Neuraxial Anesthesia & Local Anesthetic Dosing Flashcards
Lance Carter, CAA
Descent of the Spinal Cord & Dural Sac

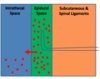
Neuraxial Anatomy
(Layers From Skin to CSF)

Spinal Vertebrae

Spinal Nerve Roots

Nerve Roots


Spinal/Epidural Landmarks

Finding The L3-4 Landmark

T10 (Umbilicus) Dermatome

T4 (Nipple) Dermatome


T5-L1 (Vasomotor Tone) Dermatome

T5-L1 (Vasomotor Tone) Dermatome (Cont’d)

T1-T4 (Cardiac Accelerator Fibers) Dermatome

C3-C5 (Phrenic Nerve) Dermatome

C6-C8 (Hands/Fingers) Dermatome

C6-C8 (Hands/Fingers) Dermatome (Cont’d)

Other Neuraxial Dermatomes

Sympathetic vs. Sensory vs. Motor Blockade

Sympathetic Blockade

Nerves are more easily blocked if they are:

Differential Blockade

Epidural

EpiduralAdvantages
(Compared To Spinals) (4)

EpiduralDisadvantages
(Compared To Spinals) (2)

EpiduralDisadvantages
(Compared To Spinals) (3-4)