Paeds Flashcards
Gross motor milestones
3 months
Little or no head lag on being pulled to sit
Lying on abdomen, good head control
Held sitting, lumbar curve
Gross motor milestones
6 months
Lying on abdomen arms extended
Lying on back, lifts and grasps feet
Pulls self to sitting
Held sitting, back straight
Rolls front to back
Gross motor milestones
7-8m
Sits without support
(Refer at 12m)
Gross motor milestones
9 months
Pulls to standing
Crawls
Gross motor milestones
12m
Cruises
Walks with one hand held
Gross motor milestones
13-15m
Walks unsupported
(Refer at 18m)
Gross motor milestones
2y
Runs
Walks upstairs and downstairs holding onto rail
Gross motor milestones
3y
Rides a tricycle using pedals
Walks up stairs without holding a rail
Gross motor milestones
4y
Hops on one leg
Pyloric stenosis presentation:
Pyloric stenosis typically presents in the second to fourth weeks of life with vomiting, although rarely may present later at up to four months. It is caused by hypertrophy of the circular muscles of the pylorus
Features of Py Sten
‘projectile’ vomiting, typically 30 minutes after a feed
constipation and dehydration may also be present
a palpable mass may be present in the upper abdomen
hypochloraemic, hypokalaemic alkalosis due to persistent vomiting
Dx of py sten
USS
Ramstedt pylorotomy
Used in management of py sten
Excision of the hypertrophied circular muscles of the pylorus
Def intussuception
Intussusception describes the invagination of one portion of bowel into the lumen of the adjacent bowel, most commonly around the ileo-caecal region.
Intussusception usually affects infants between 6-18 months old. Boys are affected twice as often as girls
Features of intussuception
paroxysmal abdominal colic pain
during paroxysm the infant will characteristically draw their knees up and turn pale
vomiting
blood stained stool - ‘red-currant jelly’
sausage-shaped mass in the right lower quadrant
Ix intussuception
USS
Mx of intussuception
Air insuffation under radiological control
If the child has signs of peritonitis or the air insufflation fails, Sx
A 2-month-old boy is brought to the afternoon surgery by his mother. Since the morning he has been taking reduced feeds and has been ‘not his usual self’. On examination the baby appears well but has a temperature of 38.7ºC. What is the most appropriate management?
Advise regarding antipyretics, to see if not settling
IM benzylpenicillin
Advise regarding antipyretics, booked appointment for next day
Admit to hospital
Empirical amoxicillin for 7 days
Any child less than 3 months old with a temperature > 38ºC is regarded as a ‘red’ feature in the new NICE guidelines, warranting urgent referral to a paediatrician. Although many experienced GPs may choose not to strictly follow such advice it is important to be aware of recent guidelines for the exam
Assessment of febrile children?
T: electronic thermometer in the axilla if <4w or with infra-red tympanic thermometer
HR
RR
CRT
Signs of dehydration: skin turgor
What are the categroies on the feverish illness guidelines
Colour
Activity
Respiratory
Circulation and hydration
Other
Mx of child at “green” on risk stratificiation for feverish illness?
Managed at home with appropriate care advice, including when to seek further help
Mx of child at “amber” on risk stratificiation for feverish illness?
Safety net or refer to paediatric specialist for further assessment
Safety net: verbal/written info about warning symptoms and how to access further care
Mx of child at “red” on risk stratificiation for feverish illness?
Admit to hospital
Key points for Mx of fever in child
Oral antibiotics should not be prescribed without identification of an apparent source of fever
CXR in ?pneumonia in children?
Not routinely performed
Green
Colour
Normal
Green
Activity
Responds normally to social cures
Content/smiles
Stays awake or wakens quickly
Strong normal cry/not crying
Green
Circulation and hydration
Normal skin and eyes
Moist mucous membranes
Important for Green risk stratification
No amber or red signs present
Amber
Coour
Pallor reported by patient/carer
Amber
Activity
Not responding to social cues normally
No smiles
Wakes only with prolonged stimulation
Decreased activity
Amber
Respiratory
Nasal flaring
Tachypnoea >50 breaths/m aged 6-12
>40 breats/minute age, 12m
Oxygen saturation <95% on air
Crackles in chest
Amber
Circulation
Tachycardia
12m: >160bpm
12-24m >150bpm
2-5y >140
CRT >3
Dry mucous membranes
Poor feeding in infants
Reduced urine output
Amber
Other things of note
3-6m >39 deg temperature
Fever for >5d
Rigors
Swelling of a limb or joint
Non-weight bearing limb/not using an extremity
Red
Colour
Pale/mottled/ashen/blue
Red
Activity
No response to social cues
Appears ill to healthcare professional
Does not wake or does not stay awake
Weak, high-pitched or continuous cry
Red
Respiratory
Grunting
Tachypnoea: RR >60
Moderate or severe chest indrawing
Red
Circulation
Reduced skin turgor
Red
Other features
Age <3m, T >38
Non blanching rash
Bulging fontanelle
Neck stiffness
Status epilepticus
Focal neurological signs
Foal seizures
Tachypnoea
6-12m
>50
Tachypnoea
>12m
>40
Tachycardia
<12m
>160bpm
Tachycardia
12-24m
>150bpm
Tachycardia
2-5y
>140bpm
A 3-year-old girl is brought in by her mother. Her mother reports that she has been eating less and refusing food for the past few weeks. Despite this her mother has noticed that her abdomen is distended and she has developed a ‘beer belly’. For the past year she has opened her bowels around once every other day, passing a stool of ‘normal’ consistency. There are no urinary symptoms. On examination she is on the 50th centile for height and weight. Her abdomen is soft but slightly distended and a non-tender ballotable mass can be felt on the left side. Her mother has tried lactulose but there has no significant improvement. What is the most appropriate next step in management?
Switch to polyethylene glycol 3350 + electrolytes (Movicol Paediatric Plain) and review in two weeks
Speak to a local paediatrician
Reassure normal findings and advise Health Visitor review to improve oral intake
Prescribe a Microlax enema
Continue lactulose and add ispaghula husk sachets
The history of constipation is not particularly convincing. A child passing a stool of normal consistency every other day is within the boundaries of normal. The key point to this question is recognising the abnormal examination finding - a ballotable mass associated with abdominal distension. Whilst an adult with such a ‘red flag’ symptom/sign would be fast-tracked it is more appropriate to speak to a paediatrician to determine the best referral pathway, which would probably be clinic review the same week.
Wilms’ tumour
WIlm’s tumour
Wilms’ nephroblastoma is one of the most common childhood malignancies. It typically presents in children under 5 years of age, with a median age of 3 years old.
Features of Wilm’s tumour
Abdominal mass (most common PC)
Painless haematuria
Flank pain
Anorexia, fever
Unilateral in 95%
Mest found in 20%
Wilm’s associated with
Beckwith-Wiedemann syndrome
As part of WAGR syndrome
Hemihypertrophy
1/3rd associated with a lof mutation in WT1 on chromosome 11
Beckwith-Wiedemann syndrome
Beckwith-Wiedemann syndrome is a condition that affects many parts of the body. It is classified as an overgrowth syndrome, which means that affected infants are considerably larger than normal (macrosomia) and tend to be taller than their peers during childhood. Growth begins to slow by about age 8, and adults with this condition are not unusually tall. In some children with Beckwith-Wiedemann syndrome, specific parts of the body on one side or the other may grow abnormally large, leading to an asymmetric or uneven appearance. This unusual growth pattern, which is known as hemihyperplasia, usually becomes less apparent over time.
WAGR Syndrome
WAGR syndrome is a rare geneticsyndrome in which affected children are predisposed to develop Wilms tumour (a tumour of the kidneys), Aniridia (absence of the coloured part of the eye, the iris),Genitourinary anomalies, and Retardation.[1]The G is sometimes instead given as “gonadoblastoma,” since the genitourinary anomalies are tumours of the gonads (testes or ovaries).[2]
A subset of WAGR syndrome patients shows severe childhood obesity; the acronymWAGRO (O for obesity) has been used to describe this category.[3]
The condition results from a deletion on chromosome 11 resulting in the loss of severalgenes. As such, it is one of the best studied examples of a condition caused by loss of neighbouring (contiguous) genes.[3]
Mx of Wilm’s
Management
nephrectomy
chemotherapy
radiotherapy if advanced disease
prognosis: good, 80% cure rate
Histological features of WIlms
Histological features include epithelial tubules, areas of necrosis, immature glomerular structures, stroma with spindle cells and small cell blastomatous tissues resembling the metanephric blastema
Features of pertussis
Caused by Bordetella pertussis
10-14d incubation
Infants rountely immunised at 2,3,4m and 3-5y. Pregnant women also immunised
Clinical features of pertussis
Coughing bouts: usually worse at night and after feeding, may be ended by vomiting and associated central cyanosis
inspiratory whoop (not always present), caused by forced inspriration against a closed glottis
Persistent coughing may cause subconjunctival haemorrhages or anorexia, leading to syncope and seizures
Symptoms may last 10-14w and tend to be more severe in infants
Lymphocytosis
Dx of pertussis
Per nasal swab culture for B. pertussis
PCR and serology may also be used
Mx of pertussis
Oral erythromycin to eradicate organism and reduce spread
Has not been shown to alter the course of the illness
Cx of pertussis
Subconjunctival haemorrhage
Pneumonia
Bronchiectasis
Seizures
A mother presents to your GP surgery with her six month old daughter. She has been struggling to feed her daughter, and her health visitor found that she was small for her age. Her mother is exhausted as she says her daughter sleeps poorly.
On examination, the baby is just below the 3rd centile in length. She has epicanthic folds and low set ears. Her neck appears short and she has micrognathia. You hear an ejection systolic murmur on auscultation.
What is the most likely diagnosis?
Fragile X syndrome
Down’s syndrome
Patau syndrome
Klinefelter’s syndrome
Turner’s syndrome
Turner’s syndrome is a genetic condition due to a loss or abnormality of one X chromosome. In infancy, children often have difficulty with feeding which contributes to poor weight gain, although the often have short stature too when older. Babies with Turner’s syndrome often have multiple dysmorphic features, but a webbed neck is often classical. It is also associated with cardiac abnormalities, in this question aortic stenosis although others are also common. Chromosome analysis would be needed to confirm the diagnosis.
While Down’s syndrome babies would have many of the dysmorphic features, they would not usually have a webbed neck or micrognathia. They may have loose skin at the nape of the neck but not webbing. It is caused by Trisomy 21.
Klinefelter’s syndrome is caused by having an extra X chromosome. They are often tall in stature with small testes and gynaecomastia. They do not tend to have the dysmorphic features.
Fragile X syndrome is due to a CGG repeat on the X chromosome. They tend to have learning difficulties, long ears, mitral valve prolapse and a large forehead and jaw.
Patau’s syndrome is caused by trisomy 13. They do tend to have intrauterine growth restriction leading to low birth weight, and can have congenital heart defects and ear abnormalities. However, they do not have webbing of the neck, and eye dysmorphic features tend to be microphthalmia or anophthalmia. They typically have rocker bottom feet and polydactyly.
Features of Turner’s syndrome
45XO
Short stature
Shield chest, widely spaced nipples
Webbed neck
Cardiac: bicuspid aortic valve, coarctation
Primary amenorrhoea
Cystic hygroma
High-arched palate
Short fourth metacarpal
Multiple pigmented naevi
Lymphoedema
Increased incidence of autoimmune disease: thyroiditis and Crohn’s especially
A 2 year old boy presents to the GP with his mother. She is worried that he is not growing at the same rate as the other children at his play group. His mother describes foul smelling diarrhoea about 4-5 times a week, accompanied by abdominal pain.
On examination he has a bloated abdomen and wasted buttocks. He has dropped 2 centile lines and now falls on the 10th centile.
What is the most appropriate initial investigation?
Stool sample
IgA TTG antibodies
Hydrogen breath test
Endoscopy
Abdominal xray
The most likely diagnosis here is coeliac disease, diagnosed using IgA TTG antibodies, as explained below.
A stool sample would be diagnostic for gastroenteritis, in order to dictate which antibiotic should be used.
The hydrogen breath test is used to diagnose irritable bowel syndrome or some food intolerances.
Endoscopy is more commonly used in adults where cancer is suspected.
An abdominal X-ray may be useful where obstruction is suspected.
Coeliac disease is a digestive condition which is becoming increasingly common, and describes an adverse reaction to gluten. gluten is a protein found in wheat, barley and rye.
Coeliac disease in children
Coeliac disease is caused by sensitivity to the protein gluten. Repeated exposure leads to villous atrophy which in turn causes malabsorption. Children normally present before the age of 3 years, following the introduction of cereals into the diet
Which HLAs are associated with coeliac?
HLA-DQ2 (95%)
HLA-B8 (80%)
Features of coeliac in children?
May coincide with the introduction of cereals
FTT
Diarrhoea
Abdominal distension
Older children may present with anaemia
May not be dxed until adulthood

Villous atrophy- Coeliac
Duodenal biopsy from a patient with coeliac disease. Complete atrophy of the villi with flat mucosa and marked crypt hyperplasia. Intraepithelial lymphocytosis. Dense mixed inflammatory infiltrate in the lamina propria.

Turner syndrome
45XO
Hirschprung’s features
Hirschsprung’s disease is caused by an aganglionic segment of bowel due to a developmental failure of the parasympathetic Auerbach and Meissner plexuses. Although rare (occurring in 1 in 5,000 births) it is an important differential diagnosis in childhood constipation
Possible presentations
neonatal period e.g. failure or delay to pass meconium
older children: constipation, abdominal distension
Associations
3 times more common in males
Down’s syndrome
Klumpke’s palsy
Klumpke’s palsy occurs due to damage of the lower brachial plexus and commonly affects the nerves innervating the muscles of the hand.
Erb’s palsy
Erb’s palsy occurs due to damage to the upper brachial plexus most commonly from shoulder dystocia. Damage to these nerve roots results in a characteristic pattern: adduction and internal rotation of the arm, with pronation of the forearm. This classic physical position is commonly called the ‘waiter’s tip’.
A male child from a travelling community is diagnosed with measles. Which one of the following complications is he at risk from in the immediate aftermath of the initial infection?
Arthritis
Pancreatitis
Infertility
Subacute sclerosing panencephalitis
Pneumonia
Subacute sclerosing panencephalitis is seen but develops 5-10 years following the illness. Pancreatitis and infertility may follow mumps infection
Pneumonia
Measles overview
Overview
RNA paramyxovirus
spread by droplets
infective from prodrome until 4 days after rash starts
incubation period = 10-14 days
Measles clinical features
Prodrome: irritable, conjunctivitis, fever
Koplik spots: grains of salt, on buccal mucosa
Rash: starts behind ears, then to whole body, discrete maculopapular rash becoming blotchy and confluent

Measles

Koplik spots
Pre-measles rash on buccal mucosa
Cxs of measles
encephalitis: typically occurs 1-2 weeks following the onset of the illness)
subacute sclerosing panencephalitis: very rare, may present 5-10 years following the illness
febrile convulsions
giant cell pneumonia
keratoconjunctivitis, corneal ulceration
diarrhoea
increased incidence of appendicitis
myocarditis
Mx of measles contacts
if a child not immunized against measles comes into contact with measles then MMR should be offered (vaccine-induced measles antibody develops more rapidly than that following natural infection)
this should be given within 72 hours
Def: nephrotic syndrome
Nephrotic syndrome is classically defined as a triad of
proteinuria (> 1 g/m^2 per 24 hours)
hypoalbuminaemia (< 25 g/l)
oedema
Nephrotic syndrome in children
In children the peak incidence is between 2 and 5 years of age. Around 80% of cases in children are due to a condition called minimal change glomerulonephritis. The condition generally carries a good prognosis with around 90% of cases responding to high-dose oral steroids.
Other features include hyperlipidaemia, a hypercoagulable state (due to loss of antithrombin III) and a predisposition to infection (due to loss of immunoglobulins)
Features of acute epiglottitis
Acute epiglottitis is rare but serious infection caused by Haemophilus influenzae type B. Prompt recognition and treatment is essential as airway obstruction may develop. Epiglottitis was generally considered a disease of childhood but in the UK it is now more common in adults due to the immunisation programme. The incidence of epiglottitis has decreased since the introduction of the Hib vaccine
Clinical features of epiglottits
Features
rapid onset
high temperature, generally unwell
stridor
drooling of saliva
Develpmental milestones
social behaviour
6w
Smiles
(Refer at 10w)
Develpmental milestones
social behaviour
3m
Laughs
Enjoys friendly handling
Develpmental milestones
social behaviour
6m
Not shy
Develpmental milestones
social behaviour
9m
Shy
Developmental milestones: feeding
6m
May put hand on bottle when being fed
Developmental milestones: feeding
12-15m
Drinks from cup and uses spoon
Developmental milestones: feeding
2y
Competent with sppon, doesn’t spill cup
Developmental milestones: feeding
3y
Uses spoon and fork
Developmental milestones: dressing
12-15m
Helps getting dress/undressed
Developmental milestones: dressing
18m
Takes of shoes, hat but unable to replace
Developmental milestones: dressing
2y
Puts on hat and shoes
Developmental milestones: dressing
4y
Can dress and undress independently except for laces and buttons
Developmental milestones: play
9m
Peek a boo
Developmental milestones: play
12m
Waves bye bye
Plays pat a cake
Developmental milestones: play
18m
Plays contentedly alone
Developmental milestones: play
2y
Plays near others, not with them
Developmental milestones: play
4y
Plays with other children
A 7-year-old boy is brought in to the GP surgery with an exacerbation of asthma. On examination he has a bilateral expiratory wheeze but there are no signs of respiratory distress. His respiratory rate is 36 / min and PEF around 60% of normal. What is the most appropriate action with regards to steroid therapy?
Oral prednisolone for 3 days
Admit for intravenous steroids
Give a stat dose of oral dexamethasone
Double his usual beclometasone dose
Do not give steroids
Oral prednisolone for 3 days
2-5y/o Asthma
Moderate attack
SpO2 >92%
No clinical features of severe asthma
2-5y/o Asthma
Severe attack
SpO2 <92%
Too breathless to talk or feed
HR >140
RR >40
Use of accessory neck muscles
2-5y/o Asthma
Life-threatening attack
SpO2 <92%
Silent chest
Poor respiratory effort
Agitation
Altered consciousness
Cyanosis
>5y/o Asthma
Moderate attack
SpO2 >92%
PEF >50% predicted
No clinical features of severe asthma
>5y/o Asthma
Severe attack
SpO2 <92
PEF 33-50
Can’t complete sentences in one breath or too breathless to talk or feed
HR >125
RR >30
Use of accessory neck muscles
>5y/o Asthma
Life-threatening attack
SpO2 <92
PEF <33
Silent chest
Poor respiratory effort
Altered consciousness
Cyanosis
PEF in children
Attempt to measure in all children >5
Mx of mild-moderate acute asthma
Bronchodilator:
Beta-2 agonist via a spacer (<3y use a close-fitting mask)
1 puff every 15-30secs, up to a maximum of 10 puffs, repeat dose after 10-20 mins if necessary
If symptoms are not controlled, repeat beta-2 and refer to hospital
Steroid therapy:
should be given to all children with asthma exacerbation
Treatment for 3-5d
Prednisolone dose
2-5y
>5y
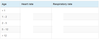
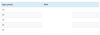
Age Dose as per BTS Dose as per cBNF
2 - 5 years 20 mg o d1-2 mg/kg od (max 40mg)
> 5 years 30 - 40 mg od 1-2 mg/kg od (max 40mg)
A 9-year-old boy is brought to surgery with recurrent headaches. What is the most common cause of headaches in children?
Migraine
Depression
Refractive errors
Tension-type headache
Cluster headache
Migraine
Features of Hand foot and mouth disease?:
Hand, foot and mouth disease is a self-limiting condition affecting children. It is caused by the intestinal viruses of the Picornaviridae family (most commonly coxsackie A16 and enterovirus 71). It is very contagious and typically occurs in outbreaks at nursery
Clinical features
mild systemic upset: sore throat, fever
oral ulcers
followed later by vesicles on the palms and soles of the feet
Mx of hand foot and mouth?
Management
general advice about hydration and analgesia
reassurance no link to disease in cattle
children do not need to be excluded from school*
*The HPA recommends that children who are unwell should be kept off school until they feel better. They also advise that you contact them if you suspect that there may be a large outbreak.

