Neuropsych Flashcards
1
Q
Depression Pathophysiology
A
- All antidepressants effect monoamine system and neurotransmitters (NT)
- Serotonin (5-HT), norepinephrine (NE), and/or dopamine (DA)
-
Monoamine Hypothesis: Decrease in function or amount of NT in the brain
- Treatment increases NT immediately, but effects on symptoms are delayed
-
Neurotrophic Hypothesis: Adaptive Changes to Amine Receptor Systems
- Desensitization or downregulation of receptors
- Disrupted Brain-Derived Neurotrophic Factor (BDNF)
- Growth factor protein that regulates differentiation & survival of neurons
2
Q
Antidepressant Classes
A
- Selective Serotonin Reuptake Inhibitors (SSRI)
- Fluoxetine has the most evidence to support its use in the adolescent population
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRI)
- Tetracyclic and Unicyclic Antidepressants
- Not Recommended in children:
- Tricyclic Antidepressants (TCA)
- Monoamine Oxidase Inhibitors (MAOI)
3
Q
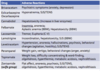
Receptors and Transporters
A
- ACh M: acetylcholine muscarinic receptor
- Anticholinergic effects (dry)
- H1: histamine1 receptor
- Sedation, HOTN, weight gain
- 5-HT2: serotonin 5-HT2 receptor
- Sedation, HOTN, sexual dysfunction
- Bleeding risk – impairment of platelet aggregation with serotonic-affecting agents
- NET: norepinephrine transporter
- NE reuptake inhibition: decreased depression, tremors, tachycardia, sexual dysfunction
- SERT: serotonin transporter
- Serotonin reuptake inhibition: decreased depression, anxiety, GI distress, sexual dysfunction
Affinity
- • 0/+, minimal affinity +, mild affinity
- • ++, moderate affinity +++, high affinity
4
Q
SSRI
A
- MOA - Inhibition of serotonin transporter (SERT)
- Many Treatment Indications - broad spectrum of use
- First line treatment option
- Safe in overdose
- Relative tolerability
- Consider variability within class
- Consider Drug Interactions
- Enhance serotonergic activity
- GI – n/v/d/GI issues (start early and improve with time)
- Diminished sexual function and interest
- 30-40% loss of libido, delayed orgasm, diminished arousal
- Headaches
- Insomnia, hypersomnia
- Excessive sleepiness or trouble staying awake during the day; can fall asleep at any time
- Weight gain (especially paroxetine)
- “Disinhibition” (risk-taking behaviors, increased impulsivity)
- Increase risk of bleeding
- Citalopram/Escitalopram – prolong QT interval
- SIADH and hyponatremia (Age, volume depletion, diuretic use)
- Prozac t1/2 48-72h; active metabolites t1/2 180 hours – longest
- Paxil t1/2 20-23h – shortest

5
Q
Serotonin-Norepinephrine Reuptake Inhibitors (SNRI)
A
- Similar serotonergic effects to SSRIs
- Increased risk of bleeding
- Noradrenergic effects: Dose-related hypertension; tachycardia
- CNS activation: insomnia, anxiety, agitation
- Increased sweating and urinary retention
- SIADH and hyponatremia (Risk factors - volume depletion, diuretic use)
- Increase risk of seizures
-
Duloxetine
- Hepatotoxicity; Hyperglycemia
-
Venlafaxine
- Dyslipidemia (Total cholesterol, TG)

6
Q
Tetracyclic and unicyclic
A
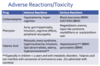
Tetracyclic & Unicyclic Adverse Reactions
-
Bupropion
- Improves sexual dysfunction; not sedating; no weight gain
- Agitation, insomnia, anorexia; hypertension
- Seizure risk especially in overdose
- Contraindicated in patients with seizure disorders & eating disorders
-
Mirtazapine
- Sedative effect; weight gain; sexual dysfunction
- Anticholinergic effects (dry mouth, constipation, orthostatic hypotension)
- Increased arrhythmias (QT prolongation, V Fib)
- Hyperlipidemia; hyponatremia

