Neurology Flashcards
Seizure Pathophysiology
- *“Good” transmitters** which reduce seizures (2) - drugs potentiate these
- *“Bad” transmitters** which increase seizures (4) - drugs block these
Good - K channels, GABA
Bad - Glutamate, AMPA, NMDA, Na channel
Gerstmann Syndrome
Anatomical Location
Features (5)
Angular gyrus of the lower dominant parietal lobe
-associated with posterior circulation stroke
Features
- Agraphia
- Constructional apraxia
- Acalculia
- Left/Right dissociation
- Finger agnosia
TPA in acute stroke - indication and contraindications

Treatment of choice for trigeminal neuralgia
carbamazepine - 100mg BD to TDS, works within a few days

Auto-antibody of Lambert Eaton Myasthenic Syndrome
Anti- Voltage Gated Calcium Channel
Rate of congenital abnormalities in women taking AEDs
and
Advice re folic acid
Rate: 4 - 6%
Approximately double the national average of women without epilepsy
Folic acid
5mg daily for at least 3 months before and after conception
Both hemicrania continua and paroxysmal hemicrania both respond 100% to
Indomethacin!
This is the diagnostic criteria
Sydenham Chorea
- causative infection
- first line AEDs
- What else should the patient be on?

Pharmacological management of Tics

Glial cells
Oligodendrocytes are what is lost/defective in MS

Types of nerve fibres

Brown Sequard Syndrome

Pathogenesis of GBS
-most common preceeding infection

GBS: Presentation

Prognosis of GBS

Atypical degenerative causes of Parkinsonism: PSP

Atypical degenerative causes of Parkinsonism: MSA
triad of: autonomic failure, parkinsonism and cerebellar signs
*autonomic failure does not present so early on in disease of PD whereas in MSA they can develop autonomic failure and orthostatic hypotension quite early on

Atypical degenerative causes of Parkinsonism: CBA
Alien hand!

Braak Stages of PD
Risk factors and Protective Factors for Parkinson’s Disease

Treatment Options/Principles in PD
- While medications improve motor and non-motor symptoms, they do not improve balance

Treatment of Other Aspects of PD

Management of Essential Tremor

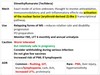
- *Carbamazepine**
- mechanism
- use
- contraindications (4)
- pregnancy?
- HLA we test for, who is more likely to have it
- HLA we don’t test for