Hand foot and mouth disease
Features of Croup?
Croup is a form of upper respiratory tract infection seen in infants and toddlers. It is characterised by stridor which is caused by a combination of laryngeal oedema and secretions. Parainfluenza viruses account for the majority of cases.
Epidemiology
peak incidence at 6 months - 3 years
more common in autumn
Features
stridor
barking cough (worse at night)
fever
coryzal symptoms
Features of mild croup
Occasional barking cough
No audible stridor at rest
No or mild suprasternal and or intercostal recession
Child is happy and is prepared to eat, drink and play
Features of moderate croup
Frequent barking cough
Easily audible stridor and rest
Suprasternal and sternal wall retraction at rest
No or little distress or agitation
Child can be placated
Features of severe croup
Frequent barking cough
Prominent inspiratory and occasionally expiratory stridor at rest
Marked sternal wall retractions
Significant distress and agitation or lethargy or restlessness (sign of hypoxaemia)
Tachycardia occurs with more sever obstructive symptoms and hypoxaemia
Indications for admission in croup
Moderate or severe croup
<6m
Known upper airway abnormality e.g. laryngomalacia, DS
Uncertainty about ddx (acute epiglottitis, bacterial tracheitis, peritonsillar abscess, FBI)
Mx of croup
Single dose of oral dexamethasone (0.15mg/kg)
Emergency:
High flow O2
Nebulised adrenaline
The parents of a 14-month-old girl present to their GP. They have noticed that in some photos there is no ‘red eye’ on the left hand side. When you examine the girl you notice an esotropic strabismus and a loss of the red-reflex in the left eye. There is a family history of a grandparent having an enucleation as a child. What is the most likely diagnosis?
Congenital hypertrophy of the retinal pigment epithelium
Uveal malignant melanoma
Neuroblastoma
Retinoblastoma
Congenital cataract
A congenital cataract may cause a loss of the red-reflex but is likely to have been detected at birth or during the routine baby-checks. It would also not explain the family history of enucleation.
Retinoblastoma
Features of retinoblastoma
Retinoblastoma is the most common ocular malignancy found in children. The average age of diagnosis is 18 months.
Pathophysiology
caused by a loss of function of the retinoblastoma tumour suppressor gene on chromosome 13
around 10% of cases are hereditary
Possible features
absence of red-reflex, repalced by a white pupil (leukocoria) - the most common presenting symptom
strabismus
visual problems
Mx of retinoblastoma
Management
enucleation is not the only option
depending on how advanced the tumour is other options include external beam radiation therapy, chemotherapy and photocoagulation
Prognosis
excellent, with > 90% surviving into adulthood
Draw management of asthma in children under 5

Draw management of asthma in children >5

What is the major risk factor for NRDS?
Prematurity
What is the major risk factor for TTN?
C-sec
What is the major risk factor for aspiration pneumonia?
Meconium staining
What differentiates between NRDS and TTN?
Neonates with NRDS usually present with respiratory distress shortly after birth which usually worsens over the next few days. In contrast, TTN usually presents with tachypnoea shortly after birth and often fully resolves within the first day of life. A chest radiograph can be useful
CXR in NRDS?
Diffuse ground glass lungs
Low volumes
Bell shaped throax

NRDS
CXR in TTN
Heart failure type pattern
Intersitital oedema
PLeural effusions
But normal heart size in contrast to congenital heart disease

TTN
Features of Surfactant lung disease?
Surfactant deficient lung disease (SDLD, also known as respiratory distress syndrome and previously as hyaline membrane disease) is a condition seen in premature infants. It is caused by insufficient surfactant production and structural immaturity of the lungs
The risk of SDLD decreases with gestation
50% of infants born at 26-28 weeks
25% of infants born at 30-31 weeks
Other risk factors for SDLD include
male sex
diabetic mothers
Caesarean section
second born of premature twins
Clinical features are those common to respiratory distress in the newborn, i.e. tachypnoea, intercostal recession, expiratory grunting and cyanosis
Chest x-ray characteristically shows ‘ground-glass’ appearance with an indistinct heart border
Mx of SDLD?
Management
prevention during pregnancy: maternal corticosteroids to induce fetal lung maturation
oxygen
assisted ventilation
exogenous surfactant given via endotracheal tube
How can primary, secondary and tertiary preventative measures be classified?
Preventive healthcare can be divided up into primary (preventing the accident/disease from happening), secondary (prevent injury from the accident/disease) and tertiary (limit the impact of the injury) prevention strategies
Contraindications to IFV immunisation in children?
Contraindications
immunocompromised
aged < 2 years
current febrile illness or blocked nose/rhinorrhoea
current wheeze (e.g. ongoing viral-induced wheeze/asthma) or history of severe asthma (BTS step 4)
egg allergy
pregnancy/breastfeeding
if the child is taking aspirin (e.g. for Kawasaki disease) due to a risk of Reye’s syndrome
A mother is concerned about the risk of her son developing influenza. Her son is fit and otherwise well. Following NHS immunisation guidance, at what age should the child first be offered the influenza vaccine?
3 months
4 months
12-13 months
2-3 years
65 years
2-3y
Suggestigve of constipation (>=2)
Stool pattern in Child
<1y
Fewer than 3 complete stools per week
hard large stool
Rabbit droppings
Stool pattern suggestigve of constipation (>=2)
>1y
Fewer than 3 complete stools per week
Overflow soiling (commonly very loose, very smelly and passed without sensation)
Rabbit droppings
Large, infrequent stools that can block toilet
Symptoms associated with defecation suggestigve of constipation (>=2)
<1y
Distress on passing stool
Bleeding associated with hard stool
Straining
Symptoms associated with defecation suggestigve of constipation (>=2)
>1y
Poor appetite that improves with passage of large stool
Waxing and waning of abdo pain with passage of stool
Evidence of tenetive posturing
Straining
Anal pain
Retentive posturing in examination?
Typical straight legged, tip toed, back arching
Hx suggestigve of constipation (>=2)
<1y
Previous episode of constipation
Previous or current anal fissure
Hx suggestigve of constipation (>=2)
>1y
Previous epsiode
Previous or currrent anal fissure
Painful BM and bleeding associated with hard stools
Causes of constipation
Idiopathic
Dehydration
Diet
Medication e.g. opiates
Anal fissure
Over-enthusiastic potty training
Hypothyroidism
Hirschsprung’s
Hypercalcaemia
LD
What timing indicates idiopathic constipation?
Starts after a few weeks of life
Obvious precipitating factors coinciding with the start of symptoms: fissure, change of diet, timing of potty/toilet training or acute events such as infections, moving house, starting nursery/school, fears and phobias, major change in family, taking medicines
What is a red flag in constipation relating to timing?
Reported from birth or first few weeks of life
Passage of meconium in idiopathic constipation?
<48h
Red flag in meconium passage?
>48h
Ribbon stools?
?Hirschprungs
Faltering growth in constipation?
Amber flag
Growth in idiopathic sontipation
Generally well
Weight and height within normal limits, fit and active
Red flag in constipation
Previously unkown or undiagnosed weakness in legs, locomotr delay
Improtant determinant in idiopathic constipation?
Changes in infant formula
Weaning
Insufficient fluid intake or poor diet
Abdominal distension in constipation?
Red flag symptom suggestive of underlying disorder
What features suggest fecal impaction?
Symptoms of severe constipation
Overflow soiling
Faecal mass palpable in abdomen (DRE should only be performed by specialist)
Mx of feacal impaction
Polyethylene glycoe 3350 + electroyles (using an escalating dose) is first line
Stimulant laxative can be addied if first line does not lead to disimpaction after 2 weeks.
Subsititue a stimulant laxative singly or in combination with an osmotic laxative such as lactulose if Movicol Paediatric plan is not tolerated.
Inform families that disimpaction treatment can initially increase symptoms of soiling and abdominal pain
What type of laxative is Movicol Plain?
Osmotic
Eg of a stimulant laxative?
Senna
Maintenance therapy in constipation
very similar to the above regime, with obvious adjustments to the starting dose, i.e.
first-line: Movicol Paediatric Plain
add a stimulant laxative if no response
substitute a stimulant laxative if Movicol Paediatric Plain is not tolerated. Add another laxative such as lactulose or docusate if stools are hard
continue medication at maintenance dose for several weeks after regular bowel habit is established, then reduce dose gradually
What type of laxative is lactulose?
Osmotic
Bulk forming laxatives?
ispaghula psyllium) husk, methylcellulose and sterculia
Osmotic laxatives
lactulose, macrogols, phosphate enemas and sodium citrate enemas.
Stimulant laxatives.
bisacodyl, docusate sodium, glycerol, senna andsodium picosulfate
General points in Mx of constipation?
General points
do not use dietary interventions alone as first-line treatment although ensure child is having adequate fluid and fibre intake
consider regular toileting and non-punitive behavioural interventions
for all children consider asking the Health Visitor or Paediatric Continence Advisor to help support the parents.
Mx of infants not yet weaned with constipation
bottle-fed infants: give extra water in between feeds. Try gentle abdominal massage and bicycling the infant’s legs
breast-fed infants: constipation is unusual and organic causes should be considered
Mx of infants with constipation that have or are being weaned
Infants who have or are being weaned
offer extra water, diluted fruit juice and fruits
if not effective consider adding lactulose
Exacerbations of chronic bronchitis
Amoxicillin or tetracycline or clarithromycin
Uncomplicated community-acquired pneumonia
Amoxicillin (Doxycycline or clarithromycin in penicillin allergic, add flucloxacillin if staphylococci suspected e.g. In influenza)
Pneumonia possibly caused by atypical pathogens
Clarithromycin
Hospital-acquired pneumonia
Within 5 days of admission: co-amoxiclav or cefuroxime
More than 5 days after admission: piperacillin with tazobactam OR a broad-spectrum cephalosporin (e.g. ceftazidime) OR a quinolone (e.g. ciprofloxacin)
Lower urinary tract infection
Trimethoprim or nitrofurantoin. Alternative: amoxicillin or cephalosporin
Acute pyelonephritis
Broad-spectrum cephalosporin or quinolone
Acute prostatitis
Quinolone or trimethoprim
Impetigo
Topical fusidic acid, oral flucloxacillin or erythromycin if widespread
Cellulitis
Flucloxacillin (clarithromycin or clindomycin if penicillin-allergic)
Erysipelas
Phenoxymethylpenicillin (erythromycin if penicillin-allergic)
Animal or human bite
Co-amoxiclav (doxycycline + metronidazole if penicillin-allergic)
Mastitis during breast-feeding
Flucloxacillin
Throat infections
Phenoxymethylpenicillin (erythromycin alone if penicillin-allergic)
Sinusitis
Amoxicillin or doxycycline or erythromycin
Otitis media
Amoxicillin (erythromycin if penicillin-allergic)
Otitis externa*
Flucloxacillin (erythromycin if penicillin-allergic)
*a combined topical antibiotic and corticosteroid is generally used for mild/moderate cases of otitis externa
Gonorrhoea
Intramuscular ceftriaxone + oral azithromycin
Chlamydia
Doxycycline or azithromycin
Pelvic inflammatory disease
Oral ofloxacin + oral metronidazole or intramuscular ceftriaxone + oral doxycycline + oral metronidazole
Syphilis
Benzathine benzylpenicillin or doxycycline or erythromycin
Bacterial vaginosis
Oral or topical metronidazole or topical clindamycin
Clostridium difficile
First episode: metronidazole
Second or subsequent episode of infection: vancomycin
Campylobacter enteritis
Clarithromycin
Salmonella (non-typhoid)
Ciprofloxacin
Shigellosis
Ciprofloxacin
Meningitis
Neonatal to 3 months
Group B Streptococcus: usually acquired from the mother at birth. More common in low birth weight babies and following prolonged rupture of the membranes
E. coli and other Gram -ve organisms
Listeria monocytogenes
Meningitis
1 month to 6 years
Neisseria meningitidis (meningococcus)
Streptococcus pneumoniae (pneumococcus)
Haemophilus influenzae
Meningitis
>6y
Neisseria meningitidis (meningococcus)
Streptococcus pneumoniae (pneumococcus)
Throat examination in Croup?
Should be avoided as it may precipitate airway obstruction
A newborn baby is transferred to the neonatal intensive care unit shortly after birth due to respiratory distress. An x-ray taken on arrival is shown below:
What is the diagnosis?
Bronchopulmonary dysplasia
Respiratory distress syndrome
Left-sided neonatal bronchiectasis
Congenital diaphragmatic hernia
Left pneumothorax

Bowel loops can be seen in the left side of the thoracic cavity.
Features of congenital diaphragmatic hernia
Occurs in 1:2000
Characterised by the herniation of abdominal viscera into the chest cavity due to incomplete formation of the diaphragm
Can result in pulmonary hypoplasia and HTN which causes RDS shortly after birth
Px for congenital diaphramatic hernia
50% survive despite intervention
What is the most common type of congenital diaphramatic hernia?
Bochdalek hernia
85% cases
Left sided, posterolateral
Features of:
Chickenpox
Fever initially
Rash starting on head/trunk before spreading
Initially macular, then papular, then vessciular
Normally mild systemic upset

Chicken pox
Features of measles
Prodrome: irritable, conjuncitivits, fever
Koplik spots
Rash starting behind ears, spreading to the whole body
Initially discrete maculopapular rash that becomes blotchy and confluent
Features of mumps
Fever, malaise, muscular pain
Parotitis initially unilateral becoming bilateral in 70%
Features of Rubella
Pink maculopapular rash initially on face before spreading to the whole body, usually faind by the 3-5th day
Suboccipital and postauricular lymphadenopathy

Rubella
Features of erythema infectiosum
AKA slapped cheek syndrome
Caused by parvovirus B19
Lethargy, fever, headache
Slapped cheek rash spreading to proximal arms and extensor surfaces

Erythema infectiosum
Features of Scarlet fever
Reaction to erythrogenci toxins produced by group A haemolytic strep
Fever, malaise, tonsilitis
Strawberry tongue
Fine punctate erythema sparing face

Scarlet Fever
Features of hand, foot and mouth disease
Caused by coxsackie A16 virus
Mild systemic upset: sore throat, fever
Vesciles in the mouth and on the palms and soles of the feet

Hand foot and mouth
Scarlet fever features
Scarlet fever is a reaction to erythrogenic toxins produced by Group A haemolytic streptococci (usually Streptococcus pyogenes). It is more common in children aged 2 - 6 years with the peak incidence being at 4 years.
Scarlet fever has an incubation period of 2-4 days and typically presents with:
fever
malaise
tonsillitis
‘strawberry’ tongue
rash - fine punctate erythema (‘pinhead’) which generally appears first on the torso and spares the face although children often have a flushed appearance with perioral pallor. The rash often has a rough ‘sandpaper’ texture. Desquamination occurs later in the course of the illness, particularly around the fingers and toes
Dx of scarlet fever
Throat swab usually taken but antibiotic treatment should be commenced immediately
Mx of scarlet fever
Oral penicillin V (penallergic: azithromycin)
Children can return to school 24h after commencing antibiotics
Notifiable disease
Cx of Scarlet fever?
Otitis media: most common
Rheumatic fever: typically 20d after infection
Acute GN
Autosomal recessive conditions
Autosomal recessive conditions are often thought to be ‘metabolic’ as opposed to autosomal dominant conditions being ‘structural’, notable exceptions:
some ‘metabolic’ conditions such as Hunter’s and G6PD are X-linked recessive whilst others such as hyperlipidemia type II and hypokalemic periodic paralysis are autosomal dominant
some ‘structural’ conditions such as ataxia telangiectasia and Friedreich’s ataxia are autosomal recessive
Inheritance:
Albinism
AR
Inheriance:
Congenital adrenal hyperplasia
AR
Inheritance:
Ataxia telangiectasia
AR
Inehritance: Familial Mediterranean fever
AR
Inheritance: Fanconi anaemia
AR
Inheritance: Friedreichs ataxia
AR
Inheritance: Gilber’ts
AR (although some textbooks will still say AD)
Glycogen storage disease inheritance
AR
Hamochromatosis inheritance
AR
Homocystinuria inheritance
AR
Lipid storage disease: Tay-Sach’s, Gaucher, Niemann-Pick
Inheritance
AR
Mucopolysaccharidoses: Hurler’s
Inheritance
AR
PKU inheritance
AR
Sickle cell inheritance
AR
Thalassaemia inheritance
AR
Wilson’s inheritance
AR
Characteristic symptoms in ADHD?
Extreme restlessness
Poor concentration
Uncontrolled activity
Impusliveness

Patau syndrome (trisomy 13)
Microcephalic, small eyes
Cleft lip/palate
Polydactyly
Scalp lesions
Edward’s syndrome (trisomy 18)
Micrognathia
Low-set ears
Rocker bottom feet
Overlapping of fingers
Fragile X
Learning difficulties
Macrocephaly
Long face
Large ears
Macro-orchidism
Noonan syndrome
Webbed neck
Pectus excavatum
Short stature
Pulmonary stenosis
Pierre-Robin syndrome*
*this condition has many similarities with Treacher-Collins syndrome. One of the key differences is that Treacher-Collins syndrome is autosomal dominant so there is usually a family history of similar problems
Micrognathia
Posterior displacement of the tongue (may result in upper airway obstruction)
Cleft palate
Prader-Willi syndrome
Hypotonia
Hypogonadism
Obesity
William’s syndrome
Short stature
Learning difficulties
Friendly, extrovert personality
Transient neonatal hypercalcaemia
Supravalvular aortic stenosis
Short stature
Learning difficulties
Friendly, extrovert personality
Transient neonatal hypercalcaemia
Supravalvular aortic stenosis
William’s syndrome
Hypotonia
Hypogonadism
Obesity
Prader-Willi syndrome
Micrognathia
Posterior displacement of the tongue (may result in upper airway obstruction)
Cleft palate
Pierre-Robin syndrome*
Webbed neck
Pectus excavatum
Short stature
Pulmonary stenosis
Noonan syndrome
Learning difficulties
Macrocephaly
Long face
Large ears
Macro-orchidism
Fragile X
Micrognathia
Low-set ears
Rocker bottom feet
Overlapping of fingers
Edward’s syndrome (trisomy 18)
Microcephalic, small eyes
Cleft lip/palate
Polydactyly
Scalp lesions
Patau syndrome (trisomy 13)
What is the difference between primary, secondary and tertiary prevention strategies?
Preventive healthcare can be divided up into primary (preventing the accident/disease from happening), secondary (prevent injury from the accident/disease) and tertiary (limit the impact of the injury) prevention strategies
What is the most common cause of childhood death in 1-15y/o?
Accidents
What Ixs should be performed in infants <3m old with fever?
FBC
Blood culture
CRP
Urine dip
CXR if respiratory signs are present
Stool culture if diarrhoea is present
What causes head lice?
Pediculosis capitis
What is the dx of head live?
Treatment only if living lice found
Malathion, wet combing, dimeticone, isopropyl myristate and cyclomethicone.
School exclusion is not advised
HAP Rx
Within 5d of admission: co amoxiclav or cefuroxime
>5d: piperacilline with tazobactam OR a broad-spectrum cephalosporin OR a quinolone
(provides pseudomonas cover)
Risk of DS by maternal age?
One way of remembering this is by starting at 1/1,000 at 30 years and then dividing the denominator by 3 (i.e. 3 times more common) for every extra 5 years of age