7
Q
Serotonin Syndrome
A
-
Overstimulation of 5-HT receptors
- Serotonin antidepressant + other serotonin medications
- (Linezolid; dextromethorphan, sumatriptan, tramadol, methadone, St. John’s wort)
- Triad of Symptoms
- Cognitive (delirium, coma) +
- Autonomic (hypertension, tachycardia, diaphoresis) +
- Somatic (myoclonus, hyperreflexia, tremor)
- Caution when switching from one serotonin antidepressant to another, especially Fluoxetine with longer t 1⁄2; allow 1-2 weeks washout period
8
Q
Antidepressant Discontinuation Syndrome/Withdrawal Syndrome
A
- Avoid abrupt discontinuation of antidepressant therapy
- Taper dose over several weeks with consideration to half-life
- Reduce dose every 5-7 days
- Longer duration for medications with shorter t1⁄2 • Fluoxetine taper may be unnecessary
- Long term therapy - taper over 4-6 months
- If symptoms occur during taper, restart at the original dose taper slower
- Especially if short half-lives; case reports with all drugs
- Differentiate from relapse of depression or other psychiatric/medical conditions
-
F.I.N.I.S.H. Mnemonic for recognition of symptoms
- Flu-like symptoms (general malaise, muscle ache, headaches)
- Insomnia
- Nausea - GI disturbances
- Imbalance - Dizziness/lightheadedness, vertigo
- Sensory disturbances - paresthesia, visual disturbance
- Hyperarousal - anxiety, agitation
- Symptoms resolve within 1-2 weeks; Not life-threatening
9
Q
AAP Recommendations – Selecting Therapy
A
First Line – SSRI
- Base selection on optimum combination of safety and efficacy data including drug interactions
- Deliberate self-harm and/or suicide risk is more likely if SSRI started at higher doses
- Only fluoxetine FDA approval ≥6yo for depression
- Also approved for depressive episodes associated with bipolar I disorder (in combo w/ olanzapine ≥ 10yo); and OCD ages ≥7yo
- Escitalopram only FDA approved >12yo for depression
- *Sertraline FDA approved ≥ 6yo for OCD
- Details regarding initial selection of specific SSRI and possible reasons for initial drug choice in GLAD-PC toolkit
10
Q
Selecting between SSRIs
A
- FDA approval for adolescents
- If no contraindications, fluoxetine recommended as first-choice • Success of prior medication trials
- SSRI half-life
- Interactions with other medications
- Side effect profiles of different medications
- Family history of successful medication treatment
- Patient’s medical issues
11
Q
AAP Recommendations – During Treatment
A
- Delayed improvements in symptoms
- Consider titrating dose after 2-3 weeks if no positive response noticed
- Reassess diagnosis/ initial treatment if no improvement noted after 6 to 8 weeks and consider mental health consultation
- < 50% of patients respond to 1st line therapy
- Maintain therapy for 6 to 12 months after full resolution of depressive symptoms
- Regardless of length of treatment, monitor all patients on a monthly basis for 6 to 12 months after full resolution of symptoms
- If patient experiences a recurrence, clinicians are encouraged to monitor patients for up to 2 years given high rates of recurrence
- Switch within a class before switching to another class

12
Q
ADHD
A
- Eval for ADHD for any child 4-18yo presenting with academic or behavioral problems and symptoms of inattention, hyperactivity, or impulsivity
- Pre-school: EBP behavior therapy first; methylphenidate if not improved
- Elementary: drug and/or behavior therapy, preferably both
- Evidence stronger for stimulant medications and sufficient but less strong for atomoxetine, extended release guanfacine, and extended release clonidine (in that order)
- Adolescent: drug and/or behavior therapy, preferably both
- ER formulations more expensive, but benefits of consistent & sustained coverage with fewer administrations, better adherence
- Some adolescents, might require > 12 hours of coverage: utilize a short-acting might be used in addition to long-acting
- Identify risk factors for Stimulant Medications
- History of cardiac symptoms; cardiac family history (arrhythmias, sudden death, death at young age from cardiac conditions); vital signs, cardiac physical examination
- Presence of tic disorder: affects ~20% of patients with ADHD
- Stimulant medication does not clearly worsen tics, may do so in individual cases. Atomoxetine or alpha-agonist may lessen comorbid tics.
- Minimization of adverse effects
- Affect on sleep initiation
- Risk status for drug use/abuse
13
Q
AAP Recommendations – Initiating ADHD Therapy
A
- Begin with low dose and titrate to dose that provides maximum benefit and minimal adverse effects
- During 1st mo of trx, titrate weekly/biweekly via discussions w parents
- Stimulant medications can be effectively titrated on a 3 to 7 day basis
- In-person follow up recommended by 4th week of therapy
- Initially, core symptom reduction is more likely to indicate medication effects
- Effects of improvement in function require more extended time period
- If max dose reached without satisfactory results or intolerable effects, switch to another stimulant before attempting non-stimulant
14
Q
Stimulant Medications
A
Methylphenidate or amphetamine compounds
- MOA: Affect CNS dopaminergic pathways
- First choice of treatment
- > 70% of children and youth with ADHD respond to 1st stimulants at an optimal dose; 90-95% respond to 2nd stimulant
- Highly effective for most children in reducing core sx of ADHD
-
ADME Consideration:
- Children 4-5 years of age have slower rates of metabolizing methylphenidate, initiate a lower dose and increase in smaller increments
- AE: generally dose dependent
- Most Common AE
- Appetite loss, abdominal pain, headaches, and sleep disturbances
- Decreases growth velocity (~1-2 cm)
- Esp in higher, consistently administered doses
- Effects decrease by 3rd year of trx
- Uncommon: hallucinations and or psychotic symptoms
- Rare occurrence of sudden cardiac death; depression, suicidal ideation
- AE in preschool-age children – increased mood lability and dysphoria
15
Q
Non-stimulant Medications for ADHD
A
- First choice of treatment if concerns about possible abuse/diversion or strong family preference against stimulant medication
- Take longer to reach efficacy
Atomoxetine
- May also be effective for comorbid mood or anxiety disorders and has no abuse risk
Guanfacine and Clonidine
- Also beneficial as alternatives or adjuncts to stimulant treatment
- Useful in combination with stimulants for comorbid sleep problems, tics, or Tourette syndrome
- Potential advantages of guanfacine over clonidine include fewer sedative and hypotensive effects