic reactions?
A
- Quinidine

31
Q
- Which class IA drug is likely to put you in a normal rhythm, but also 2-3x more likely to kill you?
A
- Qunidine, the prototype class IA drug, which is now seldom used

32
Q
- What is the MOA of disopyramide?
- what effect does it have on peripheral vessels?
A
- blocks Na channels similar to quinidine
- is NOT an alpha-adrenergic receptor antagonist like quinidine, instead is a peripheral vasoconstrictor

33
Q
- How does disopyramide effect
- QRS?
- QT?
- Inotropy?
A
- prolongs QRS
- prolongs QT
- negative inotrope

34
Q
- What are the indications for disopyramide?
- offlabel use?
A
- used to prevent recurrence of vtach or vfib
- maintains sinus rhythm in pts with afib/flutter
- off label use: maintenance of sinuys rhythm in afib patients that have vagally-induced afib or hypertrophic cardiomyopathy

35
Q
- Which class IA drug exerts the most anticholinergic side effects?
- what are these side effects?
A
- Disopyramide
- dry mouth, blurred vision, constipation, urine retention, closed-angle glaucoma**

36
Q
- Which class IA drug is used to convert supraventricular tachycardias such as WPW when given in IV form
- how does this work?
A
- procainamide
- inhibits conduction in the accessory pathway

37
Q
- Which drug is indicated for vagally mediated afib?
A
disopyramide
38
Q
- What does the action potential look like when a patient is given a class IB drug?
A

39
Q
- What effect do class IB drugs have on sodium and potassium channels?
- which state of sodium channels do they bind to?
A
- State-dependent sodium channel blockage
- binds to inactivated sodium channels
- preferentially depolarized cells–> ischemic damage causes depolarization of cells due to loss of ATP
- 1B drugs DO NOT block K+ channels and thus do not (usually) significantly prolong action potential, QT duration.

40
Q
- What is the MOA of lidocaine?
A
- blocks both the initiation and conduction of nerve impulses by decreasing the neuronal membrane’s permeability to sodium ions
- (konorev mentions only inactivated na channels, while wolff says both open and inactivated)