What 3 features must be present to dx autism?
All 3 of the following features must be present for a diagnosis to be made
global impairment of language and communication
impairment of social relationships
ritualistic and compulsive phenomena
What syndromes are assocaited with autism?
Fragile X
Rett’s
What are hte criteria for admission in bronchiolitis?
Apnoea (observed or reported)
Persistent oxygen saturation of <92% in air
Inadequate oral fluid intake (<50% of normal fluid intake)
Persisting severe respiratory distress, for example grunting, marked chest recession, or a respiratory rate of over 70 breaths/minute.
Ix of bronchiolitis?
Can be done using fluorescent Ab test on nasopharyngeal secretions
Mx of RSV
Admit if fulfils criteria
Deliver humidifed oxygen best through head box. Level can be determiend with pulse oximetry.
Fluids and feed may need to be given by NG tube or IV.
Only 5% require venitlation.
What is the most common cause of food poisoning in the UK?
Campylobacter.
<5y/o and >60 y/o are at greater risk
Features of campylobacter
Campylobacter is the commonest bacterial cause of infectious intestinal disease in the UK. The majority of cases are caused by the Gram-negative bacillus Campylobacter jejuni. It is spread by the faecal-oral route and has an incubation period of 1-6 days.
Features
prodrome: headache malaise
diarrhoea: often bloody
abdominal pain
Mx of Campylobacter
Usually self-limiting
BNF advises antibiotics if immunocompromised. CKS also advise antibiotics if severe symptoms (high fever, bloody diarrhoea, >8 stools/d).
First line antibiotic is clarithromycin
Cxs of campylobacter infection
GB syndrome
Reiter’s syndrome
Septicaemia, endocarditis, arthritis
A 2-year-old girl is brought to her GP because her mother has noticed she is constantly itching her bottom at night. Her mother says she has noticed some strange looking white bits when she wipes her daughters bottom following a bowel motion. What is the most appropriate management option?
Prescribe 14 days of daily miconazole for whole household and issue hygiene advice.
Issue hygiene advice only.
Prescribe a single dose of mebendazole for the daughter and issue hygiene advice.
Prescribe a single dose of mebendazole for the whole household and issue hygiene advice.
Prescribe topical clotrimazole for 2 weeks and issue hygiene advice.
This child is highly likely to have a threadworm infection with symptoms of perianal itching that is worse at night. It is also possible to see threadworms, described as small threads of slowly-moving white cotton either around the anus or in the stools.
The risk of transmission in families is as high as 75%, and asymptomatic infestation is common. For this reason an anthelmintic drug (mebendazole) should be given as a single dose to all household members.
Features of threadworm infection
Asymptomactic in 90%
Perianal itching, particulrly at night.
Girls may have vulval symptoms.
Dx can be made by applyoing sellotape to the perianal area and sending it to the laboratory for microscopy to identify the eggs.
First line antihelmintic for children >6m
mebendazole
Paediatric PLS
Unresponsive
Help
Open airway
Look, listen, feel for breathing
5 rescue breaths
Circulation?
15 chest compressions:2
What are hte contraindications to the MMR?
severe immunosuppression
allergy to neomycin
children who have received another live vaccine by injection within 4 weeks
pregnancy should be avoided for at least 1 month following vaccination
immunoglobulin therapy within the past 3 months (there may be no immune response to the measles vaccine if antibodies are present)
Adverse affects of the MMR
malaise, fever and rash may occur after the first dose of MMR. This typically occurs after 5-10 days and lasts around 2-3 days
A mother comes to surgery with her 6-year-old son. During the MMR scare she decided not to have her son immunised. However, due to a recent measles outbreak she asks if he can still receive the MMR vaccine. What is the most appropriate action?
Arrange for measles immunoglobulin to be given
Cannot vaccinate at this age as live vaccine
Give separate measles vaccine
Give MMR with repeat dose in 3 months
Give MMR with repeat dose in 5 years
The Green Book recommends allowing 3 months between doses to maximise the response rate. A period of 1 month is considered adequate if the child is greater than 10 years of age. In an urgent situation (e.g. an outbreak at the child’s school) then a shorter period of 1 month can be used in younger children.
Transient synovitis
Acute onset
Usually accompanies viral infections, but the child is well or has a mild fever
More common in boys, aged 2-12 years
Septic arthritis/osteomyelitis
Unwell child, high fever
Juvenile idiopathic arthritis
Limp may be painless
Trauma
History is usually diagnostic
Development dysplasia of the hip
Usually detected in neonates
6 times more common in girls
Perthes disease
More common at 4-8 years
Due to avascular necrosis of the femoral head
Slipped upper femoral epiphysis
10-15 years - Displacement of the femoral head epiphysis postero-inferiorly
Criteria for admission in sickle cell crisis?
Admit all people with clinical features of a sickle cell crisis to hospital unless they are:
A well adult who only has mild or moderate pain and has a temperature of 38°C or less.
A well child who only has mild or moderate pain and does not have an increased temperature.
This is based on the recommendation that a fever with no identified source associated with a sickle cell crisis needs bloods and cultures taken to look for the possible source of infection and early treatment as there is a higher risk of severe infections due to hyposplenism.
Consider admission if the person presents with a fever but is otherwise generally well.
Admission is not necessarily required if the source of infection is obvious (such as a viral illness) and can be managed in the community.
Have a low threshold for admission:
In a child.
If the person has a temperature over 38°C (as there is a risk of rapid deterioration).
If the person has chest symptoms (as acute chest syndrome may develop quickly).
Make sure that the person with chest symptoms and their family understand the importance of seeking urgent medical advice if their clinical state deteriorates, especially if breathing becomes faster or more laboured.
Whenever possible, admit the person to the specialist centre that has their records.
Management of sickle cell crises
Analgesia: opiates
Rehydrate
O2
Consider
antibiotics
Blood transfusion
Exchange transfusion e.g. if neurological complications
How can hypotonia be classified?
May be central or related to nerve and muscle problems.
Acutely ill child e.g. septicaemia may also be hypotonic on examination.
Hypotonia associated with encephalopathy in the newborn period is most likely caused by hypoxic ischaemic encephalopathy
Central causes of hypotonia?
DS
Prader Willi
Hypothyroid
Cerebal palsy- hypotonia may preced the development of spasticity
Neurological and muscular causes of hypotonia
Spinal muscular atrophy
Spina bifida
GB syndrome
MG
Muscular dystrophy
Myotonic dystrophy
myotonic dystrophy
Myotonic dystrophy (dystrophia myotonica, myotonia atrophica) is a chronic, slowly progressing, highly variable, inherited multisystemicdisease. It is an autosomal-dominant disease.It is characterized by wasting of the muscles (muscular dystrophy), cataracts, heart conduction defects, endocrine changes, and myotonia.[1]
There are two main types of myotonic dystrophy. Myotonic dystrophy type 1 (DM1), also called Steinert disease, has a severe congenital form and an adult-onset form. Myotonic dystrophy type 2 (DM2), also called proximal myotonic myopathy (PROMM) is rarer than DM1 and generally manifests with milder signs and symptoms. Myotonic dystrophy can occur in people of any age. Both forms of the disease display an autosomal-dominant pattern of inheritance. Both “DM1” and “DM2” have adult-onset forms.
Which one of the following statements regarding scabies is false?
All members of the household should be treated
Typically affects the fingers, interdigital webs and flexor aspects of the wrist in adults
Scabies causes a delayed type IV hypersensitivity reaction
Patients who complain of pruritus 4 weeks following treatment should be retreated
Malathion is suitable for the eradication of scabies
It is normal for pruritus to persist for up to 4-6 weeks post eradication
Features opf Scabies
Scabies is caused by the mite Sarcoptes scabiei and is spread by prolonged skin contact. It typically affects children and young adults.
The scabies mite burrows into the skin, laying its eggs in the stratum corneum. The intense pruritus associated with scabies is due to a delayed type IV hypersensitivity reaction to mites/eggs which occurs about 30 days after the initial infection.
Clinical features of scabies
Widespread prutirus
Linear burrows on the side of fingers, interdigital webs and flexor aspects of hte wrist.
Infants the face and scalp may be affected.
2o features are due to scratching excoriation, infection
Mx of scabies
Permethrin 5% is first line
Malathion is second line.
Guidance on use.
Pruritus persists 4-6w post eradication
When is crusted scabies seen?
Mx
Crusted scabies is seen in patients with suppressed immunity, especially HIV.
The crusted skin will be teeming with hundreds of thousands of organisms.
Ivermectin is the treatment of choice and isolation is essentia

Crusted (Norweigan) scabies
Risk factors for DDH
Female sex x6
Breech presentation
Positive Fhx
First born children
Oligohydramnios
Birthweight >5kg
Congenital calacenovalgus foot deformity
Barlow test
Barlow maneuver. (A) The leg is pulled forward and then (B) adducted in an attempt to dislocate the femur.
The Barlow test is a provocative maneuver used to diagnose a dislocatable hip. With the infant in a supine position, the hips are flexed to 90° and abducted. The thigh is grasped, and the leg is gently adducted while applying downward and lateral pressure (Fig 8A and B). A palpable clunk or movement indicates that the femoral head dislocates by sliding over the posterior rim of the acetabulum
Ortolani test
Ortolani maneuver. (A) Initial downward pressure further dislocates the hip, which then (B) relocates as the thigh is adducted. A palpable clunk will be noted
The Ortolani maneuver moves a dislocated hip back into the socket, creating a distinct, palpable sensation. To perform the Ortolani maneuver, place your index and middle fingers along the greater trochanter of the femur and your thumb along the inner thigh (Fig 7A and B). With the infant’s legs in a neutral position, flex the infant’s hips 90°. Gently abduct the hips while lifting forward on the femur. A positive Ortolani sign is noted if the hip is dislocated, by a characteristic clunk that is felt as the femoral head slides over the posterior rim of the acetabulum and is reduced
Confirmation of dx of DDH
USS
Mx of DDH
Most unstable hips will spontaneously stabilise by 3-6w
Pavlik harnesses in children younger than 3-5m
Older children may require sx
A 3-year-old girl presents with a 3 day history of fever and bloody diarrhoea. Over the past 24 hours she has had 5 episodes of loose bloody stools. On examination she has a temperature of 39.6ºC, a heart rate of 175 bpm and her abdomen is soft with generalised tenderness. It is also noted that she has a reduced urinary output. Blood tests show a haemolytic anaemia and raised urea.
What is the most likely diagnosis?
Campylobacter gastroenteritis
Salmonella gastroenteritis
Norovirus
Rotavirus
Escherichia coli gastroenteritis
A short history of bloody diarrhoea is very suggestive of haemorrhagic gastroenteritis which can occur due to a variety of pathogens including Campylobacter, Salmonella and Escherichia coli.
In this case, the haemolytic anaemia and raised urea suggest haemolytic uraemic syndrome. Haemolytic anaemia and renal failure form two parts of the classic triad of haemolytic uraemic syndrome. The third part of the triad is thrombocytopenia. It is usually caused by Escherichia coli subtype 0157. Treatment is supportive as antibiotics are contraindicated.
How can E Coli be classified?
`According to its antigens which may trigger an immune response
O: LPS
K: Capsule
H: Flagellin
What E Coli serotype usually causes Neonatal meningitis?
K-1 (capsular antigen)
A 9 year old boy is brought to the emergency department by ambulance. For approximately 24 hours he has had nausea and vomiting. However, he has now developed acute abdominal pain and when he arrives in the emergency department his breathing is laboured, deep and of a gasping nature. He is usually fit and well and is not prescribed any medication. Blood results show the following:
Na+130 mmol/l
K+3.5 mmol/l
HCO3-19 mmol/l
What is the likely cause?
Sepsis
Rotavirus
Intestinal obstruction
Meningitis
Diabetic ketoacidosis
The patient in this scenario has developed diabetic ketoacidosis (DKA). The important pieces of information to consider when answering this question are his acute presentation and the blood results.
This patient has presented to the emergency department with nausea, vomiting and acute abdominal pain. These are all symptoms of diabetic ketoacidosis. Furthermore, the laboured, deep breathing that is mentioned is Kussmaul’s breathing, which is witnessed in DKA and metabolic acidosis. Kussmaul’s breathing occurs whereby excess CO2 is exhaled as a compensatory mechanism for an increased blood pH. The recognition of Kussmauls breathing in this question is one of the major factors in getting this question correct, as you would not expect to see this phenomenon in the other 4 possible answers.
The blood results are concurrent with a diagnosis of DKA. Bloods will often show a hyponatraemia, low bicarbonate and a hypokalaemia in severe cases. The low bicarbonate in this question gives the indication that there is an acidosis in this patient, which helps in deriving the correct answer.
Taking into account all other answers, they each could explain some of the symptoms of this child. However, the low bicarbonate, his symptoms and Kussmaul’s respirations should lead to a working diagnosis of diabetic ketoacidosis in this patient.
Kussmaul’s breathing
laboured, deep breathing that is mentioned is Kussmaul’s breathing, which is witnessed in DKA and metabolic acidosis. Kussmaul’s breathing occurs whereby excess CO2 is exhaled as a compensatory mechanism for an increased blood pH
What are the most common precipitating factors for DKA?
Infection
Missed insulin
MI
Features of DKA
Abdo pain
Polyuria, polydipsia, dehydration
Kussmaul respiration
Acetone smelling breath
What are the causes of death in DKA?
Other complications?
Cerebral oedema
Hypokalaemia
Aspiration pneumonia
Hypoglycaemia
Hypokalaemia
Systemic infections
Appendicitis
Pulmonary oedema
Hyperosmolar hyperglycaemia non-ketotic coma
What are the criteria for DKA
Glucose >11 or known DM
pH <7.3
Bicarbonate <15mmol
Ketones >3mmol or ++ on dipstick
Mx of DKA
ABCD
Correct dehydration
Replace insulin
Replace potassium
Phosphate replacement
Anticoagulation
Once KA has resolved:
Continue IV fluids until patient is drinking and tolerating food
Change to subcut insuline once blood ketones <1mmol
Monitor until biochemistry has normalised
Correcting dehydration in DKA
Assess dehydration: ideally weigh patient.
Patients with <5% dehydration who are not clinically unwell can be given oral rehydration with subcut insulin.
If patient is severely dehydrated or schokled:
10ml/kg 0.9% saline as a bolus up to 30ml/kg
Calculate deficit and replace over 48h along with usual maintenance requirements using 500ml of 0.9% saline, initially contianing 20mmol KCl, which can be changed to 0.45% saline and 20mmol KCl once BG has fallen to 12-15 mmol
NB neonates may require larger volumes
Fluid replacement should be monitored as some patients may experience massive diuresis
Fluids in DKA
10ml/kg bolus 0.9% salin up to 30ml
Calculate deficit + maintenance
Over first 48h: 0.9% 500ml saline + 20mmol KCl until BG <15
Then 0.45% saline + 20mmol KCl
What can be used to clinically assess dehydration
CRT
Skin turgor
Respiratory pattern
Dry mucous membranes
Sunken eyes
Weak pulses
Cool peripheries
Hypotension and oliguria which are late signs in children
Mild dehydration
3%: only just clinically detectable
Moderate dehydration
5%: dry mucous membranes and reduced skin turgor
Severe dehydration
8%
As for 5% but with sunken eyes and prolonged CRT
Shocked in dehydration
Severely ill, with poor perfusion and thready rapid pulse
Hypotension is a late sign and is not always present
Replacing insulin in DKA
IV fluids and K replacement should occur 1-2h before starting.
Early insulin associated with increased chacnce of developing cerebral oedema
IV infusion at 0.1U/kg/h (can be 0.05U in younger children)
Aim is to reduce BG by <4mmol/h.
If the BG drops below 8mmol add a sideline of 10% glucose and titrate to 8-12mmol but do not decrease the insulin infusion.
Replacing K in DKA
Always depletion in total body potassium however initial serum values may not necessarily be low.
K replacement should be started if patient is hypokalaemic, if not it should be when insulin is started.
If the patient is hyperkalaemic, do not start replacement until U/O documented
Phosphate replacement in DKA
Phosphate loss can be aggravated by insulin therapy.
If associated with neurology, hypophosphataemia can be treated using K phosphate salts as an alternative to KCl
Anticoagulation in DKA
Femoral line insertion associated with femoral vein thrombosis and these patients must be anticoagulated.
May also be indicated in patients who are significantly hyperosmolar
Monitoring of DKA
Obs
Fluid blaance
ECG
CBG hourly
Capillary blood ketones 1-2hourly
Twice-daily weights
Bloods every 2-4hrs
Neurological investigations looking for indications of cerebral oedema.
Mx of suspected cerebral oedema
Mannitol 0.1-1g/kg IV immediately over 20 minutes.
Symptoms of cerebral oedema
Headache
Vomiting
Confusion or irritibaility
Rising BP and bradycardia
Decreased O2 saturation
Focal neurology
Papilloedema (late sign)
Risk factors for cerebral oedema
Younger age
New-onset DM
Longer duration of symptoms
Use of bicarbonate in management of KA
Treatment of cerebral oedema
Exclude hypoglycaemia
Mannitol
Reduce rate of fluid admin
Elevate head of the bed
Transfer to ICU
Cause of roseola infantum
AKA exanthem subitum
Common disease of infancy caused by HHV6.
Incubation period of 5-15d and affects children of 6m-2y
Features of roseola infantum
high fever: lasting a few days, followed by a
maculopapular rash
febrile convulsions occur in around 10-15%
diarrhoea and cough are also commonly seen
Potential complications of HHV6 infection
aseptic meningitis
hepatitis

Roseola infantum (HHV6)
Def: squint
Squint (strabismus) is characterised by misalignment of the visual axes. Squints may be divided into concomitant (common) and paralytic (rare)
Cause of concomitant squint
Due to imablance in extraocular muscles
Convergent is more common than divergent
Cause of paralytic squint
Due to paralysis of extraocular muscles
What is the corneal light reflection test
Used to identify squint
Hold light source 30cm from the child’s face
Mx of strabismus
Eye patches may prevent amblyopia
Referral to secondary care
Ambylopia
Amblyopia, also known as lazy eye, is a vision development disorder in which an eye fails to achieve normal visual acuity, even with prescription eyeglasses or contact lenses. Amblyopia begins during infancy and early childhood. In most cases, only one eye is affected.
What can be used to identify the nature of the squint
The cover test
Presentation of UTI in childhood
Infants: poor feeding, vomiting, irritability
Younger children: abdominal pain, fever, dysuria
Older: dysuria, frequency, haematuria
Features suggestive of upper UTI: T >38, loin pain/tenderness
Indications for checking urine in a nchild
Any symptoms suggestive
Unexplained fever of 38
Alternative site of infection who remain unwell
Collection of urine
Clean catch is preferrable
If not possible then urine colleciton pads should be used.
Suprapubic aspiration can be used if non-invasive methods are not possible
Mx of UTI
<3m: immediate referrl to paediatrirican
>3m with upper UT: consider admission, oral antibiotics including cephalosporin or co-amoxiclav should be given for 7-10m
Lower UTI: oral antibiotics for 3d according to local guidelines (trimethoprim, nitrofurantoin, cepahlosporin, amoxicillin)
Antibiotic prophylaxis not given after the first UTI but should be considered with recurrent UTIs
Features of seborrhoeic dermatitis
Seborrhoeic dermatitis is a relatively common skin disorder seen in children. It typically affects the scalp (‘Cradle cap’), nappy area, face and limb flexures.
Cradle cap is an early sign which may develop in the first few weeks of life. It is characterised by an erythematous rash with coarse yellow scales.
Mx of seborrhoeic dermatitis
Mild-moderate: baby shampoo and baby oils
Severe: mild topical steroids e.g. 1% hydrocortisone
Tends to resolve by 8m

