Peritoneum Flashcards
Gross appearance of endosalpingosis?
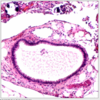
prominent cyst formation
Gross apearance of endocervicosis?
mass in outer cervix/bladder
Histological features of endocervicosis?
Glands lined by endocervical-type epithelium
Hyalinized, fibroblastic, or edematous stroma
± mucin extravasation
IHC for endometrial type stroma?
CD10 positive, p16 patchy positive
IHC for endometrial epithelium?
pax-8, ER, PR positive
IHC for ectopic decidua?
ER, vimentin, desmin positive
CD10 and inhibin-α may be positive
Molecular abnormalities in endometriosis?
± KRAS mutations (endometriosis)
Features of atypical endosalpingosis?
Cytologic atypia that falls short of carcinoma
Features of Serous Borderline Tumour (vs. atypical endosalpingosis)?
May form mass lesion
Architectural complexity with cellular budding and tufting
Eosinophilic cells with abundant cytoplasm are common
Features of Endometriosis with Hyperplasia (vs Endometriosis)?
Glandular crowding and complexity + cytologic atypia
Features of Metastaic Adenocarcinoma (vs. Endometriosis/Endocervicosis/Mullerianosis)?
Prior history &/or concomitant primary
Complex glandular architecture, at least focally
Irregularly shaped and haphazardly infiltrating glands with cytologic atypia
Desmoplastic stroma
Features of Stromal Sarcoma (vs Stromal Endometriosis)?
Prior history or concomitant mass
Features of Low-Grade Müllerian Adenosarcoma (vs. Polypoid Endometriosis)?
Well-developed, leaf-like architecture
Pronounced stromal condensation or “cuffing”
± sex cord-like differentiation or sarcomatous overgrowth
± infiltration of underlying tissues
Stromal cytologic atypia with variable mitotic activity
Features of Deciduoid Mesothelioma (vs ectopic decidua)?
Large, often confluent nodules may be seen
Infiltration of underlying tissues common
May show wide variation in nuclear size and shape
Mitoses may be seen
Numerous, long, slender microvilli by electron microscopy
Keratin (AE1/3, pan keratin, CK7, CK5/6), EMA, D2-40, WT1, mesothelin positive
ER and inhibin negative
Features of Metastatic SCC (vs Ectopic Deccidua)?
Prior history or concomitant ovarian/uterine tumor
Keratin formation and intercellular bridges (i.e., true squamous differentiation)
Cytologic atypia and mitoses
Keratin and p63 positive
p16 diffusely positive (if cervical origin)
Features of Peritoneal Tuberculosis (vs. Necrotic Pseudoxanthomatous Nodules)?
Prior history of tuberculosis, positive tuberculosis test, or immunosuppression
Variably sized, sometimes confluent granulomas with central necrosis
Peripheral palisading of histiocytes and giant cells
Positive AFB stain &/or culture
Gross features of florid mesothelial hyperplasia?
Rough, dull, ± thickened and whitish surfaces
IHC for florrid mesothelial hyperplasia?
- Vimentin, AE1/AE3, calretinin, CK5/6, WT1, D2-40 (podoplanin), thrombomodulin positive
- BAP1 expression preserved
Features of Malignant mesothelioma?
Widespread peritoneal involvement, often with hemorrhagic ascites
Sarcomatoid/storiform component may be present
Invasion of underlying tissues
Necrosis
Marked uniform cytologic atypia
Homozygous p16 deletion (chromosome 9p21) specific (but not sensitive)
BAP1 loss of expression specific (but not sensitive)
Features of well differentiated papillary mesothelioma?
Relatively abundant eosinophilic to amphophilic cytoplasm
Papillae covered by single layer of cuboidal cells
No inflammation, granulation tissue, or hemorrhage
IHC for Peritoneal inclusion cysts?
Vimentin, AE1/AE3, CK5/6, calretinin, WT1, D2-40 (podoplanin), caldesmon, desmin positive

