Ophthalomolgy Flashcards
What is Non Arteritic anterior ischemic optic neuropathy (AION)?
Occlusion of the short posterior ciliary arteries resulting in infarction of the optic nerve head.
What are the risk factors for non arteritic AION?
Male Systemic ateriopathy 40-60yrs Small hypermetropic optic discs Hypertension Diabetes
What are the symptoms and signs of non ateritic AION?
Painless, monocular sudden loss of vision
Can be asymptomatic if good vision in other eye Moderate to severely reduced visual acuity in the affected eye
Swollen optic nerve with splinter or flame shaped haemorrhages
Relative afferent pupillary defect
Visual field defect - most common inferior altitudinal defect

How do you manage no arteritic AION and what is the prognosis?
Refer to ophthalmology - needs to exlcude GCA
R/V and treat all cardiovascular risk factors
Consider asprin
30% make substantial improvment
15-50% risk in other eye
Optic disc swellign resolves to leave optic disk pallor (loss of neural tissue)
What is another name for giant cell arteritis?
Arteritic anterior ischemic optic neuropathy - optic nerve is damaged as the posterior ciliary arteries are blocked by inflammation
How does GCA present?
Sudden loss of vision associated with headache
jaw and tongue claudication
tender scalp and temporal arteries
Loss of appetite and weight loss
symptoms of polymyalgia rheumatica
O/E: swollen optic disc and RAPD, flame shaped haemorrhages and cotton wool spots - retinal nerve fibre layer infarction
How do you manage giant cell arteritis?
Ophthalomology referal
bloods for ESR (>47)
High dose steroids - prednisolone 80mg/24hrs ASAP
Temporal artery biopsy
Describe the anatomy and physiology of the aqueous production of the eye
The CILIARY BODY - joins the iris to the choroid, it produces the aqueous humor and controls lens convexity
The ANTERIOR CHAMBER - the space between the cornea and the iris (shallower in the hypermetropic eyes as the eyes or smaller)
TRABECULAR MESHWORK - sieve like structure through which aqueous drains into the SCHLEMMS CANAL and out of the eye
The aqueous humour is produced and drained to maintain an appropriate intraoccular pressure.

What is the mechanism in acute angle glaucoma?
Failure of the aqueous humour to pass through the pupil and drain out through the trabecular meshwork.
Occurs when:
- the iris is pushed forward and blocks the meshwork
- the aqueous fails to pass through the pupil (a pupil block)
The result is raised intraoccular pressure
What are the risk factors for acute closed angle glaucoma?
Hypermetropia - eyes are normally smaller than usual and therefore have a shawllow anterior chamber which a narrower angle that is more prone to closure
Family history
Narrow anterior chamber angles
>30yrs - the lens thickens with age
Race - shallower angles in asians and eskimos
Women
What are the symptoms and signs of acute closed angle glaucoma?
Unilateral sudden loss of vision
Painful red eye
Halos around lights
Nausea and vomiting
O/E: corneal oedema, oval unreactive pupil, raised IOP
What is gonioscopy?
Uses prisms and a slit lamp to visualise the iridocorneal angle in 4 quadrants simultaneously
How do you treat acute angle glaucoma?
acetazolamide 500mg IV STAT - decreases the aqeous formation
timolol 0.5% and apraclonidine 1% eye drops - misosis opens the blocked drainage angle.
Laser - YAG peripheral iridotomy to create an alternative outflow tract for the aqueous to drain through
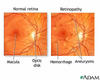
What is the anatomy of the retina?
Two main layers:
Neurosensory retina - in contact with the vitreous
The pigment layer - in contact with the choroid
The centre = the macula (5.5mm) and the fovea is the central area of the macula (high density of cones)
What are the different types of retinal detachment?
rhegmatogenous - a seperation of the vitreous layer causing a tear in the retina and detachment. The sensory retina separates from the retinal pigment epithelium
Tractional retinal detachment: secondary to intraocular problems - melanoma or fibrous bands in the vitroeous, seen in DM
post cataract surgery or trauma
What are the risk factors for retinal detachment?
MYOPIA - the higher the degree the higher the risk
previous retinal detachment in other eye
Trauma
What are the symptoms of retinal detachment?
Floaters, Flashes, Field loss, Fall in acuity
Usually field loss unless the macula is affected and then there will be a central loss of vision
How do you manage a retinal detachment?
REFER TO OPHTHALMOLOGY
the aim is to treat before the macula detaches.
Cyrobuckle surgery - silicome explant which indents the sclera to push back the retinal pigment epithelium against the retina and a cryotherapy probe to create a scar that seals the retinal break
Pars Plana vitrectomy - threet port pars plana cetrectomy involves removal of the vitreous, cryotherapy or laser to seal the break and then a bubble of gas to push the retina back against the retinal pigment epithelium.
Describe the visual pathway:
Nerve fibres from each retina leave the eye at the optic disc and travel along the optic nerve
The optic nerves of each eye join at the optic chiasm
Nerve fibres from the nasal retina of each eye cross over at the chiasm and travel down the contralateral optic tract
Nerve fibres from the temporl retina do NOT cross over so travel down the ipsilteral tract
The optic tracts connect with the lateral geniculate body. At this point synapses are formed with the neurones passing through the optic radiations to reach the visual cortex.

Describe the postion of lesions and what type of visual field defects they produce:

What is a homonymous hemianopia?
Field loss affecting the corresponding half fields of each eye. eg left homonymous hemianopia, the left side of the visual field is affected which means the right side of the visual pathway is damaged.
Must be posterior to the chiasm as the loss is bilateral.
Stroke is most common cause, others include tumours

What is a quandrantanopia?
Loss of a quarter of field of vision.
Bilateral to posterior to the chaism
Normally due to damage to the optic radiations.
A right homonymous inferior quadrantopia is due to lesion in the upper optic radiation in the left parietal lobe
What causes a bitemporal hemianopia?
Lesions in the optic chiasm
eg pituitary tumours - usually cause bi-temporal superior quadrantopia.
What causes central visual field defects?
Commonest cause = age related macula degeneration
Can be caused by optic nerve disease, often associated colour vision defects and visual acuity reduction