Seborrhoeic dermatitis (cradle cap)
Def: anapylaxis
Anaphylaxis may be defined as a severe, life-threatening, generalised or systemic hypersensitivity reaction.
Causes of anaphylaxis in children
Common identified causes of anaphylaxis
food (e.g. Nuts) - the most common cause in children
drugs
venom (e.g. Wasp sting)
Dose in anaphylaxis
<6m
150microg adrenaline
25mg hydrocortisone
250ug/kg chlorphenamine
Dose in anaphylaxis
6m-6y
150microg adrenaline
50mg hydrocortisone
2.5mg chlorphenamine
Dose in anaphylaxis
6-12y
300 microg adrenaline
100mg hydrocortisone
5mg chlorphenamine
Dose in anaphylaxis
Adult and child >12
500ug adrenaline
200mg hydrocortisone
10mg chlorphenamine
Adrenaline in anaphylaxis
Can be repeated every 5 minutes if necessary
What is the best site for IM injection in children of adrenaline
Anterolateral aspect of the middle third of the thigh
Def: CMPI/CMPA
Cow’s milk protein intolerance/allergy (CMPI/CMPA) occurs in around 3-6% of all children and typically presents in the first 3 months of life in formula fed infants, although rarely it is seen in exclusively breastfed infants.
Both immediate (IgE mediated) and delayed (non-IgE mediated) reactions are seen. The term CMPA is usually used for immediate reactions and CMPI for mild-moderate delayed reactions.
Dx of cows milk protein intolerance/allergy
Often clinical (elimination of cow’s milk protein)
Skin prick/patch testing
Total IgE and specific IgE (RAST) for cow’s milk protein
Mx of cow’s milk protein intolerance/allergy
If FTT-> paediatirician
If formula fed:
Extensive hydrolysed formula milk is first line replacement for infants with mild-moderate symptoms
Amino-acid based formula in infants with severe CMPA or if no response to eHF
10% also intolerant to soy milk
If breast fed:
Continue breastfeeding
Eliminate cow’s milk protein from maternal diet
Use eHF milk when breast feeding stops until 12m of age and at least 6m
Usually resolves by 1-2y/o
Challenge often performed in hospital due to risk of anaphylaxis
A baby boy born 6 hours ago has an APGAR score of 10. He is not cyanosed, has a pulse of 140, cries on stimulation, his arms and legs resist extension and he has a good cry, He appears jaundiced. What is the most appropriate action?
Encourage the mother to sit with the baby in sunlight
Arrange a blood transfusion
Start phototherapy
Prescribe intravenous immunoglobulin
Measure and record the serum bilirubin level urgently.
Measure and record the serum bilirubin level urgently (within 2 hours) in all babies with suspected or obvious jaundice in the first 24 hours of life since this is likely to be pathological rather than physiological jaundice. NICE CG98
Jaundice <24h y/o
Always pathological
Causes of jaundice in the first 24h
Rhesus disease
ABO disease
Hereditary spherocytosis
G6PDD
Jaundice 2-14d
Common and usually physiological, commonly seen in breast fed babies
Causes of prolonged jaundice (>14d)
Biliary atresia
Hypothyroidism
Galactosaemia
HTI
Breast milk jaundice
Congenital infections e.g. CMV, toxoplasmosis
Raised conjugated bilirubin in prolonged jaundice?
Could indicate biliary atresia which requires urgent surgical intervention
Components of a prolonged jaundice screen
Conjugated and unconjugated bilirubin
DAAT
TFTs
FBC and blood film
urine for MC&S and reducing sugars
U&Es
LFTs
Features of growing pains
A common presentation in General Practice is a child complaining of pain in the legs with no obvious cause. Such presentations, in the absence of any worrying features, are often attributed to ‘growing pains’. This is a misnomer as the pains are often not related to growth - the current term used in rheumatology is ‘benign idiopathic nocturnal limb pains of childhood’
Growing pains are equally common in boys and girls and occur in the age range of 3-12 years.
Features of growing pains
never present at the start of the day after the child has woken
no limp
no limitation of physical activity
systemically well
normal physical examination
motor milestones normal
symptoms are often intermittent and worse after a day of vigorous activity
Daniel is a newborn who is having his baby check done by nurse Karen, who notices that he has microcephaly with a prominent occiput, low set ears, micrognathia, palpebral fissures and wide spaced eyes. What genetic disorder are these features suggestive of?
Edward’s syndrome
Down’s syndrome
Turner’s syndrome
Noonan syndrome
Angelman syndrome
The correct answer for this question is Edward’s syndrome.
All of the aforementioned characteristics can be present in Edward’s syndrome. Furthermore, individual’s with Edward’s syndrome can also have:
Ptosis
Rocker bottom feet
Undescended testes
Risk factors for SIDS
Most common at 3m of age
Prematurity
Parental smoking
Hyperthermia
Sleeping prone
Male sex
Multiple births
Bottle feeding
Social classes IV and V
Maternal drug use
Winter
Following cot death, siblings should be screened for potential sepsis and inborn errors of metabolism
Features of Achondroplasia
Achondroplasia is an autosomal dominant disorder associated with short stature. It is caused by a mutation in the fibroblast growth factor receptor 3 (FGFR-3) gene. This results in abnormal cartilage giving rise to:
short limbs (rhizomelia) with shortened fingers (brachydactyly)
large head with frontal bossing
midface hypoplasia with a flattened nasal bridge
‘trident’ hands
lumbar lordosis

Achondroplasia
Features of kawasaki’s disease
High-grade fever which lasts >5d and is characteristically resistant to antipyretics
Conjunctival injection
Bright red, cracked lips
Strawberry tongue
Cervical lymphadenopathy
Red plams of the hands and the soles of the feet which alter peel

Kawasaki disease
Mx of kawasaki
High dose aspirin
IVIG
Echocardiogram as screening test for coronary artery aneurysm
Cx of kawasaki
Coronary artery aneurysm
An 8-year-old boy presents with increasing jaundice over the past week. He was recently treated with nitrofurantoin for a simple urinary tract infection. On examination he is obviously jaundiced, and he is looking pale and breathless. Investigation results are as follows:
Hb58 g/l
Platelets250 * 109/l
WBC6.5 * 109/l
A blood films demonstrates red cell fragments and Heinz bodies.
What is the most likely diagnosis?
Pyruvate kinase deficiency
Sickle cell disease
Glucose-6-phosphate dehydrogenase deficiency
Beta-thalassaemia
Hereditary spherocytosis
Glucose-6-phosphate dehydrogenase deficiency is an X linked disorder affecting red cell enzymes. It results in a reduced ability of the red cells to respond to oxidative stress. Therefore, red cells have a shorter life span and are more susceptible to haemolysis, particularly in response to drugs (e.g. nitrofurantoin), infection, acidosis and certain dietary agents (e.g. fava beans).
The red cell fragments, Heinz bodies and anaemia confirm a haemolytic anaemia.
Features of G6PD
Features
neonatal jaundice is often seen
intravascular haemolysis
gallstones are common
splenomegaly may be present
Heinz bodies on blood films
Dx of G6PD
Enzyme assay
Drugs thought to be safe in G6PD
Some drugs thought to be safe
penicillins
cephalosporins
macrolides
tetracyclines
trimethoprim
Inheritance of G6PD
X-linked recessive
Inheritance of HS
Male+female AD
Fraser guidelines
The following points should be fulfilled:
the young person understands the professional’s advice
the young person cannot be persuaded to inform their parents or allow the professional to contact them on their behalf
the young person is likely to begin, or continue having, sexual intercourse with or without contraceptive treatment
unless the young person receives contraceptive treatment, their physical or mental health, or both, is likely to suffer
the young person’s best interests require them to receive contraceptive advice or treatment with or without parental consent
A 6-year-old boy is reviewed in clinic due to nocturnal enuresis. His mother has tried using a star-chart but unfortunately this has not resulted in any significant improvement. Of the following options, what is the most appropriate initial management strategy?
Enuresis alarm
Trial of oral desmopressin
Trial of imipramine
Trial of intranasal desmopressin
Restrict fluids in the afternoon and evening
Restricting fluids is not recommended advice - Clinical Knowledge Summaries suggest: ‘Do not restrict fluids. The child should have about eight drinks a day, spaced out throughout the day, the last one about 1 hour before bed.’
Enuresis alarm
Def: enuresis
Involuntary discharge of urine by day or night or both in any child aged >5 in the absence of congenital or acquired defects of the nervous system of the urinary tact
Can be primary or secondary (dry for at least 5 months before)
Mx of Nocturnal enuresis
Look for possible underlying causes/triggers: constipation, DM, UTI
Advise on fluid intake
Reward systems e.g. star charts
Enuresis alarm for children <7
Desmopressin may be used if >7y particulalry if ST control is needed or an enuresis alarm has been ineffective
Mx of meningitis
ABCD approach
- Antibiotics
- Steroids if >1m and H influenzae, dexamehtasone
- Fluids e.g. colloid
- Cerebral monitoring
- PH notification and antibiotic prophlyaxis of contacts- rifampicin
Antibiotics in childhood meningitis
<3m: IV amoxicillin and IV cefotaxime
>3m: IV cefotaxime
Used for antibiotic prophylaxis of contacts to child with meningitis?
Rifampicin
For patients with meningococcal septicaemia, LP?
Is contraindicated, blood cultures and PCR for meningococcus should be obtained
Contraindications to LP
Signs of raised ICP
Focal neurology
Papilloedema
Bulging of the fontanelle
DIC
Signs of cerebral herniation
Henry is a 29 week premature baby who was born 2 weeks ago. Over the past week it has been noted that he has had bloody stool, abdominal distension and has not been feeding well. Physical examination reveals an increased abdominal girth with reduced bowel sounds. Abdominal X-ray shows dilated asymmetrical bowel loops and bowel wall oedema. What is the likely diagnosis?
Intussusception
Inflammatory bowel disease
Pyloric stenosis
Hirschsprung’s disease
Necrotising enterocolitis
The correct answer for this question is necrotising enterocolitis.
AXR findings in NEC
dilated bowel loops (often asymmetrical in distribution)
bowel wall oedema
pneumatosis intestinalis (intramural gas)
portal venous gas
pneumoperitoneum resulting from perforation
air both inside and outside of the bowel wall (Rigler sign)
air outlining the falciform ligament (football sign)
Features of NEC
Necrotising enterocolitis is one of the leading causes of death among premature infants. Initial symptoms can include feeding intolerance, abdominal distension and bloody stools, which can quickly progress to abdominal discolouration, perforation and peritonitis.
You see a worried mum with her 6 month old baby boy. She is concerned that his skull shape is not normal. His development and birth have been normal and there are no conditions in the family. On examination his head circumference is at the 40th centile with his height and weight at the 30th centile. His occiput is flattened on the left, his left ear mildly protruding forward and his left forehead more prominent than the right. No other abnormality is detected. What is the most appropriate management?
Urgent referral to neurosurgery
Suggest buying an infant helmet
Arrange an MRI scan
Routine referral to community child health clinic
Reassurance
Plagiocephaly is more common since there have been campaigns to encourage babies to sleep on their back to reduce the risk of sudden infant death syndrome (SIDS). Plagiocephaly is a skull deformity producing unilateral occipital flattening, which pushes the ipsilateral forehead ear forwards producing a ‘parrallelogram’ appearance. The vast majority improve by age 3-5 due to the adoption of a more upright posture. Helmets are not usually recommended as there was no significant difference between groups in a randomised controlled trial. Turning the cot around may help the child look the other way and take the pressure off the one side. Other simple methods include giving the baby time on their tummy during the day, supervised supported sitting during the day, and moving toys/ mobiles around in the cot to change the focus of attention. Ensure all advice is in line with prevention of SIDS.
Plagiocephaly
parallelogram shaped head
the incidence of plagiocephaly has increased over the past decade. This may be due to the success of the ‘Back to Sleep’ campaign
Craniosynostosis
premature fusion of skull bones
A 4-year-old boy was discharged from the hospital six weeks ago after an episode of viral gastroenteritis. He now has 4-5 loose stools each day which has been present for the past four weeks.
What is the most likely diagnosis?
Coeliac disease
Inflammatory bowel disease
Secondary bacterial infection
Lactose intolerance
Clostridium difficile infection
Transient lactose intolerance is a common complication of viral gastroenteritis. Removal of lactose from the diet for a few months followed by a gradual reintroduction usually resolves the problem.
Gastroenteritis
main risk is severe dehydration
most common cause is rotavirus - typically accompanied by fever and vomiting for the first 2 days. The diarrhoea may last up to a week
treatment is rehydration
Causes of chronic diarrhoea in infants
most common cause in the developed world is cows’ milk intolerance
toddler diarrhoea: stools vary in consistency, often contain undigested food
coeliac disease
post-gastroenteritis lactose intolerance
Which one of the following statements regarding cerebral palsy is incorrect?
It is the most common cause of major motor impairment in children
Less than 5% of children will have epilepsy
It affects 2 in 1,000 live births
20% of children have hearing impairment
Postnatal factors account for 10% of cases
Around 30% of children with cerebral palsy have epilepsy
Def: Cerebal palsy
Cerebral palsy may be defined as a disorder of movement and posture due to a non-progressive lesion of the motor pathways in the developing brain. It affects 2 in 1,000 live births and is the most common cause of major motor impairment
Possible manifestations of cerebal palsy
Abnormal tone in early infancy
Delayed motor milestones
Abnormal gait
Feeding difficulties
Non-motor problems associated with cerebal palsy
learning difficulties (60%)
epilepsy (30%)
squints (30%)
hearing impairment (20%)
Causes of cerebal palsy
antenatal (80%): e.g. cerebral malformation and congenital infection (rubella, toxoplasmosis, CMV)
intrapartum (10%): birth asphyxia/trauma
postnatal (10%): intraventricular haemorrhage, meningitis, head-trauma
Classification of cerebal palsy
Spastic (70%0: hemiplegia, diplegia or quadriplegia
Dyskinetic
Ataxic
Miced
Mx of cerebal palsy
MDT
Spasticity: oral diazepam, oral and intrathecal baclofen, botulinum toxin type A. orthopaedic surgery
Anticonvulsants, analgesia PRN
What is the most common cause of nappy rash
Irritant dermatitis
Irritant dermatitis
The most common cause, due to irritant effect of urinary ammonia and faeces
Creases are characteristically spared

Irritant dermatitis
Candida dermatitis
Typically an erythematous rash which involve the flexures and has characteristic satellite lesions

Typically an erythematous rash which involve the flexures and has characteristic satellite lesions
Seborrhoeic dermatitis
Erythematous rash with flakes. May be coexistent scalp rash
Mx Nappy rash
General management points
disposable nappies are preferable to towel nappies
expose napkin area to air when possible
apply barrier cream (e.g. Zinc and castor oil)
mild steroid cream (e.g. 1% hydrocortisone) in severe cases
A 1-year-old girl is investigated for recurrent urinary tract infections. A micturating cystourethrogram is ordered:
What does this image demonstrate?
Vesicoureteric reflux
Horseshoe kidney
Paediatric urolithiasis
Duplex collecting system
Isolated right-sided hydronephrosis

This image demonstrates grade V vesicoureteric reflux - gross dilatation of the ureter, pelvis and calyces with ureteral tortuosity. A DMSA scan is needed to identify renal scarring.
Def: VUR
Vesicoureteric reflux (VUR) is the abnormal backflow of urine from the bladder into the ureter and kidney. It is relatively common abnormality of the urinary tract in children and predisposes to urinary tract infection (UTI), being found in around 30% of children who present with a UTI. As around 35% of children develop renal scarring it is important to investigate for VUR in children following a UTI
Pathophysiology of VUR
Pathophysiology of VUR
ureters are displaced laterally, entering the bladder in a more perpendicular fashion than at an angle
therefore shortened intramural course of ureter
vesicoureteric junction cannot therefore function adequately
Grade I VUR
Into uretur only, no dilatation
Grade II VUR
Into renal pelvis on micturition, no dilatation
Grade III VUR
Mild/moderate dilatation of the uretur, renal pelvis and calyces
Grade IV VUR
Dilatation of the renal pelvis and calyces with moderate ureteral tortuosity
Grade V VUR
Gross dilatation of the uretur, pelvis and calyces with ureteral tortuosity
Ix in VUR
Normally following a micturating cystourethrogram
DMSA scan may be performed to look for renal scarring
Features of bronchiolitis
Bronchiolitis is a condition characterised by acute bronchiolar inflammation. Respiratory syncytial virus (RSV) is the pathogen in 75-80% of cases. SIGN released guidelines on bronchiolitis in 2006. Please see the link for more details.
Epidemiology
most common cause of a serious lower respiratory tract infection in < 1yr olds (90% are 1-9 months, with a peak incidence of 3-6 months). Maternal IgG provides protection to newborns against RSV
higher incidence in winter
coryzal symptoms (including mild fever) precede:
dry cough
increasing breathlessness
wheezing, fine inspiratory crackles (not always present)
feeding difficulties associated with increasing dyspnoea are often the reason for hospital admission
Bronchiolitis
Pathogens in bronchiolitis
respiratory syncytial virus (RSV) is the pathogen in 75-80% of cases
other causes: mycoplasma, adenoviruses
may be secondary bacterial infection
more serious if bronchopulmonary dysplasia (e.g. Premature), congenital heart disease or cystic fibrosis
Def: Surfactant lung disease
Surfactant deficient lung disease (SDLD, also known as respiratory distress syndrome and previously as hyaline membrane disease) is a condition seen in premature infants. It is caused by insufficient surfactant production and structural immaturity of the lungs
Risk of SDLD at 26-28w
50%
Risk of SDLD at 30-31w
25%
Other risk factors apart from gestation for SDLD
Male sex
Diabetic mothers
C sec
Second born of premature twins
Clinical features of SDLD
Tachypnoea
Intercostal recession
Expiratory grunting
Cyanosis
Mx of SDLD
Maternal corticosteroids
O2
Assisted ventilation
Exogenous surfactant given via endotracheal tube
A 15-year-old boy presents to his GP complaining of knee pain for one week. He has no significant past medical history. Which of the following would make a diagnosis of Osgood-Schlatter disease more likely?
Bilateral knee pain.
Sudden onset of symptoms and acutely painful.
Knee pain isolated to the posterior aspect of the knee joint.
Pain relieved by rest and made worse by kneeling and activity, such as running or jumping.
Locking of the knee on movement.
Osgood-Schlatter disease may be diagnosed on the basis of clinical features alone. This age group (adolescent) is the most likely age to suffer from this condition and is localized to the tibial tuberosity.
Typically, pain is:
Unilateral (but may be bilateral in up to 30% of people).
Gradual in onset and initially mild and intermittent, but may progress to become severe and continuous.
Relieved by rest and made worse by kneeling and activity, such as running or jumping.
Chondromalacia patellae
Softening of the cartilage of the patella
Common in teenage girls
Characteristically anterior knee pain on walking up and down stairs and rising from prolonged sitting
Usually responds to physiotherapy
Osgood-Schlatter disease
(tibial apophysitis)
Seen in sporty teenagers
Pain, tenderness and swelling over the tibial tubercle
Osteochondritis dissecans
Pain after exercise
Intermittent swelling and locking
Patellar subluxation
Medial knee pain due to lateral subluxation of the patella
Knee may give way
Patellar tendonitis
More common in athletic teenage boys
Chronic anterior knee pain that worsens after running
Tender below the patella on examination
When is Guthrie test performed?
5-9d of life
What conditions are included on Guthrie test?
Congenital hypothyroidism
CF
PKU
SCD
MCADD
Features of strawberry naevi
Strawberry naevi (capillary haemangioma) are usually not present at birth but may develop rapidly in the first month of life. They appear as erythematous, raised and multilobed tumours.
Typically they increase in size until around 6-9 months before regressing over the next few years (around 95% resolve before 10 years of age).
Common sites include the face, scalp and back. Rarely they may be present in the upper respiratory tract leading to potential airway obstruction
Capillary haemangiomas are present in around 10% of white infants. Female infants, premature infants and those of mothers who have undergone chorionic villous sampling are more likely to be affected
Cx of strawberrys naevi
Mechanical: e.g. obstructing visual fields or airway
Bleeding
Ulceration
Thrombocytopenia
Mx of strawberry naevi
Most spontaneously resolve
If treatment required can use propranolol
What is a cavernous haemangioma?
Deep capilalry haemangioma

Strwaberry naevus
Cavernous haemangioma
Cavernous hemangioma, also calledcavernous angioma, or cerebral cavernoma (when referring to presence in the brain)[1] is a type of blood vessel malformation or hemangioma, where a collection of dilated blood vessels form abenign tumor. Because of this malformation, blood flow through the cavities, or caverns, is slow. Additionally, the cells that form the vessels do not form the necessary junctionswith surrounding cells. Also, the structural support from the smooth muscle is hindered, causing leakage into the surrounding tissue. It is the leakage of blood, known as a hemorrhage from these vessels that causes a variety of symptoms known to be associated with this disease.
What are the innocent murmurs heard in children?
Ejection murmurs
Venous hum
Still’s murmur
Ejection murmur
Due to turbulent blood flow at the outflow tract of the heart
Venous hum
Heard as a continuous blowing noise just below the clavicles
Due to turbulent blood flow in the great veins
Still’s murmur
Low-pitched sound heard at the lower left sternal edge
Characteristics of an innocent murmur
Soft blowing murmur in the pulmonary area or short buzzing murmur in the aortic area
May vary with posture
No radiation
No diastolic component
No thrill
No added sounds e.g. clicks
Asymptomatic child
No other abnormality
A 2-year-old boy is brought to the surgery by his mother with earache and pyrexia. On examination of the precordium a murmur is heard. Which one of the following characteristics is not consistent with an innocent murmur?
Short buzzing murmur in the aortic area
Soft-blowing murmur in the pulmonary area
Varies with posture
Diastolic murmur
Continuous blowing noise heard just below the clavicles
Diastolic murmur
Draw neonatal resscitation

Draw basic PLS

Ratio of chest compression in neonate?
3:1
Ratio of chest compressions in paediatric
5 initial breaths then 15:1
Def: Perthes disease
Perthes disease is a degenerative condition affecting the hip joints of children, typically between the ages of 4-8 years. It is due to avascular necrosis of the femoral head
Perthes disease is 5 times more common in boys. Around 10% of cases are bilateral
Features of Perthes disease
Hip pain: develops progressively over a few weeks
Limp
Stiffness and reduced range of movement
XR: early changes include joint space widening. Decreased femoral head size/flattening
Cx of Perthes
Osteoarthritis
Premature fusion of the growth plates

Perthes disease
Bilateral avascular necrosis of the femoral heads
Draw the nephritic and the nephrotic syndromes

Which one of the following types of glomerulonephritis is most characteristically associated with streptococcal infection in children?
Focal segmental glomerulosclerosis
Diffuse proliferative glomerulonephritis
Membranous glomerulonephritis
Mesangiocapillary glomerulonephritis
Rapidly progressive glomerulonephritis
Diffuse proliferative glomerulonephritis
Rapidly progressive glomerulonephritis - aka crescentic glomerulonephritis
rapid onset, often presenting as acute kidney injury
causes include Goodpasture’s, ANCA positive vasculitis
IgA nephropathy - aka Berger’s disease, mesangioproliferative GN
typically young adult with haematuria following an URTI
Diffuse proliferative glomerulonephritis
classical post-streptococcal glomerulonephritis in child
presents as nephritic syndrome / acute kidney injury
most common form of renal disease in SLE
Membranoproliferative glomerulonephritis (mesangiocapillary)
type 1: cryoglobulinaemia, hepatitis C
type 2: partial lipodystrophy
Minimal change disease
typically a child with nephrotic syndrome (accounts for 80%)
causes: Hodgkin’s, NSAIDs
good response to steroids
Membranous glomerulonephritis
presentation: proteinuria / nephrotic syndrome / chronic kidney disease
cause: infections, rheumatoid drugs, malignancy
1/3 resolve, 1/3 respond to cytotoxics, 1/3 develop chronic kidney disease
Focal segmental glomerulosclerosis
may be idiopathic or secondary to HIV, heroin
presentation: proteinuria / nephrotic syndrome / chronic kidney disease
Features of absence seizures
Absence seizures (petit mal) are a form of generalised epilepsy that is mostly seen in children. The typical age of onset of 3-10 years old and girls are affected twice as commonly as boys
Features
absences last a few seconds and are associated with a quick recovery
seizures may be provoked by hyperventilation or stress
the child is usually unaware of the seizure
they may occur many times a day
EEG: bilateral, symmetrical 3Hz spike and wave pattern
Mx of absence seizures
sodium valproate and ethosuximide are first-line treatment
good prognosis - 90-95% become seizure free in adolescence
Live attenuated vaccines
BCG
measles, mumps, rubella (MMR)
influenza (intranasal)
oral rotavirus
oral polio
yellow fever
oral typhoid*
A mother brings her 3-year-old child in to receive the DTP booster. Which one of the following would make it inappropriate to give the vaccination today?
Being below the 2nd centile for weight
Family history of allergy to DTP
Recent onset of a seizure disorder currently being investigated
Planned general anaesthesia in 2 weeks time
Being born at 29 weeks gestation
DTP: vaccination should be deferred in children with an evolving or unstable neurological condition
General contraindications to immunisation
confirmed anaphylactic reaction to a previous dose of a vaccine containing the same antigens
confirmed anaphylactic reaction to another component contained in the relevant vaccine (e.g. egg protein)
Situations where vaccines should be delayed
febrile illness/intercurrent infection
Contraindications to live vaccines
pregnancy
immunosuppression
What are the most common causes of hearing problems in children?
Conductive
secretory otitis media
Down’s syndrome*
Sensorineural
hereditary - Usher syndrome, Pendred syndrome, Jervell-Lange-Nielson syndrome, Wardenburg syndrome
congenital infection e.g. rubella
acquired - meningitis, head injury
cerebral palsy
perinatal insult
16-year-old boy presents to the emergency room with a history of groin pain for the past three hours. He has associated nausea and has vomited three times. He reports that he recently had unprotected vaginal sex. On examination there is tenderness and swelling of the scrotum and left testicle, with absence of the cremaster reflex on the left side. Elevation of the affected testicle causes increased pain.
What is the most likely diagnosis?
Torsion of the hydatid of Morgagni
Strangulated inguinal hernia
Epididymitis
Testicular torsion
Hydrocoele
Testicular torsion occurs when the testis turns on the remnant of the processus vaginalis thereby restricting blood flow. It usually presents with acutely severe testicular pain often with associated nausea and vomiting. There may be swelling of the testis with overlying erythema. The cremaster reflex may also be absent on the affected side. Elevation of the testicle often results in worsening of the pain.
Although this patient recently had unprotected sex, the history is less suggestive of epididymitis. With epididymitis we would expect urinary symptoms. In addition, elevation of the testes often relieves the pain (Prehn’s sign positive).
Ddx in acute scrotal disorder
Torsion
Irreducible inguinal hernia
Epididymitis
What is a positive Prehn’s sign
Elevation of the testes relieving pain.
Seen in epididymitis
Infants and nappies
Should have at least 6 heavy wet nappies in 24h

Molluscum contagiosum
Typical presentation of molluscum contagiosum
Typically, molluscum contagiosum presents with characteristic pinkish or pearly white papules with a central umbilication, which are up to 5 mm in diameter. Lesions appear in clusters in areas anywhere on the body (except the palms of the hands and the soles of the feet). In children, lesions are commonly seen on the trunk and in flexures, but anogenital lesions may also occur. In adults, sexual contact may lead to lesions developing on the genitalia, pubis, thighs, and lower abdomen. Rarely, lesions can occur on the oral mucosa and on the eyelids.
At what age do the majority of children achieve day and night time urinary continence?
2-3 years old
3-4 years old
4-5 years old
5-6 years old
6-7 years old
The majority of children achieve day and night time continence by 3 or 4 years of age
A jittery and hypotonic baby may suggest
neonatal hypoglycaemia.
You are called to the post natal ward to review an 8 hour old baby born by elective caesarian section at 39 weeks gestation. After reading the case notes you discover the use of maternal labetalol for high blood pressure. On examination the baby appears jittery and hypotonic. What is the most appropriate next step?
Record temperature and ensure adequately wrapped
Perform full septic screen
Measure blood glucose levels
Start empirical antibiotics for early onset sepsis
Re-examine after next feed
A jittery and hypotonic baby may suggest neonatal hypoglycaemia. The use of maternal labetalol is a risk factor and these babies must have their blood glucose measured. Neonatal abstinence syndrome may also present in this way and so the use of maternal opiates or illicit drug use in pregnancy should also be ascertained.
Causes of neonatal hypoglycaemia
Maternal DM
Prematurity
IUGR
Hypothermia
Neonatal sepsis
Inborn errors of metbolism
Nesidioblastosis
Nesidioblastosis
Nesidioblastosis is a controversial medical term for hyperinsulinemic hypoglycemiaattributed to excessive function ofpancreatic beta cells with an abnormalmicroscopic appearance. The term was coined in the first half of the 20th century. The abnormal histologic aspects of the tissue included the presence of islet cell enlargement, islet cell dysplasia, beta cells budding from ductal epithelium, and islets in apposition to ducts.
Developmental milestones: speech and hearing
3 months
Quietens to parents voice
Turns towards sound
Squeals
Developmental milestones: speech and hearing
6m
Double syllables: adah, erleh
Developmental milestones: speech and hearing
9m
Mama, Dada
understands no
Developmental milestones: speech and hearing
12m
Responds to own name
Developmental milestones: speech and hearing
12-15m
Knows about 2-6 words
Refer at 18m
Understands simple commands
Developmental milestones: speech and hearing
2y
Combine 2 words
Points to parts of the body
Developmental milestones: speech and hearing
2.5t
Vocabulary of 200w
Developmental milestones: speech and hearing
3y
Talks in short sentences (3-5w)
Asks what and who questions
Identifies colours
Counts to 10
Developmental milestones: speech and hearing
4y
Asks why, when and how questions
What are the criteria for sending a child with an acute limp for urgen assesment?
<3
>8 with painful or restricted hip movements (in particular internal rotation) to exclude SUFE
Is unable to weight bear
Has fever and or red flags suggesting serious pathology: pain waking them at night, fatigue, anorexia, weight loss, night sweats
In severe pain, agitated or has reduced peripheral pulses or muscle weakness that may indicate neurovascular compromise or impending compartment syndrome
?Maltreatment
Transient synovitis
Acute onset
Usually accompanies viral infections, but the child is well or has a mild fever
More common in boys, aged 2-12 years
Septic arthritis/osteomyelitis
Unwell child, high fever
Juvenile idiopathic arthritis
Limp may be painless
Slipped upper femoral epiphysis
10-15 years - Displacement of the femoral head epiphysis postero-inferiorly
On routine antenatal swabs, a mother is found to be colonised with Group B Streptococcus. However, she did not receive adequate intrapartum antibiotic prophylaxis and she delivers a healthy baby girl by vaginal delivery. Her baby does not require any resuscitation and remains well in the post natal ward. The mother is eager for discharge home. What is the most appropriate course of action with regards to her child?
Intravenous antibiotics for 24 hours
Check C-Reactive protein levels and take blood cultures
Discharge if no suspicion of infection
Perform routine 6 hour post natal check and discharge with community midwife follow up.
Regular observations for 24 hours
Maternal colonisation with group B streptococcus is a minor risk factor for early onset sepsis in the newborn. Newborns with only one minor risk factor for early onset sepsis should remain in hospital for at least 24 hours with regular observations. Two or more minor risk factor or one red flag warrant empirical antibiotic therapy with Benzylpenicillin and Gentamicin and a full septic screen.
Red flags for GBS infection
Suspected or confirmed infection in another baby in the case of a multiple pregnancy
Parenteral antibiotic treatment given to the woman for confirmed or suspected invasive bacterial infection (such as septicaemia) at any time during labour, or in the 24-hour periods before and after the birth [This does not refer to intrapartum antibiotic prophylaxis]
Respiratory distress starting more than 4 hours after birth
Seizures
Need for mechanical ventilation in a term baby
Signs of shock
A 9-year-old girl is brought to surgery as her mother is concerned that she is too fat. This has now been a problem for over two years and mum feels this is holding her back at school. What is the most appropriate method to ascertain how obese she is?
Body mass index
Body mass index percentile adjusted to age and gender
Weight plotted on percentile chart
Mother’s perception
Waist circumference
Defining obesity is more difficult in children than adults as body mass index (BMI) varies with age. BMI percentile charts are therefore needed to make an accurate assessment. Recent NICE guidelines suggest to use ‘UK 1990 BMI charts to give age- and gender-specific information’
Assessment of obese child
NICE recommend
consider tailored clinical intervention if BMI at 91st centile or above.
consider assessing for comorbidities if BMI at 98th centile or above
Causes of obesity in children
Lifestyle
growth hormone deficiency
hypothyroidism
Down’s syndrome
Cushing’s syndrome
Prader-Willi syndrome
Consequences of obesity in children
Consequences of obesity in children
orthopaedic problems: slipped upper femoral epiphyses, Blount’s disease (a development abnormality of the tibia resulting in bowing of the legs), musculoskeletal pains
psychological consequences: poor self-esteem, bullying
sleep apnoea
benign intracranial hypertension
long-term consequences: increased incidence of type 2 diabetes mellitus, hypertension and ischaemic heart disease
Features of Acne vulgaris
Acne vulgaris is a common skin disorder which usually occurs in adolescence. It typically affects the face, neck and upper trunk and is characterised by the obstruction of the pilosebaceous follicle with keratin plugs which results in comedones, inflammation and pustules.
Epidemiology
affects around 80-90% of teenagers, 60% of whom seek medical advice
acne may also persist beyond adolescence, with 10-15% of females and 5% of males over 25 years old being affected
Pathophysiology of acne vulgaris
follicular epidermal hyperproliferation resulting in the formation of a keratin plug. This in turn causes obstruction of the pilosebaceous follicle. Activity of sebaceous glands may be controlled by androgen, although levels are often normal in patients with acne
colonisation by the anaerobic bacterium Propionibacterium acnes
inflammation
What are the referral points in developmental problems
Referral points
doesn’t smile at 10 weeks
cannot sit unsupported at 12 months
cannot walk at 18 months
Hand preference before 12m?
Is abnormal and may indicate cerebal palsy
Gross motor problems most common causes?
Variant of normal
CP
Neuromuscular disorders
Speech and language problems, causes
Check hearing
Environmental deprivation
General developmental delay
Def: febrile convulsions
Febrile convulsions are seizures provoked by fever in otherwise normal children. They typically occur between the ages of 6 months and 5 years and are seen in 3% of children
Clinical features of febrile convulsions
usually occur early in a viral infection as the temperature rises rapidly
seizures are usually brief, lasting less than 5 minutes
may be generalised tonic or tonic-clonic
Px following febrile convulsion
risk of further febrile convulsion = 1/3 (higher if family history)
if recurrences, try teaching mother how to use rectal diazepam
if no focal signs + lasts less than 30 minutes* + single seizure then 1% risk of developing epilepsy
in the <1% who have all these features, risk of developing epilepsy is much higher (e.g. 50%)
A newborn male baby is found to have an undescended right testicle during the routine 6-8 week examination. It is neither palpable in the scrotum or inguinal canal. What is the most appropriate management?
Outpatient referral to urology to be seen within 4 weeks
Review at 3 months
Immediate referral to urology
Arrange ultrasound abdomen and scrotum
Review at 12 months
Undescended testicle - wait 6 months prior to referral
If the testicle has not descended by around 3 months then referral should be considered for orchidopexy.
Features of undescended testis
Undescended testis occurs in around 2-4% of term male infants., but is much more common if the baby is preterm. Around 25% of cases are bilateral
Complications of undescended testis
infertility
torsion
testicular cancer
psychological
Management
orchidopexy: NICE CKS now recommend referral should be considered from around 3 months of age, with the baby ideally seeing a urological surgeon before 6 months of age. Surgical practices vary although the majority of procedures are performed at around 1 year of age
What are the organisms which may colonise a patient with CF?
Staphylococcus aureus
Pseudomonas aeruginosa
Burkholderia cepacia*
Aspergillus
Which one of the following best describes the emergency treatment of a child with severe croup?
Oxygen + nebulised saline
Oxygen + nebulised adrenaline
Oxygen + nebulised salbutamol
Oxygen + IM benzylpenicillin
Oxygen + nebulised steroids
Oxygen + nebulised adrenaline
Oral dexamethasone should also be given if the child is able to take it.
A 6-week-old term infant has difficulty feeding due to increased breathlessness. As the on-call doctor you are called to review this baby. You witness the baby feeding and note she is pink and well perfused but sweating profusely with and increased respiratory rate. On examination you hear a soft pan-systolic murmur at the lower left sternal border.
What is the most likely underlying pathology?
Transient tachypnoea of the newborn
Acute respiratory distress syndrome
Heart failure
Eisenmenger syndrome
Infantile pneumonia
Heart failure typically presents in infants with symptoms of breathlessness worse on exertion (e.g. feeding), sweating, poor feeding and recurrent chest infections.
On examination you should: examine the growth charts (?failure to thrive), examine for tachycardia, tachypnoea, murmurs and pre and post-ductal saturations.
Heart failure may be due to duct dependant systemic circulations (<2 weeks old) e.g. coarctation of the aorta or left-to-right shunts (>2 weeks old) e.g. VSD as the pulmonary vasculature resistance begins to fall.
In this case the baby has a large VSD causing decompensated heart failure. Cardiac lesions can be missed during the foetal anomaly scan and this baby would need a detailed foetal echocardiogram and discussion with the cardiac team on management strategies.
What are the acyanotic congenital heart defects?
Acyanotic - most common causes
ventricular septal defects (VSD) - most common, accounts for 30%
atrial septal defect (ASD)
patent ductus arteriosus (PDA)
coarctation of the aorta
aortic valve stenosis
VSDs are more common than ASDs. However, in adult patients ASDs are the more common new diagnosis as they generally presents later
What are the most common causes of cyanotic congenital heart disease?
Cyanotic - most common causes
tetralogy of Fallot
transposition of the great arteries (TGA)
tricuspid atresia
pulmonary valve stenosis
Fallot’s is more common than TGA. However, at birth TGA is the more common lesion as patients with Fallot’s generally presenting at around 1-2 months
Factors which point towards child abuse include:
story inconsistent with injuries
repeated attendances at A&E departments
late presentation
child with a frightened, withdrawn appearance - ‘frozen watchfulness’
Possible physical presentations of child abuse include:
bruising
fractures: particularly metaphyseal, posterior rib fractures or multiple fractures at different stages of healing
torn frenulum: e.g. from forcing a bottle into a child’s mouth
burns or scalds
failure to thrive
sexually transmitted infections e.g. Chlamydia, Gonorrhoea, Trichomonas

Henoch Schonlein Purpura
Features of HSP
Henoch-Schonlein purpura (HSP) is an IgA mediated small vessel vasculitis. There is a degree of overlap with IgA nephropathy (Berger’s disease). HSP is usually seen in children following an infection.
Features
palpable purpuric rash (with localized oedema) over buttocks and extensor surfaces of arms and legs
abdominal pain
polyarthritis
features of IgA nephropathy may occur e.g. haematuria, renal failure
Mx of HSP
Analgesia for arthralgia
Supportive treatment for nephropathy
Px of HSP
Self-limiting condition, especially in children without renal involvement
1/3rd have a relapse
An 18 month old child attends the paediatric assessment unit with his mother. He has been brought in as he has had a fever, barking cough and difficulty breathing at night. He has been diagnosed with croup and you have been asked to see him to review. After history and assessment you are confident there is no stridor or respiratory distress. What would your next step in management be?
Give antibiotics
Give oxygen
Full ENT exam
Give nebulised adrenaline
Give oral dexamethasone
This child has mild croup, the severity of croup is based upon; respiratory rate, respiratory distress, heart rate, O2 saturations and exhaustion. Treatment of mild croup is oral dexamethasone 0.15mg/kg single dose and review. Systemic dexamethasone and nebulised adrenaline 5ml of 1:1000 are used in severe croup, alongside oxygen administration. Antibiotics should not be given unless an underlying bacterial infection is suspected. You should not perform an ENT exam due to the possibility of an epiglottis diagnosis.
Features of foetal alcohol syndrome
Features
short palpebral fissure
thin vermillion border/hypoplastic upper lip
smooth/absent filtrum
learning difficulties
microcephaly
growth retardation
epicanthic folds
Baby may show symptoms of alcohol withdrawal at birth e.g. irritable, hypotonic, tremors
A mother notices that her newborn boy has small eye openings, a small body and low-set ears. On examination the paediatrician also notes a flat philtre, a sunken nasal bridge, short palpebral fissures and a thin upper lip. What is the most likely cause?
Diabetes
Maternal alcohol abuse
Group B Streptococcal infection
Maternal Listeria
Maternal opioid abuse
Fetal alcohol syndrome
Maternal alcohol abuse during pregnancy.
Presentation: IUGR, microcephaly, midfacial hypoplasia, micrognathia, smooth philtrum, microphthalmia, short palpebral fissures, thin upper lip, irritability, ADHD.
What is the most common cause of DS and risk of recurrence?
94% non-disjunction
What proportion of DS caused by Robertsonian translocation?
Risk of recuccrence
5% (usually onto chromosome 14)
10-15% if mother is translocation carrier
2.5% if father is translocation carrier
What are the chromosomal causes of DS
Non disjunction
Translocation
Mosaicism
A mother asks for information following a recent admission of her 2-year-old son with a febrile convulsion. What is the chance of her son having a further febrile convulsion?
Febrile convulsions - risk of further convulsions = 30%
An 11-year-old girl presents with a productive cough and fever. A chest x-ray is taken:
Bilateral pneumothoraces
Left lingula consolidation
Dilated cardiomyopathy with pulmonary oedema
Left humeral head fracture
Left middle lobe consolidation

The loss of the left heart border is a classic sign of left lingula consolidation. There is no left middle lobe!
A 10-year-old girl is admitted with shortness-of-breath and fatigue. A chest x-ray is performed on admission:
Based on the x-ray findings, what is the most likely diagnosis?
Inhaled foreign object
Heart failure
Asthma
Cystic fibrosis
Pneumonia

