OS 214 Renal Pathology Pictures Flashcards
(193 cards)
Identify the pointed structure (from Rosai & Ackerman)

Foot processes (epithelial aspect of BM). Electron micrograph of normal glomerulus. EN (endothelial cell); EP (epithelial cell); ME (mesangium).
Identify (from Rosai & Ackerman).

Minimal change disease (minimal abnormality in LM). Glomerulus normocellular, BM normal thickness. Most common cause of nephrotic syndrome in children. Characterized by diffuse effacement of foot processes in EM.
Identify (from Rosai & Ackerman).

Minimal Change Disease in EM. Note effacement of foot processes.
Identify (from trans)

FSGS under LM. With segmental sclerosis (pointed), and obliteration of glomerular capillaries.
Identify (from trans).

FSGS under LM with hyalinosis (pointed).
Identify (from Rosai & Ackerman)

FSGS under IF. (+) segmental deposition of IgM.
To differentiate from MCD:
Under LM, FSGS is already present. MCD looks normal.
Under IF: MCD is usually negative for Igs and C3.
Identify (from trans).

Membranous glomerulopathy (LM). Note normal to diffuse thickening of capillary wall. (+) foam cells in interstitium.
Identify (from Rosai & Ackerman)

MGN. Silver preparation showing “spike” formation along thickened BM.
Identify (be specific) (from Rosai & Ackerman).

MGN Stage I (EM). BM normal thickness. (+) subendothelial deposits (arrows). Epithelial foot processes obliterated.
Identify (be specific) (from Rosai & Ackerman).

MGN Stage II. Subepithelial deposits at regular interval, separated by projections of BM.
Identify (be specific) (from Rosai & Ackerman).

MGN Stage III. BM markedly thickened; deposits appear to be surrounded by newly formed BM (arrows).
Identify (be specific) (from Rosai & Ackerman).

MGN Stage IV. BM markedly irregular; deposits lysed, leaving large electron-lucent areas;
“moth-eaten appearance”
Identify (from Rosai & Ackerman).

MGN. (+) Peripheral GRANULAR deposits of IgG +/- C3.
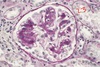
Identify (from trans).

Membranoproliferative GN - (+) mesangial cell proliferation, BM thickening, & leukocyte infiltration (top image); MPGN under IF (bottom image).
Identify A & B (from trans).

A - MPGN Type I.
B - MPGN Type II/”Dense Deposit Disease”
Identify (from Rubin’s, not Robbin’s haha)

FSGS (PAS stain). Note perihilar areas of segmental sclerosis and adjacent adhesions to Bowman’s capsule.
Identify (from Rubin’s).
FSGS in HIV nephropathy (silver stain).
Identify (from Rubin’s; don’t mind the number haha)

Membranous glomerulonephritis. Glomerulus slightly enlarged and shows diffuse thickening of capillary walls. No hypercellularity.
Identify (from Rubin’s)

Membranous glomerulopathy, Stage II (EM). Deposits of electron-dense material (arrows), with intervening projections of BM material.
Identify (from Rubin’s).

Membranous glomerulopathy (IF). (+) granular deposits of IgG outlining capillary loops.
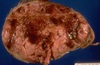
Identify (from Rubin’s).

Diabetic glomerulosclerosis (PAS stain). There is increase in mesangial matrix, forming several nodular lesions. Some capillary BM thickened, dilation of glomerular capillaries evident.
Identify (from Rubin’s).

Amyloid nephropathy.
Identify (from Rubin’s).

Amyloid nephropathy (congo red stain). Amyloid deposits show characteristic APPLE-GREEN BIREFRINGENCE.
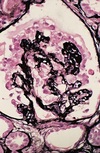
Identify (from Rubin’s).

Alport Syndrome (hereditary nephritis). Note “BASKET WEAVE” appearance - lamina densa of glomerular BM is laminated (arrows) rather than forming a single dense band.
Due to mutations in genes that encode Type IV collagen (alpha 3,4,5 chains).