Ocular Anatomy & Clinical Correlation Flashcards
What are the two major pathologies we see in the lens?
- Presbyopia
- lose ability change the shape of the lens to allow for accomodation as we age
- Cataract
- cloudy as we age
The cornea is composed of what cell types?
Its stroma is composed of what types of collagen?
epithelium, stroma, endothelium
stroma: type I, IV, V collagen
What two structures are responsible for focusing light?
Relative percentages of each?
Cornea: 70%
Crystalline lens: 30%
What muscle is the main focusing muscle of the eye?
It is attached to what structes to accomplish this?
ciliary body
attached to & suspends the crystalline lens via zonules
What structure separates the anterior & posterior chambers?
crystalline lens
What structure has the highest concntration of protein in the body?
lens
The lens gets most of its energy through what process?
glycolysis
The “uvea” references what structures?
describe these components
- iris
- thin, colored portion
- helps to control size of pupil
- ciliary body
- main focusing muscle of the eye
- produces aqueous humor tha tbathes anterior chamber
- choroid
- deep to retina, highly vascular & provides most of the blood fow adn suport to retinal tissue
Where is the aqueous humor that bathes the anterior chamber produced?
ciliary body
What are the components of the vitrous?
It accounts for what percent of total eye volume?
sticky, jelly-like: type II collagen, hyaluronic acid, water
80%
What are the two major pathologies we see with the vitreous?
- Vitreous detachment
- Liquification as we age - leads to it separating from retina (50-60 yr)
- Retinal tears
- can potentially become retinal detachment during separation
What is it called where the conjunctive, cornea & sclera all meet?
limbus

What is the presentation of a patient with nasolacrimal duct obstruction?
Treatment?
- Presentation
- recurrent tearing and discharge in an infant
- Treatment
- warm digital massage over nasolacrimal sac
- typically resolves by 12 months - if not, opthalmologist can probe to open

What is the term for the fibrous layer beginning at the periosteum of the skull & extending to the eyelids?
orbital septum

What are the terms for an infection anterior to the orbital septum & posterior to the orbital septum?
- anterior - periorbital cellulitis
- posterior - orbital cellulitis
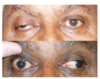
Presentation of a patient with periorbital cellulitis?
Treatment?
- Mild condition - common
- NO proptosis
- NO ophthalmoplegia
- LESS pain with eye movement
- NO vision loss
- Treatment
- antibiotics

Presentation of a patient with orbital cellulitis?
Treatment?
- Presentation - SERIOUS
- ophthalmoplegia
- pain with eye movement
- proptosis
- chemosis of conjunctiva
- coexistin rhinosiusitis (90%)
- Treatment
- IV antibiotics x3weeks
- frequently inpatient

What is the common cause of orbital cellulitis?
What complications can arise from orbital cellulitis?
- Cause
- spread from adjacent siunses (usually ethmoid)
- Complications
- cavernous sinus thrombosis
- meningitis
- cerebral, orbital, subperiosteal abscess
- vision loss

Identify the bones & indicated landmarks on the provided image


What bones make up the orbital roof?
frontal bone
lesser wing of the sphenoid
What bones make up the lateral wall of the orbit?
zygogatic bone
greater wing of the sphenoid
What is the thickest & strongest parts of the orbit?
lateral wall