The x-ray shows dilated cardiomyopathy and features of pulmonary oedema including fluid in the horizontal fissure.
Causes of snoring in children
Obesity
Nasal problems: polyps, deviated septum, hypertrophic nasal turbinates
Recurrent tonsilitis
DS
Hypothyroidism
Disease not excluded from school
Conjunctivitis
Fifth disease
Roseola
Infectious mononucleosis
Head lice
Threadwormsq
Fifth disease
Erythema infectiosum or fifth disease is one of several possible manifestations of infection by parvovirus B19.[1] The disease is also referred to as slapped cheek syndrome, slapcheek, slap face orslapped face.[2][3]
The name “fifth disease” comes from its place on the standard list ofrash-causing childhood diseases, which also includes measles (1st),scarlet fever (2nd), rubella (3rd), and Dukes’ disease (4th), though the latter is no longer widely accepted as distinct.
Roseola infantum
Roseola is a disease of children, generally under two years old.[1]Although it has been known to occur in eighteen-year-olds, whose manifestations are usually limited to a transient rash (“exanthem”) that occurs following a fever of about three days’ duration.
It is caused by two human herpesviruses, human herpesvirus 6 (HHV-6) and human herpesvirus 7 (HHV-7), which are sometimes referred to collectively as Roseolovirus. There are two variants of HHV-6 (HHV-6a and HHV-6b) and studies in the US, Europe, Dubai and Japan have shown that exanthema subitum is caused by HHV-6b. This form of HHV-6 infects over 90% of infants by age 2. Research has shown that babies can be congenitally infected with HHV-6 via vertical transmission.[2] This has been shown to occur in 1% of children in the United States.[3][4]
Excluded from school for 24h after commencing antibiotics
Scarlet fever
School exclusion 4 d from onset of rash
Measles
School exclusion 5d from onset of rash
Chickenpox
School exclusion 5d from onset of swollen glands
Mumps
School exclusion until 5d after commencing antibiotics
Whooping cough
School exclusion 6d from onset of rash
Rubella
School exclusion until symptoms have settled over 48h
D+V
School exclusion until lesions have crusted over
Impetigo
School exclusion until treated
Scabies
School exclusion until recovered
IFV
USS screening for DDH
Breech presentation is a risk factor for developmental dysplasia of the hip (DDH), so you should check that the baby has been referred for screening for this condition. The Department of Health advises that all babies that were breech at any point from 36 weeks (even if not breech by time of delivery), babies born before 36 weeks who had breech presentation, and all babies with a first degree relative with a hip problem in early life, should be referred for ultrasound of the hips. If one of a pair of twins is breech, both should be screened. Some Trusts also refer babies with other conditions including oligohydramnios, high birthweight, torticollis, congenital talipes calcaneovalgus and metatarsus adductus. Further details on screening for DDH can be found at the link below.
For which one of the following indications is carbamazepine least likely to be a useful management option?
Trigeminal neuralgia
Absence seizures
Bipolar disorder
Temporal lobe epilepsy
Complex partial seizures
Carbamazepine is generally ineffective in absence seizures
Features of carbamazepine
Carbamazepine is chemically similar to the tricyclic antidepressant drugs. It is most commonly used in the treatment of epilepsy, particularly partial seizures, where carbamazepine remains a first-line medication. Other uses include
neuropathic pain (e.g. trigeminal neuralgia, diabetic neuropathy)
bipolar disorder
Mechanism of action
binds to sodium channels increases their refractory period
Adverse effects of carbamazepine
Adverse effects
P450 enzyme inducer
dizziness and ataxia
drowsiness
headache
visual disturbances (especially diplopia)
Steven-Johnson syndrome
leucopenia and agranulocytosis
syndrome of inappropriate ADH secretion
First sign of male puberty
Testicular growth at 10-15y/o
Testicular volume >4ml= onset of puberty
Maximum height spurt at 14
Normal changes during puberty
Gynaecomastia in boys
Asymmetrical breast growth in girls
Diffuse enlargement of the thyroid gland may be seen
A 2 day old baby who was born by a ventouse delivery is noted to have a swelling on the left side of his head in the parietal region. His head appeared normal immediately after delivery. On examination, the baby is well and the swelling does not cross suture lines. The fontanelles and sutures appear normal. What is the most likely diagnosis?
Subaponeurotic haematoma
Caput succedeneum
Craniosynostosis
Skull fracture
Cephalohaematoma
A cephalohaematoma appears as a swelling due to bleeding between the periosteum and the skull. It is most commonly noted in the parietal region and is associated with instrumental deliveries. The swelling usually appears 2-3 days following delivery and does not cross suture lines. It gradually resolves over a number of weeks.
Draw difference between caput succedaneum and cepahlohaematoma


Caput succedaneum
Cephalohaematoma



A 9-year-old boy who has recently arrived from India presents with fever. On examination a grey coating is seen surrounding the tonsils and there is extensive cervical lymphadenopathy. What is the most likely diagnosis?
Dengue fever
Typhoid
Paratyphoid
Actinomycosis
Diphtheria
Diphtheria
Features of diptheria
Diphtheria is caused by the Gram positive bacterium Corynebacterium diphtheriae
Pathophysiology
releases an exotoxin encoded by a β-prophage
exotoxin inhibits protein synthesis by catalyzing ADP-ribosylation of elongation factor EF-2
Diphtheria toxin commonly causes a ‘diphtheric membrane’ on tonsils caused by necrotic mucosal cells. Systemic distribution may produce necrosis of myocardial, neural and renal tissue
Presentation of diptheria
Recent visitor to Eastern Europe/Russia/Asia
Sore throat with a diptheric membrane
Bulky cervical lymphadenoapthy
Neuritis e.g. cranial nerves
Heart block

Dipthertitic membrane
A baby born at 35 weeks gestations via normal vaginal delivery is found to be irritable 48 hours after birth and suffers a convulsion. There is no obvious head trauma or swellings. Which one of the following cranial injuries is most likely to have occurred?
Caput succedaneum
Cephalohaematoma
Subaponeurotic haemorrhage
Intraventricular haemorrhage
Extradural haemorrhage
Caput succedaneum is caused by pressure on the fetal scalp during the birthing process. It results in a large oedematous swelling and bruising over the scalp. Treatment is not required as the swelling reduces over a few days.
A cephalohaematoma may occur after a spontaneous vaginal delivery or following a trauma from the obstetric forceps or the ventouse. A haemorrhage results after the presidium is sheared from the parietal bone. The tense swelling is limited to the outline of the bone. It reduces over a few weeks - months.
A Subaponeurotic haemorrhage, also known as a subgaleal haemorrhage is rare and is due to a traumatic birth. It may result in the infant losing large amounts of blood.
An intracranial haemorrhage refers to subarachnoid, subdural or intraventricular haemorrhages. Subarachnoid haemorrhages are common and may cause irritability and even convulsions over the first 2 days of life. Subdural can following the use of forceps. Intraventricular haemorrhage mostly affects pre-term infants and can be diagnosed by ultrasound examinations.
Extradural haemorrhage is unlikely to occur during the birthing process.
Features of intraventricular haemorrhage
Haemorrhage into the ventricles
Occurs in premature neonates, may occur spontaneously
Blood may clot and occlue CSF flow, hydrocephalus may result.
Vast majority occurs in frist 72h after birth
Treatment of intraventricular haemorrhage
Supportive
Most treatments have been trialled and shown not to be of benefit
Hydrocephalus and rising ICP is an indication for shunting
You are an FY1 on the paediatric ward round with your consultant. Whilst seeing a child that has been admitted with croup, the consultant you’re with decides to quiz you on the pathophysiology.
‘What is the most likely organism to cause croup?’
Respiratory syncytial virus (RSV)
Parainfluenza virus
Pseudomonas aeruginosa
Streptococcus pneumoniae
Bordetella pertussis
Parainfluenza
A 2-year-old boy presents with a harsh cough and pyrexia. His symptoms worsened overnight and on examination stridor is noted. Which one of the following interventions may improve his symptoms?
Codeine linctus
Humidified oxygen
Nebulised salbutamol
Oral erythromycin
Oral dexamethasone
Oral dexamethasone
A 5-year-old girl attends your GP surgery with her mother. She reports a five day history of a sore throat and fever. On examination you note a bright red tongue, flushed face and a rough dry erythematous rash on her neck.
What is the most likely diagnosis?
Measles
Rubella
Bordetella pertussis
Kawasaki disease
Scarlet fever
A strawberry tongue can be seen in both scarlet fever and Kawasaki disease. However given the history a diagnosis of scarlet fever is more likely.
Lay rescuers vs two or more trained rescuers in PLS
30:2 vs 15:2 chest compressions to breaths
Presenting features of CF
Neonatal period (20%): meconium ileus, prolonged jaundice
Recurrent chest infections (40%)
Malabsroption (30%): steatorrhoea, FTT
Other featuers: liver disease
Short stature
DM
Delayed puberty
Rectal prolapse (due to bulky stools)
Nasal polyps
Male infertility, female subfertility
Developmental milestones: fine motor and vision
3m
Reaches for object
Holds rattle briefly if given to hand
Visually alert, particularly to human faces
Fixes and follows to 180 deg
Developmental milestones: fine motor and vision
6m
Holds in palmar grasps
Passes objects between hands
Visually insatiable: looking around in every direction
Developmental milestones: fine motor and vision
9m
Points with finger
Early pincer
Developmental milestones: fine motor and vision
12m
Good pincer grip
Bangs toys together
Developmental milestones: fine motor and vision Bricks
15m
Tower of 2
Developmental milestones: fine motor and vision Bricks
18m
Tower of 3
Developmental milestones: fine motor and vision Bricks
2y
Tower of 6
Developmental milestones: fine motor and vision Bricks
3y
Tower of 9
Developmental milestones: fine motor and vision drawing
18m
Circular scribble
Developmental milestones: fine motor and vision drawing
2y
Copies vertical line
Developmental milestones: fine motor and vision drawing
3y
Copies circle
Developmental milestones: fine motor and vision drawing
4y
Copies cross
Developmental milestones: fine motor and vision drawing
5y
Copies square and triangle
Developmental milestones: fine motor and vision book
15m
Looks at book, pats page
Developmental milestones: fine motor and vision book
18m
Turns pages several at a time
Developmental milestones: fine motor and vision book
2y
Turns pages, one at a time
Mx of chickenpox
Keep cool, trim nails
Calamine lotion
School exclusion
Immunocompromised patients and newborns with peripartum exposure should receive VZIG. If chickenpox develops, IV aciclovir should be considered
Cxs of chickenpox
Commonly: secondary bacterial infection of the lesioins
Rarer:
pneumonia
encephalitis (cerebellar involvement)
disseminated haemorrhagic chcikenpox
arthritis, nephritis, pancreatitis

Chest x-ray showing miliary opacities secondary to healed varicella pneumonia. Multiple tiny calcific miliary opacities noted throughout both lungs. These are of uniform size and dense suggesting calcification. There is no focal lung parenchymal mass or cavitating lesion seen.The appearances are characteristic for healed varicella pneumonia.
Features of VZV
Chickenpox is caused by primary infection with varicella zoster virus. Shingles is reactivation of dormant virus in dorsal root ganglion
Chickenpox is highly infectious
spread via the respiratory route
can be caught from someone with shingles
infectivity = 4 days before rash, until 5 days after the rash first appeared*
incubation period = 10-21 days
Clinical features (tend to be more severe in older children/adults)
fever initially
itchy, rash starting on head/trunk before spreading. Initially macular then papular then vesicular
systemic upset is usually mild
Contraindications to MMR
severe immunosuppression
allergy to neomycin
children who have received another live vaccine by injection within 4 weeks
pregnancy should be avoided for at least 1 month following vaccination
immunoglobulin therapy within the past 3 months (there may be no immune response to the measles vaccine if antibodies are present)
Adverse effects of MMR
malaise, fever and rash may occur after the first dose of MMR. This typically occurs after 5-10 days and lasts around 2-3 days
An 8-year-old boy presents with weakness and purple striae on his abdomen. On examination he is obese with a central fat distribution and is found to have facial plethora. He is also found to have a blood pressure of 130/85 mmHg and facial plethora.
What is the most likely underlying cause?
ACTH-secreting pituitary tumour
Adrenal carcinoma
Craniopharyngioma
Congenital adrenal hyperplasia
Ectopic adrenocorticotropin-producing tumour
The history is suggestive of Cushing’s syndrome. In an 8-year old boy the commonest cause of Cushing’s would be iatrogenic use of glucocorticoids. Out of the options above the most likely answer is an ACTH-secreting pituitary tumour.
Eczema herpeticum
Eczema herpeticum describes a severe primary infection of the skin by herpes simplex virus 1 or 2. It is more commonly seen in children with atopic eczema. As it is potentially life threatening children should be admitted for IV aciclovir
A 2-year-old child with a history of atopic eczema is brought to the local GP surgery. Her eczema is usually well controlled with emollients but her parents are concerned as the facial eczema has got significantly worse overnight. She now has painful clustered blisters on both cheeks, around her mouth on her neck. Her temperature is 37.9ºC. What is the most appropriate management?
Advise paracetamol + emollients and reassure
Admit to hospital
Add hydrocortisone 1%
Oral flucloxacillin
Topical fusidic acid
Eczema herpeticum is a serious condition that requires IV antivirals
IM benzylpenicillin for suspected meningococcal septicaemia in the community dose
<1y
300mg
IM benzylpenicillin for suspected meningococcal septicaemia in the community dose
1-10y
600
IM benzylpenicillin for suspected meningococcal septicaemia in the community dose
>10y
1200mg
Def: precocious puberty
‘development of secondary sexual characteristics before 8 years in females and 9 years in males’
more common in females
How can precocious puberty be classified?
Gonadotrophin dependant (central/true)
Gonadotrophin independant
Central precocious puberty
Due to premature access of the HPgonadal axis
FSH and LH raised
Pseudo precocious puberty
Due to excess sex hormones
FSH and LH low
Precocious puberty in males?
Uncommon, usually has an organic cause
Bilateral testes enlargement in male with precocious puberty
Gonadotrophin release from intracranial lesion
Unilateral enlargement of testes in precocious puberty
Gonadal tumour
Small testes in precocious puberty
Adrenal cause (tumour or adrenal hyperplasia)
Precocious puberty in females
Usually idiopathic or familial and follows normal sequence of puberty
Organic causes are rare
associated with rapid onset, neurological symptoms and signs and dissonance
e.g. McCune Albright syndrome
A mother brings her 9-year-old daughter into surgery. She has been having recurrent headaches. Which one of the following features of migraine is more common in children?
Prolonged migraines (e.g. 24-48 hours)
Strictly unilateral symptoms
Hemiplegia
Good response to metoclopramide
Gastrointestinal disturbance
Nausea, vomiting and abdominal pain are common in children with migraine.
Please rate this question:
Migraines in children
Tend to be shorter-lasting
Headache commonly bilateral
GI disturbance more prominent
Aura symptoms
motor weakness
double vision
visual symptoms affecting only one eye
poor balance
decreased level of consciousness.
Minimal change disease
75% of cases of nephrotic syndrome in children
Causes of nephrotic syndrome
Majority are idiopathic
Cause found in 10-20%
Drugs: NSAIDS, rifampicin
HL, thymoma
Infectious mononucleosis
Pathophysiology of minimal change disease
T cell and cytokine mediated damage to the GBM-> polyanion loss.
Resultant reduciton of electrostatic charge _> increased glomerular permeability to serum albumin
Featrues of minimal change disease
Nephrotic syndrome
Normotension (HTN rare)
Highly selective proteinuria: only intermediate-sized proteins such as albumin and transferrin leak through the glomerulus
Renal biopsy: electron micrsoscpy shows podocyte fusion
Mx of minimal change disease
80% are steroids responsive
Cyclophosphamide is the next step
Px of minimal change disease
1/3rd have one episode
1/3rd have infrequent relapses
1/3rd have frequent relapses
Prader Willi syndrome pathophysiology
Prader-Willi syndrome is an example of genetic imprinting where the phenotype depends on whether the deletion occurs on a gene inherited from the mother or father:
Prader-Willi syndrome if gene deleted from father
Angelman syndrome if gene deleted from mother
Prader-Willi syndrome is associated with the absence of the active Prader-Willi gene on the long arm of chromosome 15. This may be due to:
microdeletion of paternal 15q11-13 (70% of cases)
maternal uniparental disomy of chromosome 15
Features of PWS
Hypotonia during infancy
Dysmorphic features
Short features
Hypogonadism and infertility
LD
Childhood obesity
Behavioural problems in adolescence
You are in a genetics clinic and explaining to a mother and father the reasoning why their son has Prader-Willi syndrome. What is the term we use to describe the mode of inheritance for Prader-Willi syndrome?
Autosomal recessive
Autosomal dominant
Imprinting
Pleiotropy
Variable expressivity
Prader-Willi is an example of imprinting. For this disease to occur, the patient does not receive the gene from their father. The mother’s gene may be normal, but that does not prevent the phenotype occurring. The phenotype consists of learning difficulties, hypotonia, obesity and the urge to eat.
Autosomal recessive is when a person receive a defect gene from the mother and a defective gene from the father causing them to have the particular condition. An example of this is cystic fibrosis.
Autosomal dominant refers to when a person only need to receive one defective gene to inherit a condition, this can be from the mother or father. An example of this would Huntington’s disease.
Pleiotropy refers to when one gene, when defective, causing two or more clinical effects that appear unrelated.
Variable expressibility refers to when an inherited genetic defect causes different levels of clinical effect.
A baby is born at term via vaginal delivery with no complications, however he is still not showing signs of breathing at one minute. Heart rate is >100bpm, but he is floppy and cyanosed. What is the most appropriate next step in management?
Call for anaesthetist to intubate the baby
5 mouth-to-mouth rescue breaths
5 breaths of oxygen via face mask
Start chest compressions
Suction airways
Airway suction should not be performed unless there is obviously thick meconium causing obstruction, as it can cause reflex bradycardia in babies. Chest compressions are not indicated, as the HR in this case is >100bpm. CPR should only be commenced at a HR < 60bpm. In cases where there are no signs of breathing and this is thought to be due to fluid in the lungs, five breaths should be given via a 250ml bag via face mask. This is a more effective and more hygienic method than using mouth-to-mouth in a hospital setting.
A 14-year-old male being investigated for iron-deficiency anaemia is found to have numerous polyps in his jejunum. On examination he is also noted to have pigmented lesions on his palms and soles. What is the likely diagnosis?
Hereditary non-polyposis colorectal carcinoma
Gardner’s syndrome
Familial adenomatous polyposis
Peutz-Jeghers syndrome
Hereditary haemorrhagic telangiectasia
Hereditary haemorrhagic telangiectasia is associated with mucocutaneous lesions and iron-deficiency anaemia but intestinal polyps are not a feature
Features of Peutz-Jeghers syndrome
Peutz-Jeghers syndrome is an autosomal dominant condition characterised by numerous hamartomatous polyps in the gastrointestinal tract. It is also associated with pigmented freckles on the lips, face, palms and soles. Around 50% of patients will have died from a gastrointestinal tract cancer by the age of 60 years.
Genetics
autosomal dominant
responsible gene encodes serine threonine kinase LKB1 or STK11
Features
hamartomatous polyps in GI tract (mainly small bowel)
pigmented lesions on lips, oral mucosa, face, palms and soles
intestinal obstruction e.g. intussusception
gastrointestinal bleeding
Management
conservative unless complications develop

Peutz-Jeghers syndrome
You see a 6 week-old baby boy for his routine baby check and note a small, soft, umbilical hernia on examination. What should you do?
Advise parents to tape a coin over the area
Refer for surgery
Refer for ultrasound
Watch and wait
Arrange emergency admission
Small umbilical hernias are common in babies and tend to resolve by 12 months of age. Parents should be reassured no treatment is usually required but to be aware of the signs of obstruction or strangulation such as vomiting, pain and being unable to push the hernia in - this is rare in infants. Advise the parents to present the child at around 2 years of age if the hernia is still present to arrange referral to a surgeon. Attempts to treat the hernia by strapping or taping things over the area are not helpful and can irritate the skin.


The mother of a 6-week-old baby girl born at 32 weeks gestation asks for advice about immunisation. What should happen regarding the first set of vaccines?
Give first set of vaccinations at 3 months (i.e. delay for 1 month)
Give DTaP/IPV/Hib at 2 months but not PCV
Give first set of vaccinations at 4 months (i.e. correct for gestational age)
Give first set of vaccinations as per normal timetable but within hospital environment
Give as per normal timetable
Give as per normal timetable
You are asked to by the Primary Care Trust to design a program to improve the health of infants in the local community. What is the most common cause of death of infants greater than one month but less than one year old?
Accidents
Congenital disorders
Sudden infant death syndrome
Cancer
Infection
Sudden infant death syndrome
After the age of 1 year accidents are the most common cause of death in children
A 12-year-old female from Bulgaria presents to the surgery. She reports being unwell for the past 2 weeks. Initially she had a sore throat but she is now experiencing joint pains intermittently in her knees, hips and ankles. On examination there are some pink, ring shaped lesions on the trunk and occasional jerking movements of the face and hands. What is the most likely diagnosis?
Lyme disease
Infective endocarditis
Polyarticular juvenile idiopathic arthritis
Rheumatic fever
Still’s disease
Rheumatic fever
Features of rheumatic fever
Rheumatic fever develops following an immunological reaction to recent (2-6 weeks ago) Streptococcus pyogenes infection. Diagnosis is based on evidence of recent streptococcal infection accompanied by:
2 major criteria
1 major with 2 minor criteria

Erythema marginatum
Rheumatic fever criteria
JONES
CAFE PAL
Major
Joint involvement
O- myocarditis
Nodules, subcutaenous
Erythema marginatum
Sydenham’s chorea
Minor
CRP increased
Arthralgia
Fever
Elevated ESR
Proloned PRI
Anamnesis of rheumatism
Leukocytosis
Evidence of recent strep infection
ASOT >200iU/mL
Hx of scarlet fever
Positive throat swab
Increase in DNAse B titre
You are reviewing a 9-month-old child with suspected bronchiolitis. Which one of the following features should make you consider other possible diagnoses?
Fine inspiratory crackles
Rhinitis
Feeding difficulties
Temperature of 39.7ºC
Expiratory wheeze
A low-grade fever is typical in bronchiolitis. SIGN guidelines advise that the presence of high fever should make the clinician carefully consider other causes before making the diagnosis.
After birth which of the following happens in the foetus?
The foramen ovale opens allowing blood to circulate into the pulmonary artery
Haemoglobin A is replaced by Haemoglobin F, which has a lower affinity for oxygen and may lead to physiological jaundice in the newborn
The umbilical veins and arteries remain open for several days
The ductus arteriosus closes
The first few breaths force lung fluid into the fetal alveoli
After birth, the foramen ovale, ductus arteriosus and umbilical vessels close within a few hours.
After a few days Haemoglobin F is replaced by Haemoglobin A, which has a lower affinity for oxygen and may lead to physiological jaundice in the newborn, due to the breakdown of fetal blood cells. The first few breaths force lung fluid out of the fetal alveoli.
Foraemn ovale
This allows blood to shunt from the right atrium to left atrium, without having to pass through the lungs. At birth the lungs become functional and the pulmonary pressure decreases, resulting in a left atrial pressure which exceeds the right atrial pressure. This forces the septum primum septum secundum together, functionally closing the foramen ovale. The septa eventually fuse, leaving a remnant of the foramen ovale, called the fossa ovalis.
Ductus arteriosus:
This is a vessel connecting the pulmonary artery to the aorta which allows blood from the right ventricle to bypass the non-functioning fetal lungs. After birth this closes to form the ligamentum arteriosum. The closure of the ductus arteriosus allowed blood to circulate into the pulmonary artery and become oxygenated. If the ductus arteriosus fails to close patients are left with a patent ductus arteriosus (PDA) which causes left-to-right shunting and can lead to pulmonary hypertension, heart failure and arrhythmias.
Truncus arteriosus
Ascending aorta and pulmonary trunk
The division of the truncus arteriosus is triggered by neural crest cell migration from the pharyngeal arches. Problems with the migration may lead to transposition of the great arteries or tetralogy of Fallot
Bulbis cordis
Right ventricle and smooth parts of left ventricle
Primitive atria
Trabeculated parts of the left and right atria
Primitive ventricle
Majority of left ventricle
Left horn of the sinus venous
Coronary sinus
Right horn of the sinus venous
Smooth part of the right atrium
Right common cardinal vein and right anterior cardinal vein
Superior vena cava
Umbilical artery
Medial umbilical ligaments
Umbilical vein
Ligamentum teres hepatis (inside falciform ligament)
Ductus arteriosus
Ligamentum arteriosum
Ductus venous
Ligamentum venosum
Urachus
The urachus is a fibrous remnant of the allantois, a canal that drains the urinary bladder of the fetus that joins and runs within the umbilical cord.[1] The fibrous remnant lies in the space of Retzius, between the transversalis fascia anteriorly and the peritoneum posteriorly.
Pre-school wheeze in children
Wheeze is extremely common in pre-school children, with an estimated 25% of children having an episode of wheeze before 18 months. Viral-induced wheeze is now one of the most common diagnoses made on paediatric wards. There is however ongoing debate regarding the classification of wheeze in this age group and the most appropriate management.
Over recent years, led by the European Respiratory Society Task Force, the favoured classification for pre-school wheeze is to divide children into one of two groups;
episodic viral wheeze: only wheezes when has a viral upper respiratory tract infection (URTI) and is symptom free inbetween episodes
multiple trigger wheeze: as well as viral URTIs, other factors appear to trigger the wheeze such as exercise, allergens and cigarette smoke
Episodic viral wheeze is not associated with an increased risk of asthma in later life although a proportion of children with multiple trigger wheeze will develop asthma.
Mx of episodic viral wheeze
Episodic viral wheeze
treatment is symptomatic only
first-line is treatment with short acting beta 2 agonists (e.g. salbutamol) or anticholinergic via a spacer
next step is intermittent leukotriene receptor antagonist (montelukast), intermittent inhaled corticosteroids, or both
there is now thought to be little role for oral prednisolone in children who do not require hospital treatment
Mx Multiple trigger wheeze
trial of either inhaled corticosteroids or a leukotriene receptor antagonist (montelukast), typically for 4-8 weeks
An 18-month-old boy is brought to the GP by his mother as she is concerned about his breathing. Three days ago he started with fever, cough and rhinorrhoea. For the past 24 hours his mother reports that he has been ‘wheezy’. On examination his temperature is 37.9ºC, heart rate 126/min, respiratory rate 42/min and a bilateral expiratory wheeze is noted. You prescribe a salbutamol inhaler along with a spacer. Two days later the mother represents noting the inhaler has made little difference to the wheeze. Clinical findings are similar, although his temperature today is 37.4ºC. What is the most appropriate next step in management?
Inhaled long-acting beta agonist
Oral prednisolone
Add in regular ipratropium bromide
Oral montelukast or inhaled corticosteroid
Oral amoxicillin
This child is likely to have a viral-induced wheeze, also known as episodic viral wheeze. First-line treatment is short-acting bronchodilator therapy. If this is not successful then either oral montelukast or inhaled corticosteroids should be tried.
What is the prevalence of atopic eczema in children?
1-2%
2-5%
15-20%
11-12%
5-10%
Eczema occurs in around 15-20% of children and is becoming more common. It typically presents before 6 months but clears in around 50% of children by 5 years of age and in 75% of children by 10 years of age
Featues of eczma
in infants the face and trunk are often affected
in younger children eczema often occurs on the extensor surfaces
in older children a more typical distribution is seen, with flexor surfaces affected and the creases of the face and neck
Mx of eczma
Avoid irritants
Simple emollients: prescribe large amounts in a ratio with topcial steroids of 10:1. If a topical steroid is being used the emollient should be applied first followed by waiting at least 30 minutes before applying topical steroids.
Topical steroids
In severe cases wet wraps and oral ciclosporin may be used
Characteristic features of congenital rubella infection
Sensorineural deafness
Congenital cataracts
Congenital heart disease: PDA
Glaucoma
Other features include:
Growth retardation
Hepatosplenomegaly
Purpuric skin lesions
Salt and pepper chorioretinitis
Micropthalmia
CP
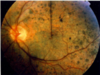
Salt and pepper chorioretinitis
Rubella
TORCH
Toxoplasmosis
Other: syphillis, VZV, parvovirus B19
Rubella
CMV
Herpes
Characteristic features of toxoplasmosis vertical transmission
Cerebral calcification
Chorioretinitis
Hydrocephalus
Other features:
Anaemia
Hepatosplenomegaly
CP
Characteristic of vertical CMV infection
Growth retardation
Purpuric skin lesions
Others:
Sensorineural deafness
Encephalitis/seizures
Pneumonitis
Hepatosplenomegaly
Anaemia
Jaundice
CP
TOF
VSD
RVH
Right ventricular outflow tract obstruction
Overriding aorta
What is the most common cause of cyanotic congenital heart disease?
TOF
*however, at birth transposition of the great arteries is the more common lesion as patients with TOF generally present at around 1-2 months


What determines the clinical severity of TOF?
The severity of the RV outflow tract obstruction
Features of TOF
Cyanosis
Causes a right to left shunt
Ejection systolic murmur due to PS
Right sided aortic arch seen in 25%
CXR shows boot shaped heart, ECG shows RVH

Boot shaped heart
TOF
Mx of TOF
Surgical repair often undertaken in two parts.
Cyanotic episodes may be helped by beta blockers to reduce infundibular spasm
What is the most common cause of hypertension in children?
Renal vascular disease
Congenital adrenal hyperplasia
Renal parenchymal disease
Coarctation of the aorta
Phaeochromocytoma
Renal parenchymal disease
Causes of HTN in children
Renal parenchymal disease
Renal vascular disease
Coarctation of the aorta
Phaeo
CAH
Essential or primary HTN
It is December and you are the paediatric foundation doctor. A five month old baby is admitted through the paediatric observation unit with tachypnoea, tachycardia and fever. On examination there is evidence of increased work of breathing with sub costal and diaphragmatic recession. There is widespread wheeze. You discuss the patient with your senior and a diagnosis of bronchiolitis is established. Oxygen is started but it is not deemed appropriate to begin intravenous fluids at this time. Which investigation is important to conduct in the management of this patient?
Glucose
Full blood count
Nasopharyngeal aspirate
Urea and electrolytes
Arterial blood gas
Nasopharyngeal aspirate are recommended during the winter months to ascertain which children are suffering with respiratory syncitial virus positive bronchiolitis. By diagnosing these patients it helps with ward management of patients, placing RSV negative patients on a ward and RSV positive patients in a side room.
Urea and electrolytes would only be appropriate if the patient was on IV fluids.
Features of benign rolandic epilepsy
Form of childhood epilepsy which typically occurs between 4 and 12 years
Seizures characteristically occur at night
Typicall partial: paraesthesia affecting face but secondary generalisation amy occur.
Child is otherwise normal
EEG characteristically shows centro-temporal spikse
Px is excellent with seizures stopping by adolescence
Charlie is a 7 month old baby boy who presents to you with poor weight gain (50th to 10th centile), on examination he has an erythematous, blanching rash over his abdomen, colicky abdominal pain and vomiting after feeds. He has been breast feeding with top ups of ‘Aptamil’ formula. What is the most likely diagnosis?
Pyloric stenosis
Eczema
Infantile colic
Cows’ milk protein intolerance
Reflux
The correct answer is cows’ milk protein intolerance.
The following clues in the history would suggest the diagnosis of cows’ milk protein intolerance:
Multi-system involvement
7 months would suggest the new introduction of top up feeds which correlates with the symptoms
Faltering growth along with the multi-system involvement would suggest cows’ milk protein intolerance
Charlie is older than the classical age of presentation for pyloric stenosis (2 to 8 weeks very rare above 6 months)
The presentation is unusual for eczema, infantile colic and reflux due to the multi-system involvement in the history making cows’ milk protein intolerance more likely.
A newborn is found to have a number of congenital abnormalities including an extra finger on each hand, a cleft palate and lip, microphthalmia and microcephaly.
Which of the following chromosomes is most likely to be affected in this child?
9
12
13
18
21
Patau syndrome is a chromosomal abnormality resulting in an extra full copy of chromosome 13 (trisomy 13). Like many of the chromosomal defects, physical and mental disability is common, in this case key distinguishing features to separate Patau’s from other trisomy disorders include polydactyly, cleft lips and palates, microcephaly and microphthalmia. Many children die before within a year of birth but those who survive will often go on to show intellectual and motor disability.
What are the most common #s associated with child abuse?
Radial
Humeral
Femoral
What are the common #s not associated with NAI
Distal radial
Elbow
Clavicular
Tibial
Triad in shaken baby syndrome
Retinal haemorrhages
Subdural haematoma
Encephalopathy
Caused by the intentional shaking of a child.
A 14-year-old boy is brought in by his mother who noticed her child had repeated episodes of slurred speech and gait abnormalities. On musculoskeletal examination, you notice muscle weakness, dysdiadochokinesis and spinal scoliosis. What is the mode of inheritance of this condition?
X-linked recessive
Autosomal dominant
Point mutation
X-linked dominant
Autosomal recessive
Firedrich’s ataxia
AR
Triad in HUS
Acute renal failure
MAHA
Thrombocytopenia
Causes of HUS
Post-dysentry- classically E Coli 0157:H7
Tumours
Pregnancy
Ciclosporin, OCP
SLE
HIV
Ix in HUS
FBC: anaemia, thrombocytopenia, fragmented blood film
U&E: acute renal failure
Stool culture
Mx of HUS
Supportive: fluids, blood transfusions, dialysis if required
No role for Abx.
PLEX reserved for cases not associated with diarrhoea
A 6-year-old boy is diagnosed as having nephrotic syndrome. A presumptive diagnosis of minimal change glomerulonephritis is made. What is the most appropriate treatment?
Cyclophosphamide
Albumin infusion
Plasma exchange
Renal biopsy followed by prednisolone
Prednisolone
A renal biopsy is only indicated if response to steroids is poor
A 29-week-old baby is born premature and shortly after birth experiences tachypnoea and tachycardia along with chest wall retractions. The paediatrician notes that the neonate has a blue discolouration of the skin and commences continuous positive airway pressure (CPAP) and intravenous fluids before explaining to the parents that the lungs lack surfactant, a compound that helps people breathe.
Which of the following cells are responsible for surfactant production?
Microfold cells
Alveolar macrophage
Type 1 pneumocytes
Type 2 pneumocytes
Paneth cells
Type 1 pneuomcytes are involved in the process of gas exchange between the alveoli and the blood and type 2 pneumocytes produce pulmonary surfactant.
Features of TTN
Transient tachypnoea of the newborn (TTN) is the commonest cause of respiratory distress in the newborn period. It is caused by delayed resorption of fluid in the lungs
It is more common following Caesarean sections, possibly due to the lung fluid not being ‘squeezed out’ during the passage through the birth canal
Chest x-ray may show hyperinflation of the lungs and fluid in the horizontal fissure
Supplementary oxygen may be required to maintain oxygen saturations. Transient tachypnoea of the newborn usually settles within 1-2 days
What is the most appropriate way to confirm a diagnosis of pertussis?
Blood cultures
Sputum culture
Per nasal swab
Urine for serology
Throat swab
Per nasal swab- may take weeks to come back
Causes of microcephaly
Normal variation e.g. small child
Familial e.g. parent with small head
Congenital infection
Perinatal brain injury e.g. hypxoci ischaemic encephalopathy
Fetal alcohol syndrome
Patau and other chromsomonal syndromes
Craniosynostosis
How can squints be classified?
By to where the eye deviates
The nose: esotropria
Temporally: exotropia
Superiorly: hypertropia
Inferiorly: hypotropia
A mother brings her son in to surgery as she suspects he has a squint. She thinks his right eye is ‘turned inwards’. You perform a cover test to gather further information. Which one of the following findings would be consistent with a right esotropia?
On covering the left eye the right eye moves medially to take up fixation
The cover test could not be used to identify this type of defect
On covering the left eye the right eye moves laterally to take up fixation
On covering the right eye the left eye moves laterally to take up fixation
On covering the right eye the left eye moves medially to take up fixation
On covering the left eye in this example the right eye moves laterally from the nasal (esotropic) position to take up fixation.
A neonate who was born prematurely at 35 weeks gestation is registered at the Practice. He was very well after delivery, without any notable complications such as respiratory problems. How should his routine childhood immunisations be given?
Adjust schedule for gestational age
Give according to chronological age
Refer to the hospital to receive first immunisations
Start immunisations at 3 months old
Delay until weight reaches 3.5kg
Babies who were born prematurely should receive their routine vaccinations according to chronological age; there should be no correcting for gestational age. Babies who were born prior to 28 weeks gestation should receive their first set of immunisations at hospital due to risk of apnoea.
A 14-year-old attends surgery. She was diagnosed with having migraines three years ago and requests advice about options for treating an acute attack. Which one of the following medications is it least suitable to recommend?
Aspirin
Paracetamol + prochlorperazine
Paracetamol + codeine
Ibuprofen
Paracetamol
Avoid aspirin in children < 16 years as risk of Reye’s syndrome
Aspirin should be avoided in children due to the risk of Reye’s syndrome.
Codeine would also be a poor choice as it has limited benefit in migraine.
Mx of migraine: acute treatment
First line: combination therapy with an oral triptan and an NSAID or an oral triptan and paracetamol
(for young people aged 12-17 consider a nasal triptan)
If the above measures are not effective or not tolearted offer a non-oral preparation of metoclopramide (NB risk of acute dystonic reactions in young children) or prochlorperazine and consider adding a non-oral NSAID or triptan
Mx of migraine: prophylaxis
Should be given if patients are expereincing 2 or more attacks per month
NICE adivses either topiramate or propranolol according to persons preference.
Propranolol should be used in women of child bearing age as topiramate may be teratogenic.
If these measures fail, NICE recommends a course of up to 10 sessions of acupuncture or gabapentin.
Ribloflavin may be affected
For women with premenstrual migrain, frovatriptan or zolmitriptan can be used as a mini-prophylaxis
Rules re 5-HT in mx of migraine
Agonists used in acute treatments
Antagonists used in prophylaxis
You are reviewing a 11-month-old baby with a viral upper respiratory tract infection. She is clinically well but at the end of the consultation her mother asks you about her development. You notice that she points and babbles ‘mama’ and ‘dada’ but has no other words. She is shy and cries when you try to examine her. There is an early pincer grip and she can roll from front to back but she cannot yet sit without support. How would you describe her development?
Normal development
Global developmental delay
Isolated delay in gross motor skills
Delay in speech + social skills, possibly early autism
Isolated delay in fine motor skills
Most babies can sit without support at 7-8 months so this probably represents a delay in gross motor skills. If still present at 12 months she should be considered for referral to a paediatrician. The other development features are normal for her age.
Rotavirus vaccination features
it is an oral, live attenuated vaccine
2 doses are required, the first at 2 months, the second at 3 months
the first dose should not be given after 14 weeks + 6 days and the second dose cannot be given after 23 weeks + 6 days due to a theoretical risk of intussusception
Other points
the vaccine is around 85-90% effective and is predicted to decrease hospitalisation by 70%
offers long-term protection against rotavirus
Meera brings her 5 year old daughter Reena to the surgery who is being treated for acute lymphoblastic leukaemia (ALL) for review as Reena’s classmate has been sent home from school with chickenpox. Reena is asymptomatic currently. Meera is unclear if Reena has suffered with chicken pox previously. What would be the correct management?
Admit urgently
Send home and come back if symptomatic
Prescribe aciclovir
Prescribe varicella zoster immunoglobulin
Urgent bloods for varicella zoster antibodies
‘People who have had a significant exposure to chickenpox and who are immunocompromised should be tested for varicella-zoster antibody, regardless of their history of chickenpox. Test for varicella-zoster immunoglobulin G (IgG) antibodies in primary care if test results can be available within 2 working days of first exposure. If this is not possible, urgently seek specialist advice because testing in secondary care and/or varicella-zoster immunoglobulin prophylaxis may be needed.’
A newborn baby has their blood glucose measured on the post natal ward as part of the neonatal hypoglycaemia protocol due to low birthweight. It measures 2.9mmol/L. The midwife asks you what you want to do next?
Admit to the Special Care Baby Unit (SCBU) for NG feeding
Offer additional feed if willing
Administer 100 mls intravenous 20% glucose
Measure blood glucose again in three hours time
Take blood sample for a formal glucose measurement
Neonatal hypoglycaemia is a common medical problem affecting neonates. This usually represents adaption to extrauterine life as opposed to any significant underlying medical problems. In the neonate blood glucose levels of >2.5mmol/L are usually regarded as normal. Formal measurements may be needed to confirm readings of either extreme as they are more reliable. If measurements are consistently >2.5mmol/L then monitoring can be stopped.
Which one of the following statements regarding absence seizures is incorrect?
Typical age of onset of 3-10 years old
Sodium valproate and ethosuximide are first-line treatments
Seizures may be provoked by a child holding their breath
There is a good prognosis
The EEG characteristically shows a bilateral, symmetrical 3Hz spike and wave pattern
Seizures are characteristically provoked by hyperventilation
Features of fetal varicella sndrome
Rsik of FVS following amternal varicella exposure is 1% IF OCCURS BEFORE 20W.
Skin scarring
Eye defects: microphthalmia
Limb hypoplasia
Microcephaly
LD
Pregnant woman with VZV rash
oral aciclovir should be given if pregnant women with chickenpox present within 24 hours of onset of the rash
1/2 alpha chains absent in alpha thalassaemia?
If 1 or 2 alpha chains are absent then the blood picture would be hypochromic and microcytic, but the Hb level would be typically normal
Loss of 3 alpha chains in alpha thalassaemia?
Hypocrhomic, microcytic anaemia with splenomegaly.
= HbH disease
Loss of 4 alpha chains in alpha thalassaemia?
Death in utero: hydrops fetalis, Bart’s hydrops
Causes of visual problems in children
congenital: infection, cataracts
prematurity - retinopathy of prematurity
cerebral palsy
optic atrophy e.g. hydrocephalus, optic nerve hypoplasia
albinism
The UK has recently switched to the new growth charts based on the WHO growth standard for children under the age of 5 years. The new UK-WHO charts have a separate preterm section and a 0-1 year section.
Key points
Key points
based on data from breast fed infants and all ethnic groups
the data matches UK children well for height and length but after 6 months UK children and slightly more heavy and more likely to be above the 98% centile
preterm infants born at 32-36 weeks have a separate chart until 2 weeks post-term
What is the pathophysiology of Fragile X?
Trinucleotide repeat disorder
Features of fragile x
In males:
LD
Large low set ears, long thin face, high arched palate
Macroorchidism
Hypotonia
Autism
Mitral valve prolapse
Features in females: range from normal to mild
A 4-year-old boy is admitted after developing a haemarthrosis in his right knee whilst playing in the garden. The following blood results are obtained:
Platelets220 * 109/l
PT12 secs
APTT78 secs
Factor VIIIc
activityNormal
What is the most likely diagnosis?
Antithrombin III deficiency
Von Willebrand’s disease
Antiphospholipid syndrome
Haemophilia A
Haemophilia B
A grossly elevated APTT may be caused by heparin therapy, haemophilia or antiphospholipid syndrome. A normal factor VIIIc activity points to a diagnosis of haemophilia B (lack of factor IX). Antiphospholipid syndrome is a prothrombotic condition
6-week-old infant is referred from the health visitor due to failure to thrive. The infant has fallen from the 50th to 9th centile on growth chart for weight. On further questioning, the parents reveal the infant vomits following each meal, which have on occasions ‘hit the wall.’ The mother’s pregnancy was unremarkable, with normal antenatal scans, and the infant was born by an uncomplicated vaginal delivery. There were no abnormal features noted at the newborn baby examination. What is the most likely diagnosis?
Intussusception
Infantile colic
Cow’s milk protein intolerance
Galactosaemia
Pyloric stenosis
In this question the most likely diagnosis is pyloric stenosis. Pyloric stenosis typically presents around 2-6 weeks of age. Infants tend to have projectile vomiting following feeds and remain hungry after vomiting. There may be an olive shaped mass in the right upper quadrant due to hypertrophy of the pylorus, and ‘waves of peristalsis’ may be seen following a test feed.
Which one of the following statements regarding infantile spasms is incorrect?
EEG shows hypsarrhythmia in the majority of children
Carries a good prognosis
More common in male children
Typically presents in the first 4 to 8 months
Causes characteristic ‘salaam’ attacks
Carries a good prognosis
West Syndrome
Infantile spasms
Features of infantile spasms
Type of childhood epilepsy which typically presents in the first 4-8m of life and is more common in males.
Often assocaited with serious underlying condition and the prognosis is poor.
Characteristics salaam attacks: flexion of the head, trunk and arms followed by extension of the arms.
This lasts 1-2 second but may be repeated up to 50 times
Progressive mental handicap
Ix in West Syndrome
EEG demonstrates hypsarrhythmia in 2/3rds of infants
CT demonstrates diffuse or localised brain disease in 70% e.g. tuberous sclerosis

Hypsarrhythmia
West Syndrome
Mx of West Syndrome
Poor Px
Vigabatrin is now considered first-line therapy
ACTH is also used
Features of Bartter’s syndrome
Bartter’s syndrome is an inherited cause (usually autosomal recessive) of severe hypokalaemia due to defective chloride absorption at the Na+ K+ 2Cl- cotransporter in the ascending loop of Henle. It should be noted that it is associated with normotension (unlike other endocrine causes of hypokalaemia such as Conn’s, Cushing’s and Liddle’s syndrome which are associated with hypertension)
Features
usually presents in childhood, e.g. Failure to thrive
polyuria, polydipsia
hypokalaemia
normotension
weakness
What are the primitive reflexes?
Moro
Grasp
Rooting
Stepping
Moro reflex
Head extension causes abduction followd by adduction of the arms
Present from birth to 3-4m old
Grasp reflex
Flexion of fingers when object placed in palm
Present from birth to around 4-5 months of age
Rooting reflex
Assists in breastfeeding
Present from birth to 4m of age
Stepping reflex
AKA walking reflex
Present from birth to around 2 onths of age
What are the 4 main Sickle cell crises?
Thrombotic ‘painful’ crises
Sequestration
Aplastic
Haemolytic
What are the features of thrombotic crises in SCD
AKA painful crises or vaso-occlusive crises
Precipitated by infection, dehydration, deoxygenation
Infarcts occur in various organs including the bones e.g. AVN of the hip, hand-foot syndrome (dactylitis) in children, lungs, spleen and brain
Sequestration crises in SCD
Sickling within the organs such as the spleen or lungs causes pooling of blood with worsening of the anaemia
Acute chest syndrome: dyspnoea, chest pain, pulmonary infiltrates, low pO2
The most common cause of death after childhood
In the context of an African patient suffering from a long-standing anaemia

Acute chest syndrome
Multiple pulmonary infiltrates
Aplastic crises in SCD
Caused by infection with parvovirus
Sudden fall in Hb
Hamolytic crises in SCD
Rare
Fall in Hb due to an increased rate of haemolysis
A 60 year-old man with haemophilia A has just become a grandfather. He wants to know what the chances are of his daughter’s son having haemophilia. Her daughter’s partner is well with no past medical history.
What is the probability that his daughter’s son has haemophilia A?
Impossible to calculate
50%
25%
No increased risk
100%
Haemophilia A is an X-linked recessive disease. This means that all female offspring of affected men will be carriers. There is then a 50% chance of these females passing the gene on. If the female’s children are male, they will therefore have a 50% chance of having the condition.
A man brings his 18 month old daughter to your GP clinic. She has had coryzal symptoms for the last 2 days. Last night, she started with a barking cough and a mild temperature of 37.8º.
On examination, there is a mild stridor when mobilising, with no recessions visible. Chest sounds clear with good air entry bilaterally. Temperature today remains at 37.8º, but all other observations are normal. What is the appropriate management?
Admit to hospital
Give nebulised adrenaline
Give a stat dose of dexamethasone 150 micrograms/kg PO
Give a salbutamol inhaler
Start antibiotics
This is a child who has croup. This is an illness that usually starts with coryzal symptoms, and the child then develops a seal like, barking cough.
The first stage is to work out how serious a case of croup this child has. Generally recommendations include:
Mild croup:
Occasional barking cough with no stridor at rest
No or mild recessions
Well looking child
Moderate croup:
Frequent barking cough and stridor at rest
Recessions at rest
No distress
Severe croup:
Prominent inspiratory stridor at rest
Marked recessions
Distress, agitation or lethargy
Tachycardia
In this case, the child would have mild croup.
Admission to hospital is only considered for moderate or severe croup, or if an alternative severe diagnosis like epiglottitis is suspected. It would not be appropriate in this case.
Nebulised adrenaline would only be used for children who were distressed, or who had a severe stridor. It would be not be used in this case as this child is well at rest with only a mild stridor on movement.
A salbutamol inhaler would only help if the child had wheeze, which she does not in this case. It would not give her any benefit.
Antibiotics are not indicated in croup as it is a viral illness.
Systematic reviews have shown that steroids can ease symptoms within a few hours. They also lead to fewer reattendances and fewer hospital admissions. Mild croup will resolve on its own, but Dexamethasone has been shown to be of some benefit.
Mx of CF
Regular (>BD) chest PT and psotural drainage. Deep breathing exercises are also useful
High calorie diet including high fat intake
Vitamin supplementation
Pancreatic enzyme supplements taken with meals
Heart and lung transplant
What is the most common cause of hypothyroidism in children in the UK?
Autoimmune thyroiditis
Other causes include:
Post total-body irradiation (i.e. in a child previously treated for ALL)
Iodine deficiency (most common cause in the developing world)
A 15-year-old collapses and dies whilst playing football and school. He had no past medical history of note. Post-mortem examination reveals asymmetric hypertrophy of the interventricular septum. Given the likely diagnosis, what is the chance his sister will also have the same underlying disorder?
0%
25%
50%
100%
66%
The underlying diagnosis is hypertrophic obstructive cardiomyopathy which is an autosomal dominant disorder. His sister therefore has a 50% chance of being affected.
Def: HOCM
AD disorder of muscle tissue caused by defects in te genes endocing contractile proteins.
Most common defects involves a mutation in the gene encoding beta-myosin heavy chain protein or myosin binding protein C
Features of HOCM
Often asymptomatic
Dyspnoea, angina, syncope
Sudden death (most commonly due to ventricular arrythmias), arrythmias, HF
Jerky pulse, large a waves, double apex beat
ESM
Jerky pulse, large a waves, double apex beat
HOCM
Conditions associated with HOCM
Friedreich’s ataxia
WPW
Echo findings in HOCM
MR SAM ASH
Mital regurgitation
Systolic anterior motion (SAM) of te anterior mitral valve leaflet)
Asymmetric hypertrophy (ASH)
ECG findings in HOCM
LV hypertrophy
Progressive T wave inversion
Deep Q waves
AF may be seen occasionally
Fever + Symptoms and signs: of meningococcal disease
Non-blanching rash, paritculalry in conjunction with:
an ill looking child
Lesions larger than 2mm (=purpura)
CRT >3s
Neck stiffness
Fever + Symptoms and signs: of meningitis
Neck stiffness
Bulging fontanelle
Decreased level of conciousness
Convulsive status epilepticus
Fever + Symptoms and signs: Herpes simplex encephalitis
Focal neurological signs
Focal seizures
Altered levels of consciousness
Fever + Symptoms and signs: pneumonia
Tachypnoea
Crackles in the chest
Nasal flaring
Chest indrawing
Cyanosis
SaO2 <95%
Fever + Symptoms and signs: UTI
Vomiting
Poor feeding
Lethargy
Irritability
Abdominal pain or tenderness
Urinary frequency or dysuria
Offensive urine/haematuria
Fever + Symptoms and signs: septic arthritis/osteomyelitis
Swelling of limb or joint
Not using an extremity
Not weight bearing
Fever + Symptoms and signs: Kawasaki
Fever lasting >5d and at least 4 from:
bilaterla conjuncitval injection
change in URT mucous membranes
Change in the peripheral extremitis
Polymorphous rash
Cervical lymphadenopathy
What are the most common causes of pharyngitis?
Adenovirus, enterovirus, rhinovirus
In older children Group A beta haemolytic strep
Def: tonsilitis
Form of pharyngitis where there is intensive inflammation of the tonsils, often with a purulent exudate
Common pathogens causing tonsilits?
Group A beta haemolytic strep
EBV
What differentiates between EBV and GAS tonsilitis
EBV surface exudate is more membranous, group a strep commonly gives a constitutional disturbance and has a white tonsilar exudate

EBV tonsiltiis

Group A strep tonsilitis
Mx of tonsilitis
Do not examine if ?acute epiglottitis
Assess airway and ability to feed
Abx commonly given, often penicllin or erythromycin if pen allergic
Analgesic with ibuprofen
NB: avoid amoxicillin as maculopapular rash may develop secondary to EBV.
This is to eradicate organism: 10d of antibiotics
Admit if unable to swallow solids/liquids.
Centor score components
<14 or >45 = +1
Exudate or swelling on tonsils
Tender/swollen anterior cervical lymph nodes
Fever >38
Cough absent
2 or 3: throat culture and treat with antibiotic
4-5 points: treat empirically with an antibioitc -risk of strep infection 56%
Indications for tonsillectomy
Useful in children with recurrent tonsilitis
Recurrent severe tonsilltiis
A peritonsillar abscess
Obstructive sleep apnoea

Quinsy abscess
Indications for adenoidectomy
Grow faster than airway between 2-8y of age
Can cause narrowing of the airway lumen
Recurrent otitis media with effusion and hearing loss
Obstructive sleep apnoea (absolute indication)
Symptoms of HSV
Asymptomatic
Gingiovstomatitis: most common manifestation of the virus in children, painful vesciles on the muth, hard palate, lips and tongue
Herpetic eczema
Herpetic whitlows: oedmatous white pusttules on the site of broken skin on the fingers
Eye infection
Meningitis/encephalitis
Penumonia and disseminated infeciton in the immunocompromised
Cx of EBV
Swelling of the pharynx so that is causes airway obstruction and difficulties feeding
Symptoms of EBV infection
Fever
Malaise
Tonsilopharyngitis limiting oral intake
Cervical lymphadenoathpy
Hepatosplenomegaly
Maculopapular rash
Jaundice
Petechiae on the soft palate
Ix in EBV
Atypical lymphocytes
Monospot test
Abs vs EBV
Mx of EBV
Supportive
Steroids if airway is compromsed
5% grow strep so treat with penicllin (not ampicillin or amoxicillin as these will cause florid maculopapular rash)
Erythema infantiosum
Fever
Malaise
Myalgia
Slapped cheek
Complications: arthrtis, arthralgia, aplastic anaemia
Causes fetal hydrops in utero
Caused by parvovirus B19

Erythema infectiosum (slapped cheek)
Coxsackie virus causes?
Hand, foot and mouth disease
Features of hand foot and mouth
Painful vesciular lesions on the hands, feet, mouth and tongue and often on the buttocks
Mild systemic features
Subsides within a few days with fluids and analgesia
Bornholms Disease
Bornholm disease or epidemic pleurodynia or epidemic myalgia[1] is a disease caused by the Coxsackie B virus or other viruses.[2]
Pleuritic chest pain, fever, myalgia- resolves within a few days
Draw the clinical features of chickenpox

What is the typical rash in chickenpox?
200-500 lesions start on head and trunk progressing to peripheries.
Appear as crops of papules, vesicles with surrounding erythema and pustules at different times
Itching and scratching may cause scarring.
If new lesions appear beyond 10d suggestive of defective cellular immunity
What are the cx of chickenpox
Bacterial superinfection:
Staph, strep
May lead to toxic shock syndrome or necrotising fasciitis
CNS:
Cerebellitis
Generalised encephalitis
Aseptic meningitis
Immunocompromised:
Haemorrhagic lesions
Pneumonitis
Progressive and disseminated infection
DIC
Rash in measles
Starts behind the ears, spreads downwards to the whole of the body
Discrete maculopapular rash intitially whch becomes blotchy and confluent
May desquamate
Draw the clinical course of measles

What are the symptoms of mumps
Fever
Malaise
Parotitis: pain on chewing or swalling
Transient unilateral heaing loss
Cx of mumps
Meningitis/encephalitis
Orchitis
Pancreatitis
Symptoms of rubella
Low grade fever
Maculopapular rash (non itch unlike adults)
Post auricular lymphadenopathy
Mx of Lyme disease
>12y: doxy
<12: amoxicillin
Neuro or cardio: IV ceftraixone
Treatment of impetigo
Topical abx e.g. mupirocin
More severe infections: fluclox or co-amoxiclav (as children prefer the taste)
Nasal carriage can be eradicated with a nasal cream containing mupirocin or chlorhexidine and neomycin
Aetiology of peri-orbital cellulitis?
Infants:
Staph or strep
Hib in unvaccinatied or trauma
Older: dental abscess or paranasal sinus infection
Symptoms of peri-orbital cellulitis
Tenderness, oedema of the eyelid, erythema and fever
Cx of periorbital cellulitis
Orbital cellulitis: if left untreated, can get pain on ocular movementm, proptosis, decreased visual actuity
Can progress to abscess formation, meningitis and cavernous sinus thrombosis
Ix in peri-orbital cellultis?
CT to exclude posterior spread
LP to exclude menignits
Mx of peri-orbital cellulitis
IV Abx to prevent posterior spread

Peri-orbital cellultitis
SCALDED SKIN SYNDROME
Infection and separation of the epidermal to granular layers due to an exfoliative staph toxin. Rare.
fever and malaise
a purulent, crusting, localised infection around the eyes, nose and mouth with subsequent widespread
erythema and tenderness of the skin.
Areas of epidermis separate on gentle pressure (Nikolsky sign), leaving denuded areas of skin which subsequently dry and heal without scarring.
Mx of scalded skin syndrome
IV Abx
Analgesia
Fluid maintenance

Scalded skin syndrome
Necrotising fascititis
Severe skin infection extending from the dermis_> fascia-> muscle
Caused by Staph or Group A strep +/- anaerobic bacteria
Systemically unwell
Severe pain
Necrotic centre with damaged tissue
Mx of necrotising fascititis
IV Abx
Surgical debridement
Possible ICU admission

Necrotising fasciitis
Pathophysiology of bacterial meningitis
Infection of the meninges usually follow bacteraemia
Inflammation and endothelial damage à cerebral oedema
à raised ICP à decreased blood flow à CEREBRAL CORTICAL INFARCTION
Fibrin deposits block CSF resorption by the arachnoid villi
à hydrocephalus
Meningitis in the Neonate-3m
GBS
E Coli and other coliforms
lIsteria
Meningitis in 1m-6y
N meningitidies
Strep penumoniae
HiB
Meningitis >6y
Neisseria meningitidis
Strep penumoniae
Cx of meningitis
Hearing loss
Local vasculitis
Local cerebral infarctaion
Subdural effusion
Hydrocephalus
Cerebral abscess
Signs of raised ICP in child
Reduce conscious level
Abnormal papillary response
Abnormal posturing
Kernig’s sign
With the child lying supine and with hips and kness flexed, there is back pain on extension of the knee
Cushing’s triad
Bradycardia
HTN
Abnormal pattern of breathing
= Raised ICP
Ix in meningitis
FBC and differential count
Blood glucose and blood gas
CRP and coag screen
U&Es
LFTs
MCS blood, throat swab, urine, stool
RAAT for meningitis organisms (blood, CSF, urine)
LP (CSF)
Mx of meningitis
Abx: third generation cephalosporin: cefotaxime or ceftriaxone
Dexamethasoone if beyond neonatal period to minimise risk of LT Cxs
Supportive
Prophylaxis with rifampicin
What are the contraindications to LP
Cardiorespiratory instability
Focal neurological signs
Signs of raised ICP
Coagulopathy
Thrombocytopenia
Local infection at site of LP
If it causes undue delay in starting antibiotics
Brudzinski sign
Flexion of the neck with the child supine causes flexion of the knees and hips
Aetiology of encephalitis
Direct invasion of the cerebrum by a neurotoxic virus (e.g. HSV)
Delayed brain swelling following a disordered neuroimmunological response to an antigen, usually a virus (post-infectious encephalopathy) e.g. following chickenpox
A slow virus infection, e.g. HIV or subacute sclerosing panencephalitis (SSPE) following measles
Enteroviruses, respiratory viruses and herpes virus (UK)
Mycoplasma, Borrelia burgdoferi, Bartonella henselae, rickettsial infections and the arboviruses (worldwide)
Ix in encephalitis
EEG and CT/MRI
PCR